All published articles of this journal are available on ScienceDirect.
Documentation of Focal Neurology on Patients with Suspected Cauda Equina Syndrome and the Development of an Assessment Proforma
Abstract
Objective :
Cauda equina syndrome is a relatively rare condition with a disproportionately high medico legal profile. Definitive management involves prompt surgical decompression with outcome dependent on timing of surgery. Documentation of a comprehensive clinical and neurological assessment including examination of anal tone and perianal sensation is essential in reducing litigation and identifying patients requiring urgent surgical decompression. The aim of this study was to evaluate the documentation of focal neurology in patients with suspected cauda equina syndrome and devise an assessment proforma to use in the accident and emergency departments.
Methods :
A retrospective case note review was performed in all patients presenting to A&E with suspected cauda equina syndrome from January 2013 to March 2014. A full neurological examination was defined as having all modalities documented such as: MRC grade power, reflexes, sensory exam, vibration proprioception, anal tone & perianal sensation.
Results :
Sixty-nine patients with suspected cauda equina syndrome were identified with a median age of 44 (35-55) and a male to female ratio of 1:1.6. 4 patients (6%) had confirmed cauda equina syndrome and were transferred to a tertiary neurosurgical centre for further management. Only 2 patients (3%) had a complete neurological examination documented. 11 (16%) patients did not have any documentation of perianal sensation and 8 patients (12%) did not have documentation of anal tone
Conclusion :
Documentation of neurological was poor across our department. The introduction of an assessment proforma is proposed to increase documentation and optimise emergency department evaluation in these patients.
BACKGROUND
André Du Laurens (1558-1609) was a prominent French anatomist who first coined the term ‘cauda equina’ (horses tail) to describe the collection of dorsal and ventral lumbar, sacral and coccygeal nerve roots surrounding the filum [1]. However, it wasn’t until 1934 when Mixter and Barr described a clinical syndrome of a ruptured herniated disc causing compression at the cauda equina [2, 3]. Cauda Equina Syndrome (CES) is a rare but severe neurosurgical disorder with a disproportionately high medico-legal profile. It comprises 2-6% of all lumbar disc operations and has an incidence between 1 in 33,000 to 1 in 100,000 [4-6]. It is essential to recognise and document the red flag features of CES as timing of surgery is dependent on post-operative outcome; surgery within 48 hours is associated with a better outcome than delayed surgery [6].
AETIOLOGY
The commonest cause of CES is a large herniated lumbar disc at L4/L5 and L5/S1. Other less common causes include: spinal fractures, spinal neoplasms, spinal abscesses, spinal TB, haematomas and other space occupying lesions have also been reported such as schwannomas, ependymomas, and facet joint cysts [7].
CLINICAL FEATURES
Cauda equina syndrome results from dysfunction of multiple sacral and lumbar nerve roots, which can cause a combination of clinical features. The term Cauda equina syndrome is only used when there is impairment of bladder, bowel or sexual dysfunction and perianal or saddle numbness [7, 8]. Other possible symptoms include back pain (with or without sciatica), sensory changes in the lower limbs, lower limb weakness and reduction or loss of reflexes in the lower limbs [7]. All patients with suspected Cauda equina syndrome should have a thorough neurological examination including perineal and perianal sensation and assessment of anal tone. Perianal sensation is often poorly tested, the patient should be in the left lateral position and sensation should be tested outside towards the sphincter using a gloved finger stroke and, if there is any uncertainty, an unfolded paper clip can be used. Loss of bulbocavernosus reflex (whereby simulation of the glans penis/clitoris causes reflex contraction of the anal sphincter), loss of anal tone and perianal sensation is suggestive of CES [7].
Tandon and Sankaran described three variations of cauda equina syndrome [9]:
1. Rapid onset without a previous history of back problems
2. Acute bladder dysfunction with a history of low back pain
3. Chronic backache and sciatica with gradually progressive cauda equina syndrome with canal stenosis
In addition, CES can be classified as complete (CES-R) and incomplete (CES-I) in relation to urinary retention and perineal sensation [10]. In CES-I patients present with motor and sensory changes such as saddle anaesthesia but have yet to develop full retention or incontinence of bowel or bladder. They experience neurogenic symptoms of straining micturition and altered stream [4]. In CES-R patients have developed true retention secondary to the loss of visceral neurogenic signal causing painless retention and overflow incontinence. It is essential to distinguish whether CES is complete or incomplete. A useful test involves testing trigone sensitivity with an inflated foley catheter, which is pulled when the patient is unaware. This should produce the urge to micturate, which will help distinguish patients with a genuine neurological deficit from those with painful retention [4].
