All published articles of this journal are available on ScienceDirect.
Ten-Year Results of Primary and Revision Condylar-Constrained Total Knee Arthroplasty in Patients with Severe Coronal Plane Instability
Abstract
Objective :
To retrospectively review the results at minimum ten years after surgery of a consecutive series of total knee arthroplasties (TKAs) performed using a constrained condylar implant in patients with severe coronal plane instability.
Materials and Methods :
The series comprised of 44 patients (45 knees) who received primary (19 knees) or revision (26 knees) TKA with a constrained condylar implant between 2001 and 2003 at a single institution.
Results :
There were no revisions or any other surgery related complications at a mean implantation time of 11.0 years. In 38 patients (15 knees in the primary group and 24 knees in the revision group) who were available for clinico-radiographic follow-up at a minimum of ten years, there was no sign of radiographic loosening. Two patients showed cortical hypertrophy at the extension stem tip but none complained of pain around the stem tip.
According to the TLKSS score grading, 73% of the patients in the primary group had results categorized as good or excellent, while 54% of the patients in the revision group had fair results. Four patients (one (7%) in the primary group and three (13%) in the revision group) had poor results. The median WOMAC Index was 80.2% (interquartile range: 74.0% - 81.2%) and 74.0% (interquartile range: 72.1% - 75.8%) in the primary and in the revision groups, respectively (p=0.010).
Conclusion :
This study showed satisfactory clinical outcomes with no re-operations at minimum ten years after implantation in patients who had undergone primary or revision TKA with a condylar constrained implant.
INTRODUCTION
In total knee arthroplasty (TKA) severe coronal plane instability of the knee is difficult to balance with a cruciate-retaining (CR) or a posterior-stabilized (PS) implant [1]. In such conditions, a ‘constrained condylar knee’ (CCK) implant is preferred [1]. CCK implants are, in fact, characterized by a large and tall tibial intercondylar eminence, which fits closely into a deep femoral box, to provide a high degree of rotational constraint [2, 3] and, more significantly, to increase knee stability in the coronal plane [1].
Although CCK implants are mainly used in revision TKA, they are also used in primary TKA: most suitable candidates to receive CCK implants are patients with severe varus/valgus deformity or capsule-ligament instability and patients with rheumatoid arthritis, who have a tendency for generalized ligamentous laxity and joint deformity [1]. On the contrary, in patients suffering from severe flexion/ extension instability, or with no soft tissue support or with massive bone loss, a linked hinge implant is preferred [2-4].
As documented in the literature, the pros of using implants with increased constraint should be weighed against the higher risks of: tibial post wear caused by tighter fit between the spine and the cam, possibly leading to osteolysis [5], and mechanical loosening of implant caused by the higher transmission of the varus/valgus stress to the bone/cement interface [2, 5]. In order to reduce the risk of implant loosening, modern CCK implants feature modular cemented or uncemented extension stems, for both the femoral and the tibial components, to transfer a part of the load to the intramedullary canal [1, 6].
As for many other implanted designs, potential failure modes leading to re-operation have been reported also for CCK implants:
- polyethylene (PE) insert disengagement from the tibial baseplate [7, 8];
- breakage of the tibial intercondylar eminence of the insert [9];
- fracture at the stem-condylar junction [10];
- loosening of the locking screw at the junction between the stem and the femoral component or femoral stem disengagement [11-15].
In addition, the benefit of using extension stems should be balanced against the fact that, in case of implant revision, the stem needs to be removed (with a removal more difficult in case of cemented fixation) [6]. Finally, pain around the tip of the extension stems has also been documented [16].
Although several studies have reported clinical outcomes for either primary CCK TKA [5, 17-19] or revision CCK TKA [16, 20-22], little is known about the long-term performance of these procedures.
Therefore, the objective of the present study was to assess the implant survival performance and the clinical outcomes at minimum ten years of TKAs performed with one CCK implant type at a single institution in either the primary or the revision settings.
MATERIALS AND METHODS
In December 2013, using the Institution joint registry, all the patients who received total knee arthroplasty surgery with a CCK implant, the NexGen LCCK (Zimmer Inc., Warsaw, IN, USA), at least 10 years prior to the study start, were identified to constitute the cohort of the present study. They were contacted by phone and asked to come to the hospital for a follow-up visit.
In total, the cohort comprised of 44 consecutive patients (45 knees) who were operated between March 2001 and October 2003. There were 19 primary TKAs (here defined as the ‘primary group’) and 26 revision TKAs (here defined as the ‘revision group’). Patients included 36 women (one woman received a primary TKA in one knee and a revision TKA in the other knee) and eight men. The mean age at the time of surgery was 69 ± 10 years (range: 43 - 82 years) in the primary group and 72 ± 7 years (range: 56 – 85 years) in the revision group.
