All published articles of this journal are available on ScienceDirect.
Modified Wilson’s Osteotomy for Hallux Valgus Deformity. A New Approach
Abstract
We introduce a new set of modifications and present the results from 48 patients (a total of 60 feet operated), who underwent this modified Wilson’s osteotomy for the correction of Hallux Valgus. Patients were of an average age of 52 years old (from 21 to 75 years of age) and were followed up for a mean of 12 months post-operatively. Patient evaluation was made with the symptom scoring system as presented by Kataraglis et al., with the final outcome being satisfactory in all of the cases. This set of modifications introduced to the original Wilson’s osteotomy, proved to offer a stable, predictable and satisfactory outcome in all cases and we strongly recommend it.
INTRODUCTION
Hallux Valgus represents a rather common deformity and a variety of operative procedures has been developed for its treatment [1]. Osteotomies of the first metatarsal have played a prominent role in the surgical management of hallux valgus deformities. Distal metatarsal osteotomies are usually preferred, together with remodeling of the medial exostosis and some form of soft tissue restoration and balancing technique. Wilson, in 1963, described an oblique osteotomy. His technique presented a simple and relatively stable way of displacing the metatarsal head, without the need for internal fixation. The broad osteotomy surfaces had reduced risk of nonunion, and the large metatarsal head fragment minimized the chances of avascular necrosis. The technique consists of an oblique osteotomy of the distal third of the first metatarsal, combined with remodeling of the medial exostosis. The line of the osteotomy starts on the medial side at the proximal end of the exostosis, extending laterally at an angle of 45°. The distal fragment is thus transferred and the remaining prominent shaft is removed after the osteotomy is in its correct alignment [2, 3].
Ever since, there have been a number of proposed modifications to the initial [4]. Helal et al. in 1974, changed the direction of the osteotomy by tilting it from a dorsal-distal position to plantar-proximal [5]. In 1976, Davis and Litman used Wilson's technique without the removal of the medial exostosis, which allowed the first metatarsopha-langeal joint to remain undisturbed [6]. Allen et al. also introduced modifications in 1981, mainly using a cancellous screw for rigid internal fixation [7]. Pittman and Burns, in 1984, altered the direction of the osteotomy from a proximal-medial to distal-lateral, to address hallux limitus by plantarly displacing the capital fragment [8]. The Telfer osteotomy forhallux valgus was introduced in 1985. It included modifications to the original Wilson’s oblique osteotomy at the neck of the first metatarsal head that produce a maximum lateral displacement of the distal fragment and retain the ideal position by means of rigid internal fixation [9]. In 1988, Klareskov et al. modified Wilson's osteotomy by plantar-flexing the first metatarsal head as it is shifted laterally. The plantar displacement of the distal fragment allows the first metatarsal to bear more of the weight-bearing forces, thus reducing excessive pressure on the lateral metatarsal heads [10]. Finally, some authors obviated the need for plaster cast immobilization even when using various types of internal fixation of the osteotomy [11-13].
In this paper we present the results from 48 patients who underwent Wilson’s osteotomy for hallux valgus with a set of concomitant modifications to the original technique.
PATIENTS AND METHODS
A number of 48 patients (a total of 60 feet), forty two women and six men, were retrospectively evaluated. All of them underwent the proposed modified Wilson’s osteotomy for Hallux Valgus deformity, from 1999 till 2011. Thirty six of the patients were operated on one foot and twelve bilaterally. Their mean age at the time of operation was 52 years old (ages varying from 21 to 75 years of age). All patients were followed-up for a mean of 12 months. Their main reason for the operation was regional pain (40% of the patients), inability to wear shoes (30%) and cosmetic reasons (30%). The prior to operation mean time of pain and disability varied from 4 to 50 years (on average 16 years). Preoperatively all patients were carefully examined for the possibility of osteoarthritis of the MTP joint (hallux rigidus) and if this was present a different type of operation was offered to them. It must be noted that patients which required extensive corrections of the forefoot were not included in the study group. Concomitant operations were limited to extensor tenotomies and/or arthrodesis of the 1st interphalangeal joint of lesser toes.
Surgical Technique
All of the surgical operations were performed by the same surgeon, under general or regional (spinal) anesthesia and with the concomitant use of a pneumatic tourniquet. The steps of the operation were as follows: A medial longitudinal skin section centered over the first metatarsophalangeal joint (Figs. 1, 2) was followed by a “Y”-shaped capsular incision and exostectomy (Fig. 3). Oblique osteotomy angled from
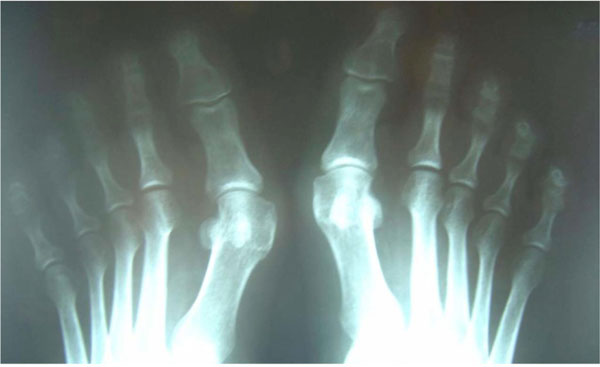
X-rays of the feet (AP): bilateral hallux valgus.

