RESEARCH ARTICLE
Treatment of Trochanteric Fractures with the Gamma3 Nail - Methodology and Early Results of a Prospective Consecutive Monitored Clinical Case Series
A.C. Unger*, 1, E. Wilde1, B. Kienast2, C. Jürgens1, 2, A. P. Schulz1, 2
Article Information
Identifiers and Pagination:
Year: 2014Volume: 8
First Page: 466
Last Page: 473
Publisher ID: TOORTHJ-8-466
DOI: 10.2174/1874325001408010466
Article History:
Received Date: 15/7/2014Revision Received Date: 18/11/2014
Acceptance Date: 23/11/2014
Electronic publication date: 29 /12/2014
Collection year: 2014

open-access license: This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
Abstract
Objectives:
There is only sparse data on clinical results and complications of the third-generation Gamma nailing system (Gamma3, Stryker). Therefore, we started a large multi-centre case series in 2008. The aim of this paper is to present the study design and early results of a single arm of a prospective, consecutive, monitored, post-market follow-up evaluation of Gamma3 nails.
Methods:
From September 2009 to January 2012, 154 consecutive patients with an average age of 80 ± 1.43 years (50-99 years) and a trochanteric femoral fracture were included in the local arm of the trial. All patients that fulfilled the inclusion criteria were treated with a Gamma3 nail. Preoperative variables included age, gender, fracture classification, walking ability (Merle d’Aubigné score), daily activity level (retrospective Zuckerman score), ASA rating of operative risk, waiting time for operation, use of walker or crutches and body mass index (BMI). Skin-to-skin time, fluoroscopy time, blood loss, intraoperative complications and device information were recorded for each patient. Follow-up postoperative assessment was undertaken at 4, 12 and 24 months. Hip range of motion, pain around the hip and the tight, walking ability (Merle d’Aubigné score, Sahlgrenska mobility score) and management of daily life (Zuckerman score) were used to evaluate the outcome.
Results:
The descriptive data of age, gender, BMI, ASA classification, fracture type and skin-to-skin time is similar to other studies. Median fluoroscopy time was 62 seconds (range: 4-225 seconds) and significantly shorter in closed reductions. No intraoperative implant-related complication was recorded. A cut-out of the leg-screw during assessment period occurred in 2.6% patients (n = 4). At the 12-month assessment two (1.8%) non-unions were identified and two patients (1.8%) had broken the femoral shaft below the 180 mm nail after a fall. Analysis of the scores showed significantly declined mobility and activity in daily life four months after operation which increased significantly from four to 12 months and increased slightly between 12 and 24 months after fracture.
Conclusion:
A low implant-associated complication rate was achieved in geriatric patients with trochanteric femoral fractures using the Gamma3 nail. A better outcome concerning mobility, activity in daily life and complications compared to the Gamma2 nail could not be found in comparison to historic data.
INTRODUCTION
Third-generation intramedullary devices for the treatment of trochanteric fractures have been introduced to the market by many manufactures. For example, a new version of the “Gamma nail” — the Gamma3 — was introduced to the market after various modifications in 2004. Although they are often used in daily orthopaedic work, studies with large numbers of patients with these implants are rare. Many studies compare external and internal fixation for trochanteric fractures, but almost all compare the second-generation Gamma nail with an external fixation system [1-5]. There are only a few clinical studies of the Gamma3 nail, of which Yaozeng published one of the first [6]. Heretrospectively compared 52 Gamma3 nails with 55 Proximal Femur Nails (PFNA). In 2009 Varela presented a prospective study of 80 patients with Gamma3 nails in correlation with the per-cutaneous Compression Plate (PCCP) [7]. The focuses of the study were intraoperative details and mortality rate. De Grave also published a randomised comparison of 112 patients who were treated either with a Gamma3 nail or with an ACE trochanteric nail [8]. None of these studies found clear evidence for superiority of any of the compared osteosynthesis forms.
The aim of this study, which started in 2006, was to collect prospective data of clinical results regarding the Gamma3 nail with special consideration to mobility and complications. This paper presents a consecutive case series of 154 patients from the Luebeck centre of the investigation, which has participated since 2009. We present the methods and early results of an international, prospective, sponsored (Stryker Trauma GmbH, Schoenkirchen, Germany) clinical investigation.