The main indications for implanting a CCK implant were ligament loosening, severe varus/valgus deformity and, in case of revision TKA, sever bone loss/bad bone quality.
Preoperative diagnosis in the revision group included five cases (19%) of infected TKA, seven cases (27%) of aseptic loosening of ‘unicompartmental knee arthroplasty’ (UKA) and 14 cases (54%) of TKA aseptic loosening (Table 1).
Operative Information
A single surgeon (the author A.C.) performed all TKAs. The medial para-patellar approach was used. The surgical technique included the ligament gap-balancing described by Insall [23]. Seven knees in the revision group sustained anterior tibial tubercle osteotomy for a better exposure. Patellas showed mild to moderate osteoarthritic changes in the primary group, while there were no lytic alterations that were macroscopically visible during surgery in the revision group. The patella was never replaced nor resurfaced in any knee. The femoral and the tibial implant components were cemented, while the extension stems were uncemented. Tibial stems were implanted in all cases. The femoral extension stem was used in seven cases (37%) in the primary group and in 18 cases (69%) in the revision group. The decision to implant the femoral stem was taken intraoperatively in relation to the quantity and quality of the patient’s bone stock. Bone grafts were never used in any knee.
Post-Operative Information
At the subject Institution the routine rehabilitation protocol after primary TKA includes passive motion exercises with the Kinetic machine and active mobilization exercises with physiotherapist the day after surgery. On the second day the patient performs active and passive motion exercises and is allowed 50% weight-bearing with two crutches for 40 days. After the first post-operative clinical/radiographic control (at 45 days after surgery) the patient is allowed to walk with a crutch on the non-operative side for 15 days and afterwards is allowed full weight-bearing. Active mobilization exercises are prescribed for at least three months after surgery.
The routine rehabilitation protocol after revision TKA includes 30% weight-bearing with aid of walker with axillary supports since the second or third postoperative day (if patient’s conditions allow) for at least 20 days. During the same period the patient performs active and passive motion exercises. The patient is then allowed to walk with two crutches (50% weight-bearing) for 20 days and afterwards with a crutch for 15 days until full weight-bearing. The rehabilitation program after revision TKA is, however, more personalized than after primary TKA.
In the cohort of difficult primary TKAs and revision TKAs documented in this study, the median hospital stay was 13 days (interquartile range: 10 - 18 days) and 15 days (interquartile range: 11 - 18 days) in the primary group and in the revision group, respectively.
Clinical Outcome Evaluation
At the follow-up visit in December 2013 the patients were assessed with both the ‘Tegner Lysholm Knee Scoring Scale’ (TLKSS) [24] and the ‘Knee Injury and Osteoarthritis Outcome Score’ (KOOS) [25]. The ‘Western Ontario and McMaster Universities Arthritis Index’ (WOMAC) [26] was derived from the KOOS outcomes.
The TLKSS evaluates limp (5 points), support (5 points), pain (25 points), instability (25 points), locking (15 points), swelling (10 points), stair climbing (10 points), and squatting (5 points). The maximum total score is 100 points, which corresponds to the best result. According to Mitsou et al. [27], the TLKSS total score was categorized as: excellent (>90 points), good (84 - 90 points), fair (65 - 83 points) or poor (<65 points). Although this score was designed for patients undergoing reconstruction of the anterior cruciate ligament, it has already been used to evaluate knee arthroplasty with acceptable results in terms of reliability [28].
The KOOS questionnaire is an extension of the WOMAC questionnaire. KOOS is a 42-item questionnaire that covers five patient-relevant dimensions (five subscales): symptoms, pain, ‘activities of daily living’ (ADL), ‘sport and recreational activities’ and knee-related ‘quality of life’ (QoL). The answer to each question is associated to an integer value between zero (best outcome) and four (worst outcome). In each of the five subscales, the items are summed up and the sum is linearly transformed in a percentage scale, with zero representing extreme knee problems and 100% representing no knee problems (i.e. a mean of zero points in each item corresponds to a score of 100%, a mean of one point to a score of 75%, a mean of two points to a score of 50%, a mean of three points to a score of 25% and a mean of four points to a score of 0%).
