All published articles of this journal are available on ScienceDirect.
Subsidence in Collarless Corail Hip Replacement
Abstract
The purpose of this study was to assess whether subsidence occurs in collarless Corail hip replacement (CCHR) and to ascertain the extent and timing of subsidence if present. Retrospective case notes analysis was performed. Sixty eight patients who had CCHR were identified from our database. Male to female ratio was 32:36. Their mean age was 74.2 years (range 37-95 years). Indications for surgery were osteoarthritis in 64 (94%) patients, rheumatoid arthritis in two (3%) patients and avascular necrosis in two (3%) patients. Subsidence was measured at 6 weeks, 6 months and 1 year post-op compared to initial post-op x-rays. At 6 weeks x-ray 21 patients did not have any subsidence, 18 patients had 1 millimeter (mm) subsidence, 10 patients had 2mms subsidence, 4 patients had 3mms subsidence, 5 patients had 4mms subsidence, 1 patient had 5mms subsidence, 4 patients had 6 mms subsidence and 1 patient each had subsidence of 7mms, 9mms, 11mms, 13mms and 26 mms respectively. When compared with 6 months x-rays only 2 patients had a further subsidence of 2mms while another patient had 3mms subsidence. No further subsidence occurred at 1 year follow up x-rays. One patient had revision surgery due to symptomatic subsidence (29mms) at 6 months follow up. Subsidence does occur in the first 6 weeks in collarless Corail hip replacement, and to a lesser extent until 6 months postoperatively, but does not progress further.
INTRODUCTION
Total hip replacement (THR) is one of the most commonly performed elective Orthopaedic procedures in England [1]. Every year approximately 1 million patients undergo a THR. It is successful in restoring activity, mobility and alleviating discomfort in patients with end-stage arthritis of the hip [2].
The femoral component can either be cemented (Polymethylmethacrylate-PMMA) or cementless. The success of cemented femoral stems particularly in elderly osteoporotic bones has been well-documented [3, 4]. Cement fixation in young patients has been shown to have an increased rate of osteolysis and aseptic loosening [5]. Cement fixation occurs by microinterlock with endosteal bone. PMMA fatigue occurs with cyclic loading and is twice as likely to fail in men as compared to women.
Cementless fixation relies on biological fixation by bone growth into the prosthesis to secure the implant. This can be achieved either by bone ingrowth (porous coating) or bone ongrowth (grit coating). This biological integration between the stem surface and endosteal bone aims to decrease the incidence of aseptic loosening [6, 7]. It is ideally reserved for young active male patients requiring a total hip replacement.
Older patients with poor bone quality, Paget disease, certain inflammatory arthritis, tumor involvement, or postirradiation do not have good bone in growth potential and they might not be ideal candidates for cementless fixation [8]. However, some studies have shown that cementless fixation is successful in patients over 65 years with poorer bone quality [9-11].
Revision of loose prostheses can be a burden to the health service. It is a surgically challenging and expensive procedure. It is also associated with considerable patient morbidity [12]. Studies have shown that early subsidence of femoral THR prostheses predicts later aseptic loosening and implant failure which may require revision surgery [13, 14].
One of the most commonly used cementless stems is the Corail stem. The Corail stem is coated with hydroxyapatite [Ca10(PO4)6(OH)2]. The two types of Corail stems are collared and collarless stems. The collarless Corail system offers the high offset and standard stem. This is to permit adequate soft tissue tensioning and femoral offset restoration. The collared Corail femoral stems are available in both coxa vara and standard offset. The collared stem is used in poor quality bone to prevent subsidence. It may also add some amount of rotational stability in these patients.
The purpose of this study was to assess whether subsidence occurs in collarless Corail hip replacement (CCHR) and to ascertain the extent and timing of subsidence if present. We also evaluated its clinical relevance.