MATERIALS AND METHODS
Patients
All patients were screened directly after admission to hospital and before surgery. The inclusion and exclusion criteria were defined as follows:
Inclusion Criteria
- Adult men or women aged 50 years or older
- An extra articular fracture in the trochanteric area, classified by AO 31A1, 31A2, 31A3, 32A1, 32A2, 32B1, 32B2 confirmed with anterior and posterior lateral hip radiographs, computed tomography, or magnetic resonance imaging (MRI)
- Patients who understood the conditions of the international multi-centre prospective clinical follow-up evaluation and were willing and able to participate for the length of the prescribed term of follow-up
- Patients with the ability to walk prior to the accident, with or without walking aids
- Patients who gave written consent (signed the informed consent form).
Exclusion Criteria
- Patients who were reasonably unlikely to be compliant with the prescribed postoperative routine and follow-up evaluation schedule, as judged by the surgeon
- Associated major injuries of the lower extremity (i.e. ipsilateral or contralateral fractures of the foot, ankle, tibia, fibula, knee, or femur; dislocations of the ankle, knee, or hip; or femoral head defects or fracture)
- Patients with a physical condition (e.g. severe obesity) or neuromuscular deficit that interfered with the patient’s ability to limit weight-bearing, or placed an extreme load on the implant in the healing period
- Patients who had not signed an informed consent form.
During the period 1 September 2009 to 31 January2012 a consecutive group of 234 patients underwent screening; 154 patients were included in the study, totalling 44 male patients (28.6%) and 110 female patients (71.4%) (Fig. 1). The mean age was 80 ± 1.43 years (range: 50-99 years). The body mass index (BMI) had a mean value of 24.02 kg/m2with a standard deviation of 5.77 kg/m2 (range: 14.88-36.30 kg/m2).
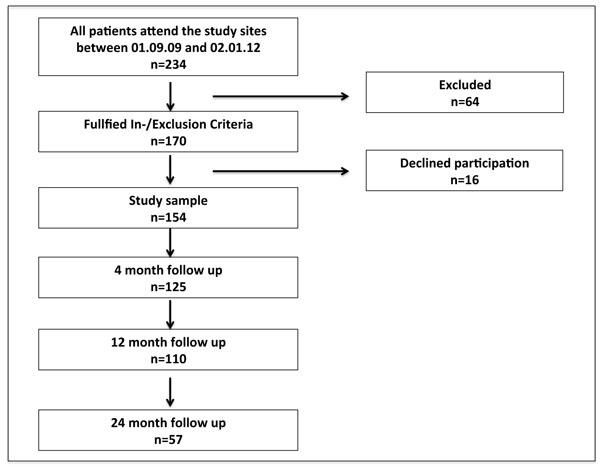 |
Fig. (1). Recruitment chart of study population, the follow-up is ongoing. |
Methods
The study centre of the cluster reported in this paper was a university hospital in northern Germany. External monitoring was performed. The acquisition of clinical investigation data was kept strictly independent from the study personnel by the assignment of a study nurse. Data was collected before the procedure, during the hospital stay, before discharge and after 4, 12 and 24 months. Some of the baseline values were retrospectively recorded to define the patient’s situation prior to the accident. The study follows the guidelines of the Declaration of Helsinki, including all amendments, and the rules of good clinical practice. Ethical approval was obtained from the local Ethics Committee. The study was registered in the German clinical trials registry (DRKS00004593).
Data included details about the implant, the procedure and living conditions before the procedure, relevant clinical data and Merle d’Aubigné, Zuckerman and Sahlgrenska scores. The objective was to evaluate the clinical and functional outcomes of treatment of trochanteric fractures with the Gamma3 nail, with particular focus on complications. Therefore, all data concerning complications (general/preoperative and device-related) were documented.
Functional Outcome Scores
The Merle d’Aubigné (MDA) score formed the basis of the hip scoring system that assessed pain, range of movement and walking ability [9]. The MDA score is a clinician-based mobility score, which consists of two parts: the first part asks two questions about current pain and functional status of the patient, with six possible answers each; the second part consists of arrange of motion (ROM) assessment. The MDA score is frequently used in the assessment of patients after hip fracture [10-14].
The Zuckerman score [15] measures activities of daily living and consists of ten questions with five possible answers each, ranging from ‘not at all’ (0 points) to ‘no difficulty’ (4 points). In this study we used Zuckerman score pre-operatively and at 4, 12 and 24 months after initial surgery. The Zuckerman score has been used in the past to assess patients with fractures around the hip region [16-19].