The WOMAC score could be calculated through the KOOS score. As the WOMAC is a widely used score [29], it was included in order to possibly compare the results of this study with the results from literature. The WOMAC produces three subscale scores (pain, stiffness and physical function) and a total score (WOMAC Index) that reflects disability overall [30]. The WOMAC Pain questions are included in the KOOS Pain questions, the WOMAC Stiffness questions are included in the KOOS Symptoms questions and the WOMAC Function questions are equivalent to the KOOS ADL questions [29]. The scores of each of these three scales and the WOMAC Index were standardized to a range of values from zero to 100, with zero representing the worst and 100 of the best results.
Additionally, the knee flexion and the knee flexion contracture at final follow-up were assessed.
Finally, the patients were specifically asked whether they had pain around the tip of femoral or tibial stems.
Radiographic Evaluation
The following parameters were assessed: radiolucent lines and osteolysis around the implant components, and cortical bone hypertrophy around the femoral and tibial stems.
A radiolucent line is a lucency at the interface between the cement and the bone (in case of cemented implants) or between the bone and the implant (in case of uncemented implant).
Osteolysis was defined as a lytic lesion that was not present on immediate postoperative radiographs. The osteolytic areas were quantified by using the maximum diameter and the widest length perpendicular to this diameter. The areas were approximated as ellipses [31]. The osteolytic areas were classified as ≤ 1 mm2, between 1 mm2 and 5 mm2, and larger than 5 mm2. Only osteolytic areas greater than 1 mm2 were considered in the analysis.
The distribution of the radiolucent lines and the osteolytic areas were assessed according to Whaley et al. [32], who modified the zones initially defined by the Knee Society [33] to accommodate the presence of the femoral and tibial stems (Fig. 1).
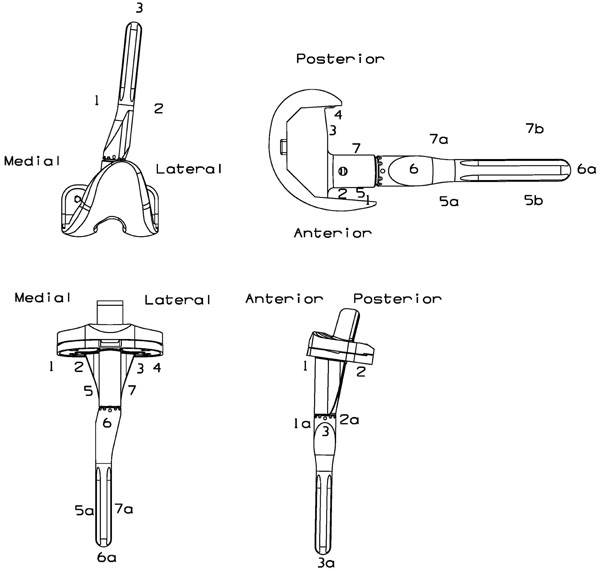
Radiographic zones of the femoral and tibial components in anteroposterior and lateral views, according to Whaley et al. [32].
Demographic data and implant characteristics in the initial study cohort stratified per surgery type (i.e. primary TKA or revision TKA).
| Primary Group | Revision Group | p-Value | |
|---|---|---|---|
| N° of knees | 19 | 26 | |
| Gender (n, %) | |||
| Male | 5 (26%) | 3 (12%) | |
| Female | 14 (74%) | 23 (88%) | |
| Side (n, %) | |||
| Left | 6 (32%) | 9 (35%) | |
| Right | 13 (68%) | 17 (65%) | |
| Age at surgery [yrs] mean ± SD/(range)( ( median/(IQR)( (distribution |
69 ± 10/(43 - 82) 70/(60 - 77) N |
72 ± 7/(56 - 85) 73/(67 -77) N |
p=0.184 (a) |
| Indication for CCK implant | -ligament loosening -severe varus/valgus deformity -severe osteoarthritis |
-ligament loosening -severe varus/valgus deformity -severe bone loss/bad bone quality |
|
| Pre-op Diagnosis (n, %) |
Primary OA (11; 58%) Post-osteotomy OA (3; 16%) Post-traumatic OA (2; 11%) Osteonecrosis (1; 5%) Rheumatoid Arthritis (2; 11%) |
Aseptic TKA loosening (14; 54%) Aseptic UKA loosening (7; 27%) Infected TKA (5; 19%) |
|
| Stem extensions | |||
| N° of knees with femoral stem (n, %) | 7 (37%) | 18 (69%) | |
| Femoral stem diameter [mm] median/ most used/(range) |
15 /15/(13 - 20) |
14/14/(11 - 18) |
|
| Femoral stem length [mm] median/ most used/(range) |
75/75/(30 - 75) |
75/75/(30 - 155) |
|
| N° of knee with tibial stem (n, %) | 19 (100%) | 26 (100%) | |
| Tibial stem diameter [mm] median/most used/(range) |
12/12/(11 - 16) |
12.5/12 and 14/(10 - 15) |
|
| Tibial stem length [mm] median/most used/(range) |
75/75/(30 - 100) |
75/75/(75 - 155) |
|
| Hospital stay [days] mean ± SD/(range) median/(IQR) distribution |
14 ± 6/(9 - 31) 13/(10 - 18) N |
16 ± 8/(9 - 39) 15/(11 – 18) N |
p=0.467 (b) |
| Implantation time [yrs] mean ± SD/(range) median/(IQR) distribution |
10.6 ± 2.2/(2.4 - 12.5) 10.8/(10.5 - 11.6) N |
11.3 ± 1.1/(7.6 - 12.8) 11.3/(10.9 – 11.9) N |
p=0.135 (b) |
|
|||
Clinical outcomes at minimum 10 years.