Management
Recent guidelines published by the Society of British Neurological Surgeons recommend an urgent MRI spine for patients with CES-R, CES-I and suspected Cauda equina syndrome [11]. All emergency departments receiving patients with suspected CES should have an agreed protocol with a local spinal unit for assessment, imaging and management of these patients. If Cauda equina compression is confirmed, immediate transfer of the patient to a tertiary neurosurgical centre should be made with all imaging and documentation [6]. Patients with Cauda equina syndrome requires decompressive surgery; the timing of such surgery is a matter of huge controversy with immediate, early and late surgical decompression reporting varied outcomes [12]. However, such studies have been limited to retrospective reviews as class I evidence from randomised controlled trials will never gain ethical approval as there will never be a study in which patients are randomised to delayed surgery [12, 13]. Todd and colleagues in a large meta-analysis concluded that patients treated earlier than 24 hours after the onset of CES are more likely to retain bladder function than those treated beyond 24 hours (p=0.03); patients treated within 48 hours are more likely to retain bladder function than those treated beyond 48 hours (p=0.005) [12]. They conclude that timing of surgery following CES probably does affect outcome. Therefore, early recognition by means of a thorough history and neurological assessment in A&E and prompt imaging is crucial in ensuring these patients get transferred for decompressive surgery [12].
Medico-Legal Significance
The majority of patient complaints after an episode of CES come from those with residual symptoms [4]. It is of utmost importance, therefore, that red flag symptoms are not only spotted, but also comprehensively recorded in clinical notes. As already discussed, best evidence seems to indicate that early surgical intervention yields the most positive outcome for the patient, especially in terms of bowel and bladder function. Given the rarity of the condition, it may not be as quickly identified as necessary to boost the probability of a good post-CES outcome. Delays of this nature may occur in both primary and secondary care. Non-availability of MRI scanning and specialist neurosurgical expertise can also delay the diagnosis. Gardner and colleagues point out, anecdotally, that most damages are eventually awarded due to a lack of accurate documentation in clinical notes [4]. Time of onset of neurological symptoms, and any on going change in bladder function were particularly poorly documented. Failure to perform a digital rectal examination is also a potential cause of litigation [8].
In a ten year period (1997-2006) there were 107 recorded cases of litigation due to negligence in the management of CES [4]. Over half (52%) of claims were directed at the inpatient team, and over a third (35%) were directed at the Accident and Emergency department [4]. This highlights the importance of spotting, and documenting, red flag symptoms at the very beginning of the patient journey. Over a recent five year period (2003-2007 inclusive), the total payout in compensation was £6,720,000, representing a significant amount in damages [4].
As the early detection and management of CES is so crucial, it is of equal importance that documentation of neurological examination is of the highest quality. This not only aids in the detection of CES, but also in the defence of any potential claim that may arise in the future.
The aims of our study were twofold, firstly to assess documentation of focal neurology in patients with suspected Cauda equina syndrome and secondly to develop an emergency department assessment proforma to enable comprehensive clinical and neurological assessment of these patients.
METHODS
Following audit approval, a retrospective case note review was performed on all patients presenting to the accident and emergency department with suspected cauda equina syndrome from January 2013 to March 2014 at our busy teaching hospital. All neurosurgical referrals are taken via the on-call neurosurgical registrar who is based out of site, at the regional tertiary neurosurgical hospital. Case notes were evaluated independently to assess documentation of various modalities, which are outlined in the table below (Table 1):
A fully comprehensive neurological examination was defined as one that documented all the above modalities. In addition, documentation of the name of neurosurgical registrar and on-call neurosurgical consultant, time of discussion with neurosurgical team, time of MRI scan and plan from the neurosurgical team was also assessed. A total of 69 patients with symptoms suggestive of cauda equina syndrome were included in this study.
