All published articles of this journal are available on ScienceDirect.
A Novel Minimally Invasive Technique for Treatment of Unicameral Bone Cysts
Abstract
Management of unicameral bone cysts (UBC) remain controversial. These cysts seldom heal spontaneously or even after pathological fracture. Sometimes these cysts can be very large and incredibly troublesome to the patient. Various treatments exist with variable success rates. We present our experience of treating these lesions by continuous drainage. Over a seven year period, six patients with unicameral bone cysts were treated by inserting a modified drain into the wall of the cyst. The aim of surgery was to place the drain in a dependent area of the cyst, through the cortex allowing for continuous drainage. This was achieved through a small incision under radiographic control. A cement restrictor (usually used for femoral canal plugging during total hip replacements) was modified and inserted to prevent closure of the drain site. A redivac drain was passed through the plug into the cyst. The drain was left in place for a week to establish an epithelialized pathway which hopefully would remain patent, into the subcutaneous tissues, after the drain had been removed. There were four males and two females in the group and the age range was 6 -12 years. Four of the lesions were in the upper humerus, one in the proximal femur and the other one in the proximal tibia. Healing was rated according to the modified Neer classification. Grade 1 (healed) and Grade 2 (healed with defect) was defined as excellent outcome. Persistent /Recurrent cysts (Grade 3 and 4) were noted as unsatisfactory. Five cases were completely healed. Only one had a further fracture and there were no recurrent fractures. All the patients reported complete comfort and they all were able to re-engage in recreational activities without restriction. We think that reducing the intra-medullary pressure in these lesions will lead to healing. We report a safe and minimally invasive technique for the management of UBC.
INTRODUCTION
Unicameral bone cyst (UBC) or simple bone cyst is a solitary [1] benign fluid-filled lesion that usually involves the metaphyseal-diaphyseal region of growing long bones [2, 3]. The majority of cases occur in the first two decades of life [4]. The common sites of occurrence are proximal humerus followed by proximal femur. Less common sites are tibia and fibula, calcaneum, radius and ulna [5].
Clinically, most lesions are asymptomatic. Pathological fractures can occur through the thin cortex. They can be a cause of significant morbidity when recurrent fractures necessitate prolonged limitation of physical activities [6]. Physeal injury may occur secondary to direct cyst expansion, leading to growth disturbance and skeletal deformity. Although some authors suggest that 25% of cysts heal spontaneously following a pathological fracture [7], others believe that UBC’s seldom heal spontaneously or even after pathological fractures [8]. They are known to have a high rate of persistence and recurrence [9]. Whilst no treatment isneeded for small asymptomatic cysts, larger cysts with thinner cortices, especially in weight bearing bones, usually need intervention to prevent fractures. Several methods of treatment have been used which include minimally invasive and open procedures [10].
We describe a new technique for treatment of unicameral bone cysts using a modified cement blocker and a drain. This technique allows for continuous drainage of UBC. Clinical and radiological outcomes are reported.
MATERIALS AND METHODS
Over the last seven years, six patients (four males and two females) with unicameral bone cysts were treated using a minimally invasive technique following Institutional Review Board approval. The mean age was 9.8 years (range 6-12 years). The UBC was located in the proximal humerus in four (67%), and in proximal femur and proximal tibia in the other two patients. Diagnosis was established by biopsy in all cases. Three patients had pathological fractures of the affected bone prior to treatment. Two patients had fractures more than once before commencing treatment.
The surgical procedure was performed under general anaesthesia. The image intensifier was used as needed. A 4.5mm hole was drilled in the thinnest part of the cortex of the cyst through a small longitudinal skin incision. The contents of the cysts were aspirated and the cell lining was curetted. A JRI (Joint Replacement Instrumentation Ltd, London, UK) cement restrictor (usually used in total hip arthroplasty) was modified by truncating and drilling and inserted through the fenestration acting like a grommet.
Intracystic fluid drainage was maximised by the use of a Redivac® drain. The tip of the drain tube was passed through the cement blocker into the cyst cavity. The drain was left for a variable amount of time ranging from five to nine days. All procedures were performed by the senior author (JKT). If the cyst was multi-loculated or a separate cyst existed, an additional cement blocker was introduced using the same technique (Fig. 1).