| Primary Group (n=15) |
Revision Group (n=24) |
p-Value | |
|---|---|---|---|
| Follow-up time [yrs] mean ± SD/(range) median/(IQR) distribution |
11.2 ± 0.7/(10.2 -12.5) 11.2/(10.7 - 11.6) N |
11.4 ± 0.8/(10.2 - 12.8) 11.3/(10.9 - 11.9) N |
p=0.445 (a) |
| Flexion of the knee mean ± SD/(range) median/(IQR) distribution |
97° ± 6°/(90° - 110°) 100°/(90° - 100°) N |
94° ± 7°/(90° - 110°) 90°/(90° - 100°) N |
p=0.158 (b) |
| Flexion contracture of the knee mean ± SD/(range) median/(IQR) distribution |
0° ± 0°/(0° - 0°) 0°/(0° - 0°) N |
0° ± 0°/(0° - 0°) 0°/(0° - 0°) N |
p=1.000 (b) |
| TLKSS: Total (0 - 100 pts) mean ± SD/(range) median/(IQR) distribution |
86 ± 10/(55 - 95) 87/(83 - 93) N |
79 ± 10/(60 - 99) 80/(75 - 88) N |
p=0.021* (b) |
| TLKSS: Overall grading (n, %) | |||
| Excellent (>90 pts) | 5 (33%) | 3 (13%) | Excellent/good vs fair/poor 73% (primary) vs 33% (revision) p=0.022* (c) |
| Good (84 - 90 pts) | 6 (40%) | 5 (21%) | |
| Fair (65 - 83 pts) | 3 (20%) | 13 (54%) | |
| Poor (<65 pts) | 1 ( 7%) | 3 (13%) | |
| KOOS [%] mean ± SD/(range) median/(IQR) distribution |
|||
| Symptoms (S1-S7) | 70.7 ± 8.1/(53.6 - 89.3) 71.4/(67.9 - 75.0) N |
69.8 ± 5.7/(53.6 - 78.6) 71.4/(67.9 - 74.1) N |
p=0.678 (a) |
| Pain (P1-P9) | 77.0 ± 9.6/(50.0 - 86.1) 77.8/(75.0 - 83.3) N |
74.8 ± 6.3/(50.0 - 80.6) 75.0/(75.0 - 77.8) N |
p=0.072 (b) |
| Function in daily living (A1-A17) | 70.7 ± 19.0/(11.8 - 85.3) 77.9/(70.6 - 79.4) N |
68.3 ± 12.5/(11.8 - 79.4) 70.6/(67.7 - 70.6) N |
p=0.004* (b) |
| Sport and Recreational activities (SP1-SP5) | 37.7 ± 11.8/(10.0 - 60.0) 35.0/(35.0 - 45.0) N |
37.7 ± 8.7/(10.0 - 45.0) 35.0/(35.0 - 45.0) N |
p=0.988 (b) |
| Quality of life (Q1-Q4) | 52.9 ± 13.7/(31.3 - 68.8) 50.0/(43.8 - 68.8) N |
50.3 ± 10.0/(31.3 - 68.8) 46.9 (43.8 - 59.4) N |
p=0.470 (b) |
| WOMAC [%] mean ± SD/(range) median/(IQR) distribution |
|||
| Pain (i.e. KOOS P5-P9) | 85.0 ± 10.0/(55.0 - 95.0) 85.0/(85.0 - 90.0) N |
82.7 ± 7.1/(55.0 – 90.0) 85.0 (80.0 - 85.0) N |
p=0.111 (b) |
| Stiffness (i.e. KOOS S6-S7) | 81.7 ± 10.4/(62.5 - 100.0) 75.0/(75.0 - 87.5) N |
81.3 ± 10.4/(62.5 – 100.0) 75.0/(75.0 – 87.5) N |
p=0.913 (b) |
| Function (i.e. KOOS A1-A17) | 70.7 ± 19.0/(11.8 - 85.3) 77.9/(70.6 - 79.4) N |
68.3 ± 12.5/(11.8 - 79.4) 70.6/(67.7 - 70.6) N |
p=0.004* (b) |
| Index (i.e. WOMAC total) | 74.6 ± 15.5/(30.2 - 88.5) 80.2/(74.0 - 81.2) N |
72.4 ± 10.5/(25.0 - 81.2) 74.0 (72.1 - 75.8) N |
p=0.010* (b) |
|
|||
Radiographic results at minimum 10 years.