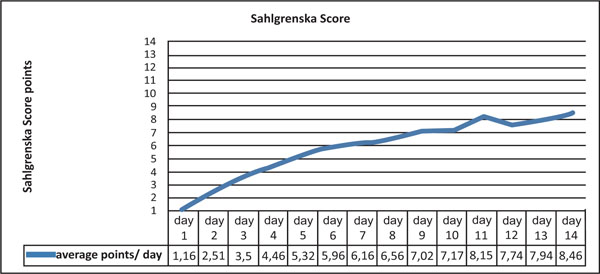
The Sahlgrenska mobility score is a new clinician-based mobility score to assess mobilisation within the first 14 days after surgery. It consists of a scale ranging from ‘bedridden’ (1 point) to ‘walking alone without any walking aid > 6 m’ (14 points). Therefore, a maximum score of 14 points can be achieved.
The device used in this investigation was the Gamma3 nail (Stryker, Schoenkirchen, Germany). Surgeons could choose between a trochanteric nail with a length of 180 mm or longer versions available with lengths280-460 mm. Cephalic-screw angulation was possible at120°, 125° or130°.
We used an internet-based electronic Case Report Form (eCRF) for data management. This electronic data-capturing (EDC) system is used for the capture, documentation and processing of data in clinical studies. The EDC system from XCLINICAL (XClinical GmbH, Munich, Germany) accords with the GAMP Guidelines. All data recorded in the eCRFs were consistent with the information reported in the patient’s hospital notes.
Statistical Analysis
Results obtained from the clinical investigations were collected in Excel 2008 and statistically analysed using SPSS (IBM Corporation, Armonk, New York, United States Version 20). For statistical analysis of continuous data all relevant descriptive parameters were tested for normality and homogeneity of variances. The non-parametric Mann-Whitney test was selected for comparison between two independent variables for non-normal data. The Wilcoxon test was used to compare paired variables. Categorical data was analysed by cross tabulation and Chi-square or Fisher’sex act test (2x2 tables) were used for comparisons. The level of significance for all tests was set to 95%.
RESULTS
Of 154 patients, 117 (76%) were living without help at home, 19 (12.3%) were admitted to hospital from a nursing home, 13 (8.5%) had extended care at home, two (1.3%) were admitted from hospital, one (0.6%) from a psychiatric institution and two (1.3%) from a rehabilitation ward. More than two-thirds of accidents (72.7%, n = 112) took place at home, followed by street accidents (17.5%, n = 27). In only four cases a high-speed trauma was the reason for the fracture (2.6%). Thirty-seven (24%) of the patients used a walking frame and 21 (13.6%) used one or two sticks prior to the accident. More than half of the patients (54.5%, n = 84) did not use any walking aid.
The majority of operations occurred within 24 hours (n = 119; 77.2%) and were done under general anaesthesia (n = 129; 83.8%). Closed reduction was possible in 82.5% (n = 127). Open reduction was necessary in 17.5% of cases (n = 27). More than half (n = 16) of the open-treated fractures were sub trochanteric fractures (p < 0.001). Nails of 180 mm length were used in 61.7% cases (n = 79) and of 320 mm length in 12.5% of cases (n = 16). The nail target angle was 125° in 93.0% of cases (n = 119). In 51 cases (54.3%), distal locking of short nails was performed statically, 43 (45.7%) were locked dynamically. Distal locking of long nails was static in 74.1%cases (n = 43). In four cases (2.6%), a secondary dynamisation after initial surgery was necessary.