MATERIALS AND METHODS
The Corail femoral stem (DePuy Synthes) which was introduced in 1986 is a straight implant, with a quadrangular cross section that is made of forged titanium alloy (TiAl6V4). It has a flared proximal aspect in the coronal and sagittal plane. This is to enhance the three-dimensional stability in the proximal aspect of the femur. The lower end of the stem has a tapered construct to prevent medullary canal obstruction. This design also produces a stiffness gradient. It has vertical and horizontal grooves to improve primary mechanical stability. The entire surface of the stem is coated with hydroxyapatite (HA) to block release of metal ions. The thickness of the HA coating is 150 μm [15]. This is also to ensure optimal osseointegration with the endosteal surface thus preventing fibrous fixation especially around the lower aspect of the stem [15].
This was a retrospective case notes and radiograph analysis. We proceed with this study after obtaining approval from our local clinical governance department. We identified sixty-eight patients who had collarless Corail hip replacement over an eighteen months period. There were 32 male patients and 36 female patients. Their mean age was 74.2 years (range 37-95 years). Indications for surgery were osteoarthritis in 64 (94%) patients, rheumatoid arthritis in two (3%) patients and avascular necrosis in two (3%) patients.
All patients had a standard posterior approach to the hip and were followed up for a minimum of one year.
Inclusion Criteria
All patients who had a primary collarless Corail hip replacement
All ages
Minimum follow-up of one year
Exclusion Criteria
No minimal follow-up of one year
Pathological process in the hip
Not primary total hip replacement
Subsidence was measured at 6 weeks, 6 months and 1-year post-op compared to initial post-operative radiographs. Measurement was from the highest point of the greater trochanter to the highest lateral aspect of the femoral stem. All our radiographs were digital images. Measurements were computer assisted from our PACS system – (Picture Archiving and Communication System).
RESULTS
All patients were allowed to fully weight bearing as tolerated immediately post op. All patients had an immediate standard post op weight bearing AP pelvic radiograph prior to discharge. They were followed up at 6 weeks, 6 months and 12 months post total hip replacement with an AP standing radiograph. At 6 weeks x-ray 21 patients did not have any subsidence, 18 patients had 1 millimeter (mm) subsidence, 10 patients had 2mms subsidence, 4 patients had 3mms subsidence, 5 patients had 4mms subsidence, 1 patient had 5mms subsidence, 4 patients had 6 mms subsidence and 1 patient each had subsidence of 7mms, 9mms, 11mms, 13mms and 26 mms respectively (Table 1).
Subsidence at 6 weeks compared to initial post op radiographs.
| Subsidence in Milimeters | Patients (Percentage) |
|---|---|
| 0 | 21 (31%) |
| 1 | 18 (26%) |
| 2 | 10 (15%) |
| 3 | 4 (6%) |
| 4 | 5 (7%) |
| 5 | 1 (1.5%) |
| 6 | 4 (6%) |
| 7 | 1 (1.5%) |
| 9 | 1 (1.5%) |
| 11 | 1 (1.5%) |
| 13 | 1 (1.5%) |
| 26 | 1 (1.5%) |
When compared with 6 months x-rays only 2 patients had a further subsidence of 2mms while another patient had 3mms subsidence. No further subsidence occurred at 1 year follow up x-rays. All total hip replacements were performed by the consultant in charge or by the specialist registrar under the supervision of the consultant in charge.
One patient had revision surgery due to symptomatic subsidence (29mms) at 6 months follow up (Fig. 1). This patient had an initial subsidence of 26 mm at 6 weeks follow up. Her symptoms were hip and back pain due to leg length discrepancy and instability. She was 72-year-old lady with a background history of diabetes and chronic pulmonary airway disease on steroids, but was not diagnosed with osteoporosis. She was revised to a long collared stem.
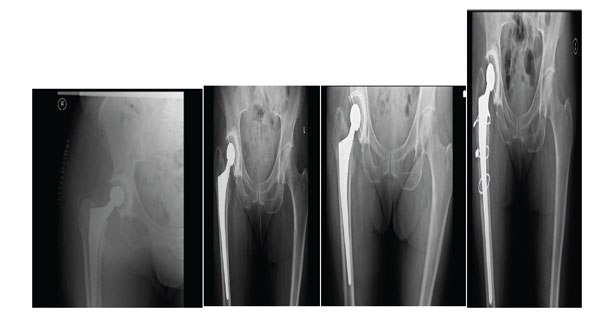
Initial post op, 6 weeks, 6 months and revision to long collared stem radiograph.