RESULTS
Sixty-nine patients with suspected cauda equina syndrome were identified with a median age of 44 (35-55) and a male to female ratio of 1:1.6. The median time to be seen by the orthopaedic team from admission was 164 minutes (109 m-238 m) with a mean length of stay of 2.8 days.
4 patients (6%) had confirmed cauda equina syndrome and were transferred to a tertiary neurosurgical centre for further management. Disc prolapse was the most common cause of suspected cauda equina syndrome in 36 patients (52%) followed by mechanical back pain in 17 patients (25%). The graph below (Fig. 1) demonstrates the various diagnoses in patients presenting with suspected CES at our trust.
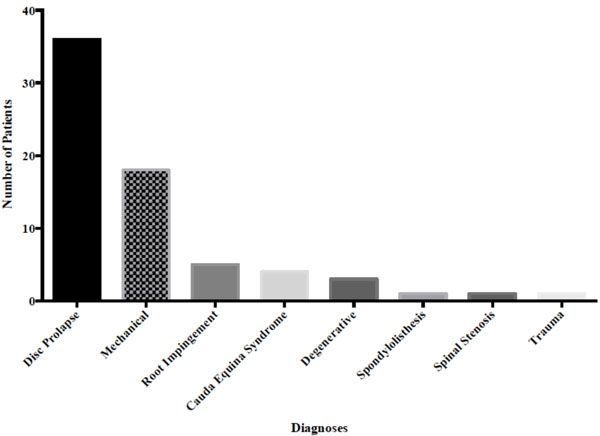
Bar chart demonstrating the various diagnoses in pateints presenting with suspected cauda equina sundrome.
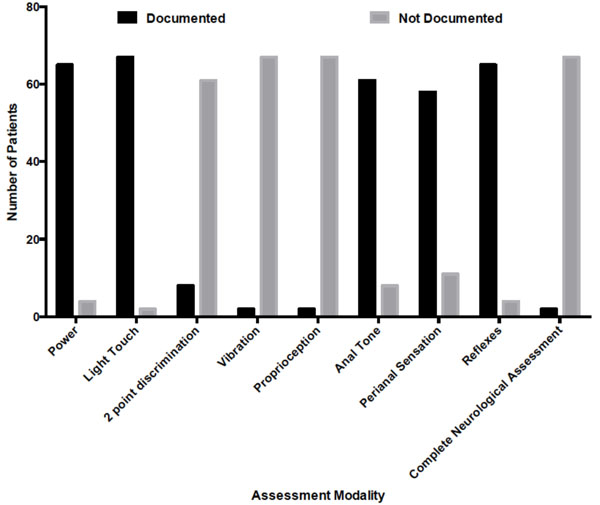
Graph demonstrating the proportion of patients with documentd and not documented neurological examination.
Various modalities of a comprehensive neurological examination.
| MRC Grade power of lower limbs |
| Sensory Examination (including light touch/two point discrimination) |
| Vibration & Proprioception |
| Anal Tone (active and passive) |
| Perianal Sensation |
| Bladder Post Void Residual Volume |
Documentation of neurological examination and other modalities in patients with suspected cauda equina syndrome.
| Assessment Modality | No of Patients Documented | No of Patients Not Documented |
|---|---|---|
| MRC Grade Power | 65 | 4 |
| Light Touch | 67 | 2 |
| Two-point discrimination | 8 | 61 |
| Vibration | 2 | 67 |
| Proprioception | 2 | 67 |
| Anal Tone | 61 | 8 |
| Perianal Sensation | 58 | 11 |
| Reflexes | 65 | 4 |
| Complete Neurological Assessment** | 2 | 67 |
| Post Void Bladder Residual Volume | 22 | 47 |
| Neurosurgical Registrar and Consultant Details | 31 | 38 |
** Neurological assessment was considered complete when all of the above modalities were tested and documented.
A complete neurological assessment included documentation of all the aforementioned variables. Only 2 patients (3%) had a complete neurological examination documented. Table 2 presents the proportion of patients who had an adequately documented neurological examination, which is represented graphically in Fig. (2).
40 patients (58%) with suspected CES got an urgent MRI scan within 24 hours. 13 patients (19%) with suspected CES failed to have MRI scans due to several reasons: 5 patients had contraindications to MRI and subsequently had a CT scan, 2 patients were advised as outpatient MRI scans, 3 patients refused and there was no documented reason for 3 patients. Remaining 16 patients (23%) did not warrant an urgent MRI based on clinical assessment and were discharged with advice and analgesia.