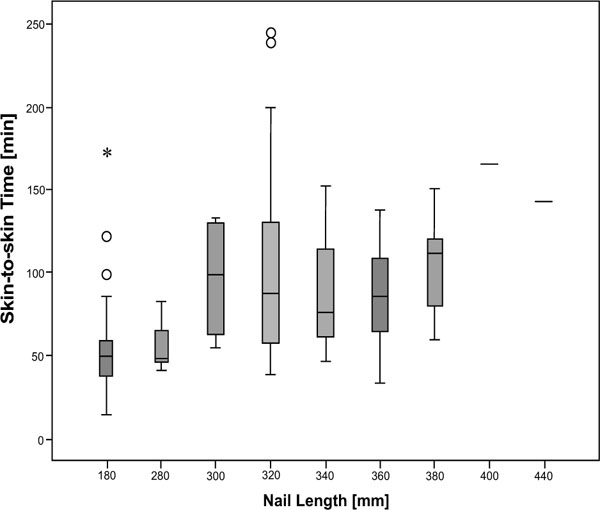
Skin-to-Skin Time
The median skin-to-skin time was 56.5 minutes with an inter quartile range (IQR) of 39 minutes. Skin-to-skin time was significantly shorter for short nails than for longer nails (p < 0.001; Fig. 2). Intraoperative blood transfusion was necessary in only 11.1% (n = 17) of cases; in the postoperative period this number increased to 14.3% (n = 22).
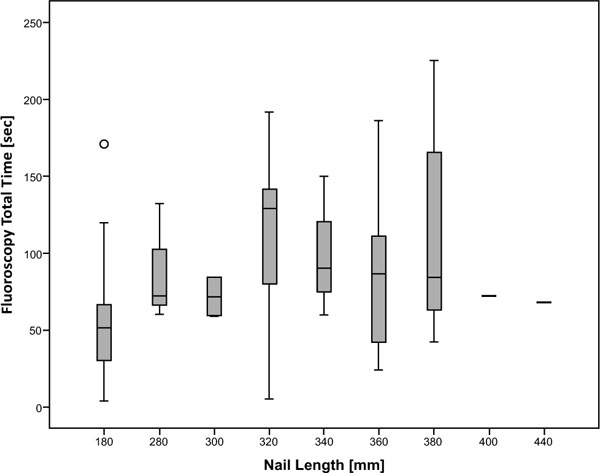
Median fluoroscopy time was 62 seconds (range: 4-225 seconds; IQR: 52 seconds). The fluoroscopy time was significantly shorter in closed reductions (p = 0.002; Fig. (3), Table 1).
Summary statistics on surgery, fluoroscopy, mortality and complication rate. Twelve patients (7.8%) developed serious general complications. Three patients (2%) died during hospitalisation, two because of pulmonary embolism and one as a result of a heart attack. Thirty-eight patients (24.7%) developed surgeryrelated complications during the overall study period (see Table).
| Variable | Measures | |
|---|---|---|
| Time to surgery (h) | Number | % |
| < 24 | 119 | 77.3 |
| 24-48 | 28 | 18.2 |
| > 48 | 7 | 4.5 |
| Closed reduction | 127 | 82.5 |
| Open reduction | 27 | 17.5 |
| Skin-to-skin time | Minutes (mean ± SD) | p |
| Short nail (180 mm) | 50 ± 21 | p < 0.001 |
| Long nail (280-400 mm) | 83 ± 43 | |
| Fluoroscopy | Seconds (mean ± SD) | p |
| Short nail (180 mm) | 51 ± 36 | p < 0.001 |
| Long nail (280-400 mm) | 83 ± 43 | |
| Mortality | Number | % |
| In hospital mortality | 3 | 2.0 |
| 1-year mortality | 17 | 15.4 |
| Overall mortality | 29 | 18.8 |
| Complications | Number | % |
| General | ||
| Fulminant pulmonary embolism | 2 | 1.3 |
| Cardiac complications | 6 | 3.9 |
| Neurological complications (perineal palsy/aphasia) |
4 | 2.6 |
| Falls | 10 | 6.5 |
| Surgical | ||
| Haemoglobin-relevant blood losses | 22 | 14.3 |
| Prolonged wound secretion | 10 | 6.5 |
| Cut-out lag-screw | 4 | 2.6 |
| Non-union | 2 | 1.3 |
Merle d’Aubigné Score
Before the operation, 87.0% of patients (n = 134) reported no pain retrospectively prior to their fracture, while two patients (1.3%) reported severe and spontaneous pain prior to the fracture. Nearly half of all patients (48.7%, n = 75) reported normal functional level before fracture. After 4 months 37.6% of the patients (n = 47) reported no pain, while 28% (n=35) experienced slight or intermittent pain. Severe and spontaneous pain was only reported by one patient (0.8%). As the study progressed there was a steady increase of patients reporting no pain (12 months: 51.8%, n = 57; 24 months: 61.4%, n = 35).