| Primary Group (n=15) |
Revision group (n=24) |
|||
|---|---|---|---|---|
| With Femoral Stem (n=4) | Without Femoral Stem (n=11) | With Femoral Stem (n=17) | Without Femoral Stem (n=7) | |
| Radiolucent lines | ||||
| Femoral side | None | None | None | None |
| Tibial side - AP view | None | None | None | None |
| Tibial side - Lateral view | None | None | None | None |
| Osteolysis | ||||
| Femoral side - AP view | None | N/A | zone 2 (1/0)° | N/A |
| Femoral side - Lateral view | zone 7 (1/0) | zone 5 (1/0) | zone 5a (1/0)° zone 5b (1/0)° |
None |
| Tibial side - AP view | zone 5 (1/0) zone 5a (1/0) zone 7 (1/0) zone 7a (1/0) |
None | zone 5 (1/0)° zone 5a (1/0)° zone 6a (1/0)° |
zone 5a (1/0) |
| Tibial side - Lateral view | zone 1a (2/0) zone 2a (1/0) |
zone 2a (1/0) zone 3a (1/0) |
zone 1a (1/0) zone 2a (2/0)° zone 3a (1/0)° |
None |
| Cortical bone hypertrophy around the stem | ||||
| Femoral | None | N/A | 1x zone 6a | N/A |
| Tibial | None | None | None | 1x zone 7a |
|
||||
Studies documenting the results of TKAs performed with CCK implants at a mean follow-up of at least 5 years (published in the last 10 years): Primary TKA.
| Indications for CCK Prosthesis | N° of Knees at Study Start (N° of pts) | Implant Type | % of Knees with Stem Extension | Implantation Period | Mean Age at Surgery [yrs] | Mean Follow-Up [yrs] | Mean WOMAC at Follow-Up [%] | Mean Flexion at Follow-Up | Complications | N° of CCK Implant Revisions (Raw Revision Rate) | Cumulative Survival [TKAs Remaining] |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Present study |
Ligament deficiency -severe varus/ valgus deformity -severe osteoarthritis |
19 (19) | NexGen LCCK | 100% | 2001-2003 | 69 ± 10 (43 to 82) | 11.2 ± 0.7 (10.2 to 12.5) | 74.6 ± 15.5 (30.2 to 88.5) | 97°± 6° [90° to 110°] | none | 0 (0) | 100% at 10 yrs [17] |
| Maynard 2014 [18] | Varus/valgus laxity greater than 5 mm at any point of the knee ROM. | 127 (114) | NexGen LCCK |
100% | 1996-2004 | 68.3 (42 to 86) | 9.2 (7.4 to 12.8) | 84.8 ± 13.6 |
117° ± 6° (95° to 130°) | 2x infection (2x R) 4x periprosthetic Fx (1x R) 6x patellar clunk syndrome 3x nerve palsy 1x patella Fx 1x patella AVN 1x patella tendon rupture 1x wound dehiscence 3x superficial infection 3x other (PE, CVA, ileus) |
3 (3/127=2.4%) | 97.6% (95% CI, 94% to 100%) at 10 yrs [NR] |
| Nam 2012 [19] | Severe deformity and compromised collateral ligament in elderly patients. | 190 (181) | Optetrak Non-Modular Constrained Condylar Knee (Exac-tech) | 0 | 2002-2007 | 72.3 ± 10.2 | 7.3 ± 2.1 (min. 3.8) | NR |
NR | 5x femoral component loosening (5x R) 1x infection (1x R) 1x stiffness (1x R) 1x knee instability (1xR) |
8 (8/190=4.2%) | NR |
| Lachiewicz 2011[17] | Incompetent medial collateral ligament and inability to balance the knee; inadvertent sectioning of the medial collateral ligament; presence of Charcot-like arthropathy |
30 (28) | NexGen LCCK |
100% | 1999-2007 | 73.9 (58 to 94) | 5.4 (2 to 11.5) | NR | 114° (100° to 130°) |
1x infection (1xR) 2x asymptomatic, minimally displaced patella Fx 5x asymptomatic calf thrombus |
1 (1/30=3.3%) | NR |
| Lachiewicz 2006[5] | Severe valgus deformity; incompetent medial collateral ligament; severe flexion contracture.; |
54 (44) | Total Condylar III (J&J) and Insall/ Burstein II (Zimmer) |
less than 50% | 1983-1998 | 67 (40 to 91) | 9 (5 to 16) | NR |
97.48° (60° to 130°). |
1x symptomatic loosening of the femoral component (1x R) 1x symptomatic loosening of the tibial component (1x R) 1x posterior dislocation of the knee 2x asymptomatic patella osteonecrosis |
2 (2/54=3.7%) | 96% (95% CI, 90.6 to 100) at 10 yrs [17] |
|
||||||||||||
Studies documenting the results of TKAs performed with CCK implants at a mean follow-up of at least 5 years (published in the last 10 years): Revision TKA.