One patient had an intra-operative calcar fracture that was dealt with cabelling of the femur. This patient had only 1 mm subsidence at 6 weeks follow up. Another patient had an early post-operative infection that required a surgical debridement, washout and antibiotics for 6 weeks. One patient developed a deep vein thrombosis six weeks post op and was anticoagulated. The average length of hospital stay was 5.5 days (range 4-8 days). There were no patient deaths at last follow-up.
DISCUSSION
There have been advances in uncemented fixation, and stable osseointegration may be achieved through a hydroxyapatite (HA) coating on the stem. Hydroxyapatite (HA) has osteoconductive properties. Osteoconductive properties allow more rapid closure of gaps between bone and prosthesis. Osteoblasts adhere to HA surface during implantation and then grow towards bone. It has the capability to stimulate the attachment, migration and distribution of vascular and osteogenic cells within an implant. It has also been shown to result in better ingrowth of bone than with uncemented titanium stem alone [16-18]. The survival rates of fully coated HA stems have proven to be excellent. Data from the Norwegian Arthroplasty Register between 1987 and 2004 showed that the revision rate at 4.5 years was 1%, at 10 years was 2.4% and 4.9% at 15 years on a total of 5,130 fully hydroxyapatite coated femoral stems.
The Corail femoral stem which is a press fit femoral component has a 97% survivorship at 15 years [19]. The Corail stem is thought to have an excellent outcome due to its fully HA coated surface resulting in increased osseointegration and its tapered design which decreases proximal femoral stress shielding [20, 21].
Campbell et al. 2011 [22] reported a mean (range -0.23-3.71) subsidence of 0.58 mm at two years for the collarless Corail stem. These authors also reported subsidence to be confined to the first six months following implantation, which is a similar finding to our study. We only measured subsidence up to 1 year follow up. Campbell et al. [22] did not obtain 6 weeks radiographs. Most of the subsidence in our study occurred at the 6 weeks radiographs. Our study demonstrates that femoral stem subsidence was confined mainly to the first six postoperative weeks. Subsidence generally stabilized after this period. Only two patients had subsequent subsidence at 6 months compared to the 6 weeks radiograph in our study.
Strom et al. 2007 [23] showed that the majority of subsidence in a cementless stem occured within the first two postoperative months. There was no significant stem subsidence that occurred within the first week of implantation in their study.
A recent study has shown that although the degree of cyclic loading did not correspond with stem micromotion at two years, it showed that early unrestricted postoperative mobilization increases early subsidence [24]. Strom et al. [24] also reported that early postoperative subsidence of the cementless CLS stem (Centerpulse, Bern, Switzerland) was invariably followed by stabilisation of the implant. This supports the theory that early subsidence seen in CCHR is an effect of impaction rather than true subsidence due to implant instability.
All the CCHR stabilized despite the huge difference in early subsidence seen in our study, except one that required revision surgery. No particular risk factor or reason for subsidence was found in our group of patient. In our study we could not find a correlation between abnormal stem positioning and subsidence. Future studies should look at risk factors such as osteoporosis and smoking in stem subsidence.
Our study has some key strengths and limitations. The radiological data were assessed by an independent surgeon, eliminating any potential bias. The skill and experience of the surgeon and the surgical approach used are both known to have a large impact upon treatment outcome. Our single-centre study using just one approach eliminated some of these potential con-founders. This is a multi surgeon series. The main limitation of this study was its relatively low follow-up and no functional outcome scores were obtained. The UK National Institute for Clinical Excellence recommends a revision rate of ≤10% at 10 years as the current benchmark level for prosthesis selection for THA. A long term follow up would tell us the rate of revision in patients who had subsidence compared to those who did not have subsidence as early migration of prosthesis have shown to predict loosening and implant failure [13, 14].
From our study we can conclude that subsidence does occur in the first 6 weeks in collarless Corail hip replacement, and to a lesser extent 6 months postoperatively, but does not progress further. Patients with subsidence of up to 13mms were asymptomatic.
Hence we recommend:
- The patient be informed about subsidence when consent is taken
- Six week check radiographs must be considered mandatory
- Further prospective study with larger numbers and better measurement technique is needed.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