At 4- and 12-month assessments, patients showed a significant lower total MDA score for the fractured leg compared to the contralateral leg (4 months: p < 0.001; 12 months: p = 0.038), whereas at the 24-month assessment there was no significant difference in the total MDA score between fractured and contralateral legs (p = 0.128). At 4- and 12-month assessments patients had significantly lower ROM scores on the fractured side compared to the contralateral leg (4 months: p < 0.001; 12 months: p = 0.028), whereas at the 24-month assessment, there was no significant difference in ROM score between the fractured and contralateral leg (p = 0.13). Overall, patients approached their initial MDA measures of pain, function, ROM and total MDA in the fractured leg after 12 months.
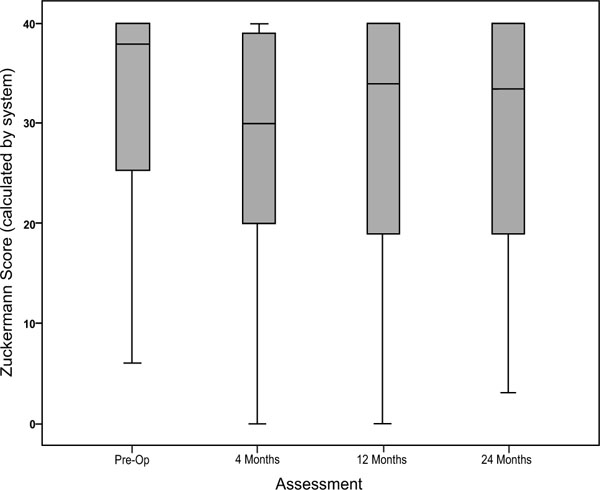
Zuckerman Score
The Zuckerman score decreased significantly (p < 0.001) from the patients’ situation before the accident (median 38 points, IQR 15, n = 154) to their 4-month assessment (median 30 points, IQR 19, n = 126). At the 12- and 24-month assessments the patients improved, with slightly higher median Zuckerman scores but still significantly worse than the pre-fracture score (p < 0.001) (Fig. 4).
Sahlgrenska Score
During the hospital stay, the Sahlgrenska score increased continuously in the first 11 postoperative days (1.16 to 8.15 points). Over the next four days to discharge from the hospital mobility remained at the same level (Fig. 5).
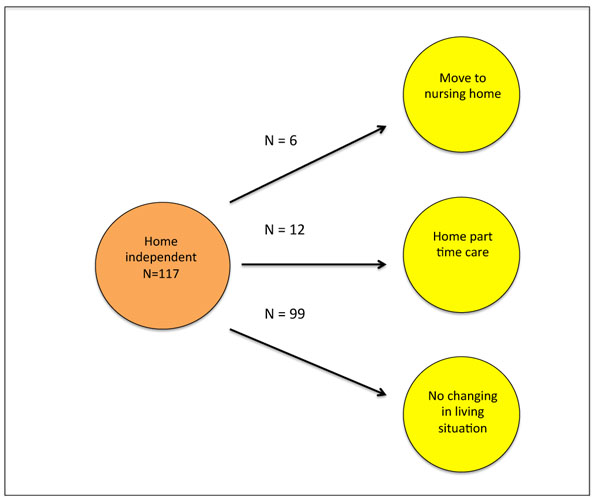
Most patients (85.9%; n = 132) were discharged to rehabilitation units, 20 (13%) to their nursing home and two (1.1%) returned home after surgical inpatient stay. Living situation changed for some of the patients after the accident. Changes in daily life, in particular regarding the need for help, are shown in Fig. (6).
Complications
During the overall study period, we recorded surgical adverse events in 24.7% of cases (n = 38; Table 1). At the 12-month assessment, two (1.8%) non-unions were identified. In both cases, the patients were more than 90 years old and clinically not affected. Surgical revision was not done. After 9 and 17 months two patients (1.3%) had each broken the femoral shaft below the 180 mm nail after another fall. In both cases open reduction and internal fixation with a long nail was performed.
Mechanical complications concerning the Gamma3 nail were recorded in four (2.6%) patients. All developed a cut-out of the leg-screw and had revision surgery. The nail and leg-screw were removed and a total hip arthroplasty was implanted.