| Indications for CCK Prosthesis | N° of Knees at Study Start (N° of Pts.) | Implant Type | % of Knees with Stem Ex-tension | Implantation Period | mean Age at Surgery [Yrs] | mean Follow-Up [yrs] | mean WOMAC at Follow-Up [%] | Mean Flexion at Follow-Up | Complications | N° of CCK Implant Revisions (Raw Revision Rate) | Cumulative Survival [TKAs Remaining] |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Present study | -ligament deficiency -severe varus/valgus deformity -severe bone loss/bad bone quality |
26 (26) | NexGen LCCK | 100% | 2001-2003 | 72 ± 7 (56 to 85) | 11.4 ± 0.8 (10.2 to 12.8) | 72.4 ± 10.5 (25.0 to 81.2) | 94° ± 7° (90° to 110°) | None | 0 | 100% at 10 yrs [25] |
| Wilke 2014 [22] | Soft tissue deficiency; Marked bone loss |
234 (209) | Total Condylar-III (Depuy) | 99% |
1995-2000 | 69.3 (33 to 89) | 9 (0.25 to 17.7) | NR | 98.6° ± 16° | 18x infection (18x R) 22x aseptic loosening, osteolysis or pain (22x R) |
40 (40/234= 17.1%) |
81% at 10 yrs [98] |
| Lee 2013 [16] | Asymmetrical extension and flexion gap; uncorrectable large flexion gap, mid flexion instability; posterolateral subluxation. |
79 (68) | NexGen LCCK |
100% | 1998-2008 | 68.8 (46 to 83) | 5.3 ± 2.3 (2 to 12.3) | NR | 108° (30° to 140°) | 4x recurrent infection (4x R) 1x periprosthetic Fx (plate fixation) 2x stem tip pain 1x aseptic loosening (1x R) |
5 (5/79=6.3%) | 93.0% at 8 yrs [12] |
| Kim 2009 [20] | Absence of posterior cruciate ligament and a deficient medial or lateral collateral ligament but with intact quadriceps mechanism. |
114 (97) | NexGen LCCK |
100% | 1998-2003 | 65 (26 to 81) | 7.2 (5 to 10) | See note (°) | 106° (67° to 125°) | 1x femoral component aseptic loosening (1x R) 3x tibial component aseptic loosening (3x R) 2x recurrent infection (2x R) 3x quadriceps tendon rupture 1x fracture of the tibial post leading to instability (1x R) |
7 (7/114=6.1%) | 96% (95% CI, 94 to 100%) at 10 yrs [NR] |
| Sheng 2005 [21] | NR | 16 (14) | Total Condylar-III (Depuy) |
100% | 1994-2000 | 59 (36 to 78) | 6.2 (3.7 to 10.2) | NR | 98° (0° to 145°) | 1x severe patellar pain treated with resurfacing 1x patellar fracture 1x infection (1x R) |
1 (1/16=6.3%) | NR |
|
||||||||||||
Cortical bone hypertrophy around the stem was defined as a thickening of the cortical diaphyseal bone.
Radiographic implant loosening was defined as the presence of continuous radiolucent lines of 2 mm or more adjacent to the fixation interface of the femoral or the tibial implant components [34].
Radiographic parameters were assessed with a digital system by two authors (S.B and G.C.), who analysed the radiographs independently, gave an estimate independently and agreed on a final value.
Statistical Analysis
Categorical data was summarized using counts and percentages, while continuous data was expressed as mean, standard deviation (SD), range, median and interquartile range (IQR). The Shapiro-Wilk test was used to test for normality.