DISCUSSION
Cauda equina syndrome is commonly caused by a prolapsed intervertebral disc, which can cause serious disability, resulting in high-cost litigation in cases of mismanagement [5, 14]. Fig. (1) demonstrates the spectrum of diagnoses in patients with suspected cauda equina syndrome with a prolapsed disc being the most common cause in 36 patients. MRI coupled with patient history and examination remains the diagnostic gold standard in these patients. Paralysis, sensory abnormalities and long-term bladder, bowel and sexual dysfunction are just some of the complications of missed Cauda equina syndrome [12]. In addition, poor documentation is just one of several reasons for disastrous medico-legal consequences [4]. In this study, we report in our institution that documentation of a complete neurological examination is insufficient, with only 2 patients (3%) having a complete assessment documented. Given the potential for complications, it is essential that optimal management of such patients is achieved and begins with adequate assessment in the accident and emergency department. This ensures that patients with red-flag features of CES are identified early and triaged to a tertiary neurosurgical centre without any delay in order to minimise morbidity.
True Cauda equina syndrome remains rare. In our institution, 4 patients had confirmed Cauda equina syndrome and were transferred in-hours to a tertiary neurosurgical unit for further management. Most hospitals in the UK do not offer a 24-hour MRI service and therefore, such patients are often directly referred to neurosurgery on clinical grounds alone. A study by Crocker et al. demonstrate that patients with suspected CES presenting out of hours should have an MRI scan at the referring hospital the next morning, with a view to transfer for surgery depending on the outcome [14]. The principle of delaying surgery until day-light hours reflects the growing adherence to the National Confidential Enquiry into Perioperative Deaths guidelines relating to avoiding ‘on-call’ surgery unless a delay would result in severe harm, coupled with the uncertainty of the true value of immediate decompressive surgery in CES patients [14, 15]. However, Crocker and colleagues argue that patients with a short duration of symptoms (<12 h) should be considered for same-night transfer with a view to MRI and same night surgery as this group of patients would likely undergo an avoidable delay out of proportion to the delay in their presentation [14]. Patients with a delayed presentation should be considered for an in-hours approach to diagnosis and management.
Fig. (2) summarises the documentation of the individual modalities of a complete neurological examination. Whereas documentation of power, light touch, perianal sensation, anal tone and reflexes was adequate, there were still patients who had symptoms suggestive of Cauda equina syndrome where these modalities were not documented. A meta-analysis by Fairbank et al. showed that Perianal sensory loss and reduced anal tone have a high specificity in predicting MRI proven Cauda equina syndrome and therefore, should be assessed and documented in all patients [16]. In our study, 11 patients (16%) did not have any documentation of perianal sensation and 8 patients (12%) failed to have any documentation anal tone. Failure to document these findings can be due to various reasons in a busy A&E department such as difficulty finding a chaperone, however, this is an inexcusable reason in a litigation claim for misdiagnosed Cauda equina syndrome. It is probable that an adequate neurological examination was more thorough than this study would suggest. For example, after completing an examination the doctor may have simply documented “no focal neurology”. This is a clear limitation of our study. The problem with such generic statements is that they do not confirm that each of the aforementioned modalities such as anal tone, perianal sensation were tested, which leads to the debate whether these general statements would suffice in a medico-legal setting [4]. Ultimately it is the responsibility of the surgeon in charge of the patients care to ensure the patient has a thorough neurological assessment and that any patients with suspected CES gets prompt imaging and neurosurgical transfer, if indicated.
CONCLUSION
In our institution, documentation of a complete neurological examination was considered inadequate. We have devised and implemented a one-page assessment proforma for patients presenting to A&E with suspected cauda equina syndrome (included in the supplementary files). This proforma should be completed in the emergency department for all patients with suspected cauda equina syndrome. Assessment proformas are used frequently in A&E and have shown to be beneficial in managing various conditions ranging from strokes to hip fractures [17]. It is hoped that such a proforma will ensure more complete assessment and documentation of clinical examination by facilitating rapid documentation of pertinent information by the emergency department doctors.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