The one-year mortality rate was 15.4% (n = 17). To date, the overall mortality rate during whole study period is 18.8% (n = 29). The median age of patients who died before completing their follow-up at 24 months post-surgery was 80 years (range: 53-98 years, IQR: 22). There was no significant difference in age between patients who died and patients who survived the complete follow-up period (median age: 80 years, range: 50-98 years, IQR: 16; p = 0.617). Equally there was no significant difference in mortality between males and females (p = 0.636).
DISCUSSION
We present the first results of an industry-sponsored clinical investigation together with details of the design of the investigation. A 24-month follow-up is planned with the inclusion of 450 patients. To date, outcomes achieved with the Gamma3 nail are equal to those of other modern intramedullary implants for fractures of the trochanteric area. The mortality rate at 12 months (15.4%) is low compared to other studies. Kammerlander et al. reported a one-year mortality rate of 23.2% in his retrospective follow-up on 281 geriatric hip fracture patients [20]. Buecking et al. had a 1 year mortality of 22.2% in their prospective, single-centre observation study of 90 patients who were treated with a Gamma3 nail for pertrochanteric and subtrochanteric femoral fractures [21]. In a prospective randomised trial comparing two different intramedullary nails in 112 geriatric patients with pertrochanteric femoral fractures, de Grave et al. found a one-year mortality of 23% [8]. The improving mortality rates are at least partially due to more modern anaesthetic techniques and faster rehabilitation schemes. A randomised trial comparing third-generation to second-generation implants would be required to test for an effect of the implant. Our descriptive data of age (78.5 ± 1.43 years) [2, 3, 6-8, 22, 23], gender (♀:♂ = 2:1) [2, 3, 6, 8, 24-26], BMI (24.52 ± 5.01), ASA classification [2, 24, 26, 27], fracture type (AO classification) [6, 8, 28] and skin-to-skin time [6-8, 24, 25, 29-32] were comparable to data reported in earlier studies of previous trochanteric nails of the second generation.
The Gamma3 nail used in this study needed less fluoroscopy screening time than other implants and Gamma2 nails [6, 24, 26, 27, 29, 33]. No implant-related complications occurred during the operations. Within the surgery-related complication rate during hospitalisation (20.8%, n = 32) most of the complications were haemoglobin-relevant blood loss, which occurred in 14.3% of patients (n = 22). In other studies the blood transfusion rate ranged from 33% to 50% [25, 26, 34]. During the follow-up period two (1.3%) femoral shaft fractures and four (2.6%) cut-outs of the lag screw occurred (Table 1). This rate is similar to other Gamma3 nail studies [8, 23, 35]. These early data cannot identify clear advantages of the third-generation nail regarding the most common complications. The rate of cut-outs of the lag screw in the Gamma2 model varied between 0 and 10% [14, 24, 25, 34, 36]. Mobility scores showed a significant decline four months after operation, especially in activities of daily living. The MDA score increased during the first 12 and 24 months of assessment, but did not reach the pre-fracture level. Utrilla and de Grave also noted a decreased mobility MDA score after trochanteric fracture [8, 26]. Buhl even found worsening mobility in 26.7% of patients [37]. The Zuckerman score showed a maximum decrease at the 4-month assessment, but increased significantly from four to 12 months, and continued to increase slightly between 12 and 24 months after fracture. The score was still significantly lower after the 24-month assessment compared to the score before the accident. Our results corresponded to those from Zuckerman [15]. Comparative results of the Sahlgrenska score are not available for this patient population.
Our study provides an impression of the trend of the whole multi-centre study data. The loss of independence in managing daily life four months after the Gamma3 nail operation can be noted in all of the assessed scores and is statistically significant. Complication rates and impairment four months after trochanteric hip fracture correspond with data in the literature. Typical complications of Gamma nail operations such as femoral shaft fracture and leg-screw cut-outs appear to be decreased.
CONCLUSION
The aim of the study was to collect data and analyse the changes in daily life regarding mobility and regaining independence after trochanteric hip fractures treated with third-generation Gamma nails. Our focus was to present the study design and descriptive data of intraoperative details and postoperative complication rates. The strength of the study is the clear design with strictly consecutive inclusion, external monitoring and the evaluation of implant behaviour. To date it is the largest study assessing the novel Gamma3 implant in daily clinical use. A limitation is the lack of proper quality-of-life data and an intention-to-treat design, assessing patients after revision surgery.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENT
The study is partially funded by Stryker Osteosynthesis, Schoenkirchen, Germany.