Comparison between groups (i.e. primary TKA vs revision TKA) was performed with Student's t-test in case of normally distributed continuous data or with Mann–Whitney U-test for non-parametric analysis, while proportions were compared by Chi-squared test or by Fisher’s exact test, as appropriate. For all comparisons, a p value of <0.05 was considered to indicate statistical significance.
The statistical analysis was carried out with IBM SPSS 21 (IBM Corp.).
RESULTS
In December 2013, of the 44 patients (45 knees) in the initial cohort, 38 patients (39 knees) were assessed clinically and radiographically at a minimum of ten years after surgery. One patient (one knee in the primary group), who was not interested to return for follow-up, was interviewed by phone (the questions regarded pain, quality of life and surgery related complications). None of the patients had been revised and no complication was reported. The remaining five patients (three knees in the primary group and two knees in the revision group) had died at 8.2 ± 3.7 years (range: 2.4 - 12 years) after the implantation. As confirmed by their relatives who were reached by phone, all these five patients were unrevised at the time of death.
In summary, in the study cohort consisting of 45 TKAs in 44 patients, there was no revision after a mean implantation time per TKA of 11.0 ± 1.6 years (range: 2.4 - 12.8 years) (for this calculation, for the patients who had died, the date of death was used).
Clinical Outcome Evaluation (Table 2)
At the follow-up in December 2013, the median total TLKSS was 87 points (IQR: 83 - 93) in the primary group and 80 points (IQR: 75 - 88) in the revision group (p=0.021). According to the TLKSS scoring, the results were classified as good or excellent in 73% of patients in the primary group and in 33% of patients in the revision group (p=0.022); fair results were documented in most of the patients in the revision group (54%). One patient (7%) in the primary group and three patients (13%) in the revision group had results classified as poor. Specifically, three of these patients had poor muscle tone already before surgery and had a poor postoperative recovery (including the patient who sustained primary TKA, who had also a severe ankylosis), while the fourth one was a septic revision.
The median WOMAC Index was 80.2% (IQR: 74.0% - 81.2%) and 74.0% (IQR: 72.1% - 75.8%) in the primary and in the revision group, respectively. Patients in the primary group had significantly better results (p=0.010).
The median knee flexion at the last follow-up was 100° (IQR: 90° - 100°) and 90° (IQR: 90° - 100°) in the primary group and in the revision group, respectively (p=0.158). No patient had either knee flexion contracture or pain around the stem tip.
Considering also the patient who was interviewed only by phone, a walking aid (a stick or a crutch) was needed in six cases (38% of 16 TKAs) in the primary group and in twelve cases (50% of 24 TKAs) in the revision group. Patients were unable to deambulate in two cases in the primary group (13%) (including the patient who was reached only by phone) and in one case in the revision group (4%). Two of these patients had a limited functional recovery due to a pre-surgery poor muscle tone that did not improve post-surgery, while in the third patient (the patient who was reached only by phone) the functional recovery was limited due to a psychiatric disease.
Radiographic Evaluation (Table 3)
At the last follow-up there was no radiographic evidence of prosthetic component loosening. No radiolucent lines were identified around the prosthetic components. Five knees (33% of 15 TKAs) in the primary group and three knees (13% of 24 TKAs) in the revision group showed osteolytic areas in one or more radiographic zones. In all cases, osteolytic areas were smaller than 5 mm2. One patient had osteolytic area in all the four radiographic views; nevertheless, the radiographies did not show any radiolucency around the implant or any clinical sign of loosening.
Cortical bone hypertrophy around the stem was identified in two patients, both in the revision group. One had bone hypertrophy at the femoral stem tip (zone 6a), while the other at the tibial stem lateral side (zone 7a). None of the patients complained of pain around the tip of femoral or tibial stems.
DISCUSSION
The most important finding of the present study was the lack of any complication related either to the surgical procedure or to the implant at a mean implantation time of 11.0 years.
In order to compare the results of this single surgeon series with other similar cohorts, a literature search on studies documenting TKAs performed with any CCK implant was conducted. The retrieved studies have been summarized in Table 4 and in Table 5 for the primary setting [5, 17-19] and for the revision setting [16, 20-22], respectively. Four studies [16-18, 20] documented the results with the NexGen LCCK, subject of the present study; one study [19] documented the results with the Optetrak Non-Modular Constrained Condylar Knee (Exactech Inc, Gainesville, Florida), which did not have stem extensions; one study [5] documented the Insall-Burstein II (Zimmer Inc), which was the predecessor of the NexGen LCCK and offered modular stem extensions, too, but for example had less articular surface thicknesses than the successor; finally, three studies documented the Total Condylar III system (DePuy, Johnson & Johnson, Warsaw, IN, USA) in a non-modular (i.e. without modular stem extension) [5] and in a modular version [21, 22].