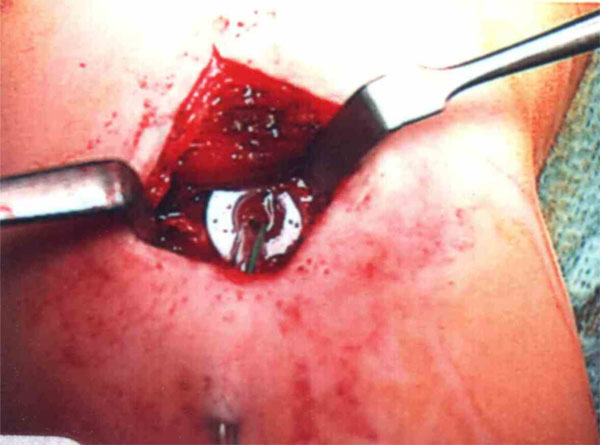
Intraoperative picture of the plug with the Redivac® drain in situ.

Serial plain AP radiographs of a unicameral bone cyst (UBC) in a proximal tibia of a 12 year old boy at 0, 3 & 12 months postoperative respectively from left to right.

Serial plain AP radiographs of a humerus of another patient showing a large UBC treated with our method at 0 month, 3 months and 5 years postoperative respectively from left to right.
Demographics and treatment outcomes of our 6 cases treated with this method. The drainage duration was defined as the number of days the drain has been left in situ. Cortical thickness was measured across the thinnest part of the cyst. Cysts were define.
| Case | Age (Yrs.) |
Location | Presenting Complain |
Single/ Multi- Loculated |
Previous Treatments |
Drainage Duration (Days) |
Cyst Ratio |
Cortical Thickness Pre-Rx mm |
Cortical Thickness Post Rx mm |
Activity | Outcome Grade |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 12 | Humerus | 4 prior fractures |
Multi | Prednisolone injections |
9 | 1.56 | 0.55 | 1.6 | active | I |
| 2 | 10 | Humerus | Pain | Multi | BM injection |
8 | 1.27 | 0.53 | 1.2 | active | II |
| 3 | 6 | Humerus | Fracture | Single | Nil | 8 | 2.55 | 0.7 | 2 | inactive | I |
| 4 | 7 | Femur | Pain/limp | Single | Cannulated Screws |
7 | 1.29 | 0.4 | 2.5 | inactive | I |
| 5 | 12 | Tibia | pain/limp | Single | Nil | 8 | 0.93 | 0.6 | 4 | active | I |
| 6 | 12 | Humerus | 2 prior fractures |
Multi | Cannulated screws |
5 | 2.92 | 0.27 | 0.7 | active | II Fractured |
An example of the several recognised methods for treatment of unicameral bone cysts.
| Author | Method |
|---|---|
| Fahey & O'Brien 1973 | Subtotal resection and grafting |
| Scaglietti 1974 | Multiple Steroids injection |
| Spence 1976 | Curettage & cortical bone allograft. |
| Catier 1981 | Intra-medullary nails. |
| Chigira 1983 | Multiple drill holes |
| Thawrani 2009 | Single percutaneous injection of α-BSM |
| Hunt 2009 | percutaneous decompression, curettage,& cancellous allograft with autologous bone marrow |
| Hou 2010 | Curettage, ethanol cauterization, bone graft & cannulated screws |
All procedures were performed as a day cases. A follow-up appointment was given for one week and two weeks to assess cyst drainage and to remove the drain. The cement plug was removed after healing of the cyst only if it was causing symptoms or on patient request.
Clinical and radiological evaluation of treatment outcome was performed at regular intervals at 6 weeks, 3, 6 and 12 months then annually. All patients had follow-ups for a minimum of 1 year (range 1-7 years). The average follow up was 4.3 years (range 2-6 years). The mean duration of drainage was 7.5 days (range 5-9 days). Postoperative Clinical assessment was performed and patients were asked to complete a questionnaire reporting their pain score, physical activity and overall satisfaction. Radiological assessment was performed according to the classification described by Chang et al. [9] (Figs. 2, 3); grade I (healed), grade II (healed with defect), grade III (persistent), grade IV (recurrent). Failure was defined as recurrent fracture, need for further intervention or radiographic evidence of persistent or recurrent cysts (grade II and IV).
