RESEARCH ARTICLE
High Rates of Postoperative Wound Infection Following Elective Implant Removal
M Backes*, 1, 2, N.W.L Schep 1, J.S.K Luitse 1, J.C Goslings 1, T Schepers1
Article Information
Identifiers and Pagination:
Year: 2015Volume: 9
First Page: 418
Last Page: 421
Publisher ID: TOORTHJ-9-418
DOI: 10.2174/1874325001509010418
Article History:
Received Date: 19/11/2014Revision Received Date: 24/6/2015
Acceptance Date: 5/8/2015
Electronic publication date: 31/8/2015
Collection year: 2015

open-access license: This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
Abstract
Introduction :
Metal implants placed during fracture surgery are often removed for various reasons (i.e. pain, prominent material, patients request). The removal of implants is considered a ‘clean’ procedure and as low risk surgery. The incidence of wound infections following implant removal has received little attention in the literature. The aim of the current study was to assess the incidence and risk factors of postoperative wound infections (POWIs) following implant removal.
Material and Methods :
All consecutive adult patients in a Level 1 and Level 2 Trauma Center who had their implants removed during a 6.5 years period were included. Exclusion criteria were removal of implants because of an ongoing infection or fistula and removal followed by placement of new implants. Primary outcome measure was a POWI as defined by the US Centers for Disease Control and Prevention. Patient characteristics and peri-operative characteristics were collected from the medical charts.
Results :
A total of 452 patients were included (512 procedures). The overall POWI rate was 11.6% (10% superficial, 1.6% deep). A total of 403 procedures (78.7%) comprised of implant removal below the knee joint with a 12.2% POWI rate. A POWI following initial fracture treatment was associated with a higher rate of POWI following implant removal (p=0.012). A POWI occurred more often in younger patients (median age 36 versus 43 years; p=0.004).
Conclusion :
The overall incidence of postoperative wound infection was 11.6% with 10% superficial and 1.6% of deep infections in patients with elective implant removal. A risk factor for POWI following implant removal was a previous wound infection.
INTRODUCTION
Implants are used to stabilize fractures and are often removed at a later stage for various reasons. Indications for implant removal mainly consist of pain, functional impairment, prominent material or at patients request [1]. Removal can result in pain relief, improvement in function and a high rate of patient satisfaction [2, 3]. Implant removal is a frequently performed procedure and it accounts for up to 29% of all elective surgery and 6.3% of orthopedic surgical interventions [4].
Antibiotic prophylaxis is administered prior to placement of implants in order to lower the rate of postoperative wound infection (POWI) [5]. However, it is not a common practice to administer antibiotic prophylaxis before implant removal. This is because, according to the Centers for Disease Control and Prevention classification of surgical wounds, implant removal is considered as a ‘clean’ procedure [6]. The effect of pre-operative antibiotics are disputed in clean wounds, as there is lack of evidence that they decrease the rate of POWI of 2% [6].
Remarkably, in contrast to literature on infectious complications following elective fracture surgery such as open reduction and internal fixation, there is a paucity in the literature on rates of POWI following implant removal (Table 1) [2, 7-13].
The aim of the current study was to assess the incidence of postoperative wound infection following elective implant removal in a Level 1 and Level 2 Trauma Center and to evaluate possible risk factors.
MATERIAL AND METHODS
We conducted a retrospective cohort study of all consecutive adult orthopedic trauma patients in two hospitals (Level 1 and Level 2 Trauma Center) who had their implants removed following fracture healing. The electronic hospital databases were searched from 2007 to 2012 for all procedures with implant removal using the appropriate surgical procedure coding reference. The start of the inclusion period coincided with the introduction of electronic medical charts.
We excluded patients with implant removal because of an ongoing infectious complication (persistent infection or chronic plate fistula) and patients with removal as part of a new procedure (e.g. non-union) from the analysis.
Patient-characteristics (gender, age, BMI, ASA-classification, type of fracture) and peri-operative characteristics (time interval from index procedure to implant removal, surgical experience (senior or resident), duration of surgery, administration of antibiotic prophylaxis and type of wound closure (subdivided into intra- and transcutaneous) were obtained from the electronic charts.