One of the most used parameters to assess the arthroplasty results is the survival rate. In the reviewed literature, the documented cumulative survival rates at ten years for different types of CCK implants are between 96% and 97.6% in the primary setting [5, 18], and between 81% and 96% in the revision setting [16, 20, 22].
Regarding device related adverse events, in one of these studies the breakage of the tibial intercondylar eminence was documented [20]. On the contrary, the disengagement of the PE insert from the tibial tray was not reported in any of these case series, even though this complication was the subject of a few case reports on TKAs performed with the NexGen LCCK [7, 8]. The failure mechanism is, however, not clear.
First of all, it should be considered that this implant design requires the surgeon to engage the PE insert, which has a dovetail locking mechanism, onto the tibial tray and to tighten a locking screw [7]. A first possible explanation for the disengagement has been provided by Chen et al. [7], who considered, as a possible cause, the cyclic antero-posterior lever mechanism on the PE insert. In summary, during knee flexion the resultant of the forces directed downwards to the posterior half of the insert causes a ‘lift-off’ of the anterior half of the insert, while vice versa in full extension the resultant of the forces directed downwards to the anterior half of the insert causes a posterior ‘lift-off’. This cycle, which is repeated daily a thousand times during normal activities (e.g. going up and down the stairs, sitting and standing, walking), may lead to the loosening of the locking screw.
A second possible explanation has been proposed by Rapuri et al. [8]. The authors suggested that a counter-clockwise torque that is created between the insert and the tibial tray might be the cause for the disengagement. In summary, during knee flexion lateral rollback of the femur occurs on the tibia (external rotation of the femur on the tibia) while during knee extension the lateral side of the femur rolls forward (internal rotation of the femur on the tibia). In the right knee, the roll forward, due the high rotational constraint of the tibial post on the femoral box, produces a counter-clockwise torque on the tibial post and therefore on the entire insert, which, over many cycles, may disengage the screw. On the contrary, in the left knee, this same mechanism creates a clockwise torque, which cannot disengage the screw. Up to now in the literature, four screw disengagement cases have been reported on the right knee [8] and two on the left knee [7, 8].
Finally, an inadequate surgical technique, consisting of an inappropriate engagement of the insert onto the tibial tray or the application of inadequate locking force on the locking screw, might also be considered as a possible explanation for the failure [7].
Regarding adverse events possibly related to extension femoral or tibial stems, neither stem loosening, nor stem breakages, nor pain around the stem tips have been detected in the present study. On the contrary, cortical bone hypertrophy around the stem tip was detected but only in two cases out of 39 TKAs. Among the reviewed studies that documented the use of extension stems [5, 16-18, 20-22], only one study reported stem tip pain in two patients [16].
Among the reviewed literature, no study documented the TLKSS or the KOOS scores, but Maynard et al. [18] reported the WOMAC score in a study on primary TKA patients. The authors documented a mean WOMAC Index of 84.8% ± 13.6% after a mean follow-up of 9.2 years (min. 7.4 years) in primary TKA, which is slightly higher than the mean score documented in the primary TKA cohort in the present study (i.e. 74.6 ± 15.5 at a mean follow-up of 11.2 years (min. 10.2 years)).
This study has a few limitations. First, it is a single surgeon, non-comparative, retrospective cohort analysis, thus the generalizability of these results may be limited. Secondly, the analysis lacks of the preoperative functional outcome scores. It should, however, be considered that if a patient was indicated to receive a CCK implant, he/she had a highly debilitating clinical condition and therefore his/her preoperative functional outcome scores would have been probably classified as poor, according to the TLKSS score categories. Another limit of the study is the relatively small cohort; it should however be considered that no patient was lost-to-follow-up. On the other side, the findings of the present study are significant because, to the best of the authors’ knowledge, this is the first study documenting patients who have been implanted with this CCK implant and who have been followed-up for at least ten years. In summary, the results of this study expands the clinical evidence on the performance of CCK implants in the long-term.
CONCLUSION
This study on a single surgeon consecutive series of total knee arthroplasties performed with a condylar constrained knee, demonstrated satisfactory patient outcomes with no re-operation at minimum ten years after implantation in both the primary and the revision settings.
CONFLICT OF INTEREST
Andrea Camera, Stefano Biggi and Gabriele Cattaneo have no competing interests. Giovanni Brusaferri is employed by Zimmer GmbH (Winterthur, Switzerland).
ACKNOWLEDGEMENTS
Declared none.