RESULTS
Clinically all patients reported complete pain relief were able to return to full activity level engaged in recreational activities without restriction of 6 months after the start of treatment. No intraoperative or perioperative complications were reported. One patient experienced some pain over the plug site of 3 years postoperatively. Following removal of the plug, the patient was asymptomatic. Patient/Parent satisfaction was 100%
Radiographically four cases showed complete healing (grade I), and two cases had healing with defect (grade II). There were no cases with persistent or recurrent cysts. In three cases the cysts were multi-loculated and in the other three they were simple. The mean cyst ratio was 1.75 (range 0.93-2.92). The cortical thickness improved by an average of 1.49mm (range 0.43-3.3mm), details of pre and post-treatment cortical thickness is provided in Table 1 for all cases. One case (grade II) sustained a fracture and therefore the outcome was considered as a failure. The details of all cases are provided in Table 1.
DISCUSSION
The aetiology and pathogenesis of UBC is still unclear and hence treatment is controversial. Several hypotheses for the pathogenesis of UBC have been advocated: cystic resorption of a traumatic haematoma or pre-existing benign tumour [5], entrapment of a synovial cyst in an intraosseous position during early growth or secondary to trauma at birth [11], and failure of ossification in a localized metaphyseal area are possible mechanisms.
The search for the best treatment method of unicameral bone cyst is still an on-going process. Since Virchow described this lesion in 1876, several treatment modalities have been described with a varied success rates and a variable criteria for successful outcome (Table 2). An ideal treatment method should be effective, safe, has a high healing and low of recurrence rate and lower complication rate. Minimally invasive techniques; intra-lesional steroid injection [12], percutaneous injection of apatitic calcium phosphate [3] and demineralised bone matrix [13] have been used with variable success rates. More invasive techniques include subtotal resection and grafting [14], open curettage and grafting with autogenous or allogenous bone [15, 16] and hydroxyapatite [17].
Obstruction of intra-medullary venous drainage is one of the most widely accepted mechanisms of formation of UBC’s first described by Cohen in 1960 [18]. The hypothesis was based on the fact that intracystic fluid pressure is higher than the intra-medullary pressure of a contra-lateral normal bone [19]. The increased pressure leads to slow bone resorption, cyst expansion and cortical thinning. Based on this hypothesis, a variety of treatment methods have been use over the years. Percutaneous drilling (trepanation) [19], continuous decompression using intra-medullary nails [20], cannulated screws [21]. In an effort to increase the free drainage of the intra-cystic pressurized fluid, we used a Redivac® drain which was passed through the modified cement restrictor into the cyst cavity. The amount of fluid drained postoperatively was considerable which supports the hypothesis of increased intra-cystic fluid production. By establishing a patent tract, a continuous drainage of the intra-cystic fluid will enable healing of the cyst.
The main goal of treatment is to prevent pathological fractures and to provide a good quality of life without any restriction of activities. Whilst the results of other minimally invasive techniques (percutaneous aspiration and injections) are variable, one should try to use the least invasive method as much as possible especially in younger children.
The described method is minimally invasive, can be performed as a day case procedure and is associated with minimal morbidity. The material that is used for this treatment is readily available in orthopaedic theatres, the technique is safe and easy to learn and removal of the restrictor is not problematic if needed. All patients were satisfied with the treatment they received. The success rate was 83% and there were no further cases of pathological fractures at latest follow up. Unlike injections which might require 2-5 treatment episodes, this method allows for a ‘one off’ procedure that allows for continuous drainage of the cyst into the subcutaneous tissue. We believe that this is an effective and minimally invasive technique that can be used even in recurrent multi-loular cysts before embarking on an open procedure. There was no reported pain or functional limitations and all patients were able to return to their full physical activity. One case that sustained a fracture, the cyst was large, occupying almost half of the humerus, multi-loculated and was previously treated with two cannulated screws.
We report a simple novel technique which allows for treatment of simple bone cysts by continuous drainage. This minimally invasive procedure was successful in treatment of five out of six patients. The procedure can be performed as a day case procedure and can be considered as another treatment option when managing unicameral bone cysts.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