Patients were seen within four weeks postoperatively in the outpatient clinic where a wound inspection was performed. The primary outcome, POWI, was subdivided in superficial or deep by applying the criteria of the US Centers for Disease Control and Prevention [6]. A POWI was considered superficial if amendable for treatment with oral antibiotics and was considered as deep when treated with intravenous antibiotics or surgical wound debridement. Bacterial cultures were obtained postoperatively in the surgical ward or in the outpatient clinic and were recorded. They were collected on suspicion of a POWI (dry swab). The occurrence of wound dehiscence was documented, which was diagnosed by wound inspection or a negative culture.
Patient and peri-operative characteristics were compared between patients with and without POWI.
Statistical Analysis
Data were analyzed using Statistical Package for the Social Sciences (SPSS) version 17.0 (SPSS, Chicago, Illinois, USA). Normality of continuous data was tested by inspecting the frequency distributions (histograms). Descriptive analysis were performed to compare baseline characteristics between patients with and without POWI. For continuous data mean SD (parametric data) or medians and interquartile ranges (non-parametric data) were calculated. Differences between the two groups of patients with and without POWI were assessed using the Student’s T-test (parametric data) or the Mann-Whitney U-test (non-parametric data). Categorical data were compared using the Chi-square test. A p-value <0.05 was taken as the threshold of statistical significance.
RESULTS
A total of 452 patients with 512 procedures were included. Patient- and perioperative characteristics are presented in Table 2.
Ten percent of patients (N=51) suffered from a superficial POWI and 1.6% (N=8) from a deep POWI. Of these eight patients one patient was treated with intravenous (iv) antibiotics. Seven patients were treated with iv antibiotics and surgical debridement. One of these patients was treated with surgical debridement three times. Forty-one of 51 patients with superficial POWI were treated with oral antibiotics. A wound dehiscence occurred in 37 patients (7.2%).
In 51 patients (10.2%) iv antibiotic prophylaxis was administered prior to implant removal. Five of these patients (9.8%) developed a POWI, which were all superficial infections. Unfortunately, the reason for administration of antibiotic prophylaxis was not routinely documented.
Seventy-three procedures (14.3%) were performed in the upper extremity with four POWIs (5.5%) versus 439 procedures in the lower extremity (85.7%) with 55 POWIs (12.5%) (Fig. 1). Given the current number of patients surgery performed in the lower extremity was not significantly associated with an increased risk of POWI (p=0.151).
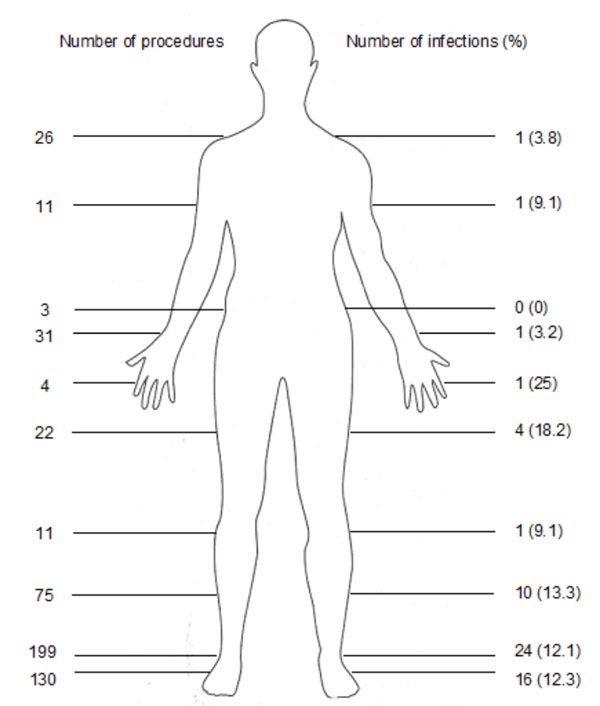 |
Fig. (1). The number of implant removals per body part (left) and the corresponding number and rate of postoperative wound infections (right). |
Current literature on implant removal and the incidence of postoperative wound infection.
| Study (Year) | N Patients | N POWI (%) |
|---|---|---|
| Raahave (1976) [7] | 269 | 7 (3.2) |
| Richards (1992) [8] | 88 | 0 (0) |
| Sanderson (1992) [9] | 188 | 27 (14.4) |
| Minkowitz (2007) [10] | 60 | 0 (0) |
| Pot (2011) [11] | 80 | 16 (20) |
| Wadia (2012) [12] | 27 | 0 (0) |
| Williams (2012) [2] | 69 | 2 (2.9) |
| Vos (2013) [13] | 284 | 23 (8) |
N; Number, POWI; postoperative wound infection.
Patient- and perioperative characteristics with statistical association on postoperative wound infections following implant removal.
| N Implant Removal of 512 (%) | N POWI (%) | p-Value (Two-Sided) | |
|---|---|---|---|
| PATIENT CHARACTERISTICS Male (N) Age in (years) BMI ASA-classification** I II III Diabetes Mellitus POWI following index procedure PERI-OPERATIVE CHARACTERISTICS Weeks to implant removal Resident performing procedure Duration of surgery (minutes) Antibiotic prophylaxis Transcutaneous wound closure |
287 (56.1) 42 (31-54)* 25 (22-28)* 370 (72.3) 130 (25.4) 11 (2.1) 15 (2.9) 71 (13.9) 49 (25-78)* 299 (60.4) 40 (26-60)* 51 (13.6) 226 (69.1) |
41 (14.3) 36 (25-49)* 26 (22-30)* 43 (11.6) 14 (10.8) 1 (9.1) 1 (6.7) 15 (21.1) 53 (34-85)* 43 (14.4) 46 (30-72)* 5 (9.8) 34 (15) |
0.130 0.004 0.336 1.000 NA 0.014 0.280 0.551 0.070 0.911 0.868 |
N; Number, POWI; postoperative wound infection, NA; not available.
*Median with interquartile ranges.
** (Chi2) difference in between ASA I and II+III.
Fifteen of 71 patients (21.2%) with a POWI following the index procedure developed a POWI following implant removal versus 44 patients following 381 uncomplicated procedures (11.5%) (p=0.014). Cultures were taken in 10 of these 15 patients, of which half showed the same micro-organism; a Staphylococcus aureus.
A POWI occurred more often in younger patients with a median age of 36 against 43 without a POWI (p=0.004). No association was found with gender, BMI, ASA-classification, smoking, diabetes mellitus, duration to implant removal, surgical experience or type of wound closure (Table 2).
DISCUSSION
Rates of POWI following implant removal from the upper and lower extremity in the current studies were 5.5% and 12.5%, respectively. These rates are consistent with rates in a recent prospective study of 6% and 10% [13]. Other retrospective studies show POWI rates of 9.2% following syndesmotic screw removal and 19% following calcaneal implant removal [14, 15]. However, overall a lower POWI rate than 11.6% is reported in literature (Table 1).
The high rate in the current study might be the result of the relatively high number of lower extremity surgery (85.7%) compared to upper extremity surgery (14.3%). In the foot and ankle region the bones are more prominent due to the limited soft tissue coverage (as compared to other bones with extensive muscle coverage). For example, after plating of the fibula in ankle fractures the plates are removed in about 27-36% of patients and following a calcaneal fracture almost 50% of patients have their implant removed [11, 16-18].
Remarkably, when looking at POWI following elective orthopedic surgery lower rates (0-5.4%) are found compared to implant removal [5, 19-28]. This might be the result of the instant use, full range of motion and weight-bearing of a limb following implant removal compared to fracture surgery, when patients are asked to build up exercise. In addition, it is a secondary procedure through scar tissue.
Importantly, the occurrence of POWI following fracture surgery was associated with the occurrence of POWI following implant removal. This information might be of help to the clinician or patient in decision making on implant removal.
Our results show that relatively younger patients are more susceptible to a POWI. This could be a result of a higher level of activity or earlier motion of younger patients compared to older patients. Earlier motion is associated with an increased risk of wound infection [29].
Finallly, in 10.2% of patients antibiotic prophylaxis was administered preoperatively. This was most likely the result of the surgeon’s preference. This missing information is a drawback inherent to the retrospective character and the main limitation of the current study.
In conclusion, the incidence of POWI following implant removal in a Level 1 and Level 2 Trauma Center is 11.6%. Risk factors for POWI following implant removal are a previous infection after initial fracture management and younger age. The results of the current study will be used in a prospective study on the effects of antibiotic prophylaxis prior to implant removal on a POWI (www.clinicaltrials.gov).
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.
COMPLIANCE WITH ETHICAL REQUIREMENTS
The current study was approved by the hospital review board and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.