Skin incision.

Capsular flap elevated, exostectomy performed.
medially-distal to laterally-proximal, starting from the proximal end (base) of the exostectomy and additionally with a plantar inclination of 30º. It should be noted here that the osteotomy was performed with the use of a power saw, only. On the contrary, the exostectomy was always performed with the use of an osteotomy chisel (Figs. 4, 5). We consider that mishaps such as fracture of the metatarsal shaft or removal of excessive amount of bone from the metatarsal head can this way be avoided. The distal fragment was stabilized with the use of a K-wire inserted through the margin of the articular surface of the head of the metatarsal, with respect to the joint surface and advanced either intramedullarly in the shaft, or transfixing it. Next, trimming of the protruding bony edge of the proximal fragment with the use of a bone nibbler was performed and “Y-V” capsulorraphy with the use of interrupted absorbable sutures. Skin suturing and bandaging. The foot was kept elevated for 48 hours, after which heel weight-bearing was initiated. Skin sutures where removed after the second post-operative week and the K-wires were removed at approximately four weeks after surgery. Full weight bearing was routinely allowed on the sixth postoperative week. The patients were followed up both radiologically and clinically at six weeks (Figs. 6, 7), three months, six months and one year.

Positioning of saw for osteotomy. Note proximal and plantar direction.

Reduction of osteotomy for stabilization with k-wire.

Postoperative X-rays (AP).

(a, b) Postoperative X-rays (Lat). Note that proximal fragment slightly covers distal, to prevent it from dorsal displacement.
Radiology
There are 60 full sets of x-rays, both pre- and postoperative. On a regular basis anteroposterior (frontal) x-rays of the foot under stress (weight bearing) were performed, in order to calculate the Hallux Valgus Angle (angle between the axis of the first metatarsal and the axis of the proximal phalanx) and the First Intermetatarsal Angle (angle between the axis of the first and the second metatarsal) [14]. The same views were used to estimate the shortening of the first metatarsal after correcting the magnification factor, as was proposed and described by Zlotoff [15].
Review of Patients
All patients were reviewed by the same reviewer. Generally speaking, there have been proposed the AOFAS Hallux, MTP and IP scoring system [16,17] proposed by AAOS, the lower extremity functional scale (LEFS) and the scoring system used by Broughton and Winson presented with minor modifications by D. Kataraglis et al. [18] to evaluate patients pre- and post-operatively. In our study we used the scoring system of D. Kataraglis (Table 1), preferred for its simplicity to be completed accurately by all patients, and in addition we assessed the radiologic findings by measuring the above mentioned post-surgically achieved angles.
Symptom score (according to D. Kataraglis et al.).
| Grade 1 | Grade 2 | Grade 3 | |
|---|---|---|---|
| Cosmetic Appearance | Happy | Slight Reservation | Unhappy |
| Pain in first MTP joint | None | Occasional | On normal activities |
| Metatarsalgia | None | After> 3h walking/standing | After<3h walking/standing |
| Function/Activities | No restrictions | Slight Restriction | Severe restriction in daily activities |
| Shoes used | Any | Slight restriction | Difficulty in finding/only special shoes |
Excellent were considered the results of patients who achieved Grade 1 in all categories, good were considered the results of patients who achieved no more than two Grade 2 and no Grade 3 scores and poor were considered all the rest of the results. As far as the angles are concerned we collected and wrote the data to assess early relapse or overcorrection complications. In the same time all patients were examined for passive and active range of motion of the first metatarsophalangeal joint as well as for the presence of callosities under the head of any of the metatarsals.
Limitations of the Study
Our study presents limitations. The included number of patients is relatively small, but the exclusion criteria used were followed very strictly, with emphasis given on proper x-rays and complete x-ray series. Many patients were thus excluded. No comparative method was used as the authors’ intention was only to present objective and accurately measured results from this method. Still, the results obtained may hopefully be considered for future comparative studies. The follow-up time of the patients can be considered short. The measurements however, proved to be rather stable when reevaluated after one year. On the counter-part, all the results, as mentioned again, were calculated and recorded by the same reviewer-author, which adds to the reliability of the presented values.
RESULTS
Of the sixty feet, fifty two were graded as 1 and eight as 2. Complications such as osteonecrosis of the metatarsal head or non-union of the osteotomy were not observed. There was no dorsal displacement of the distal part of the osteotomy. In 28 feet, surgery for the lesser toes was also required, usually by means of extensor tenotomy or arthrodesis of the first interphalangeal joint due to hammer toe deformity. Shortening of the first toe was occasionally mentioned by the patients but this, generally, was not of major importance. Shortening of the second toe after arthrodesis of the PIP in cases of hammer toe deformity, always improved the cosmetic appearance of the foot. Skin necrosis around the surgical wound was met in four cases and was treated successfully non-operatively in all circumstances. All four patients had not complied with postoperative orders for foot elevation and skin necrosis was considered the result of excessive swelling. Residual swelling often persisted for up to three months but gradually disappeared with activity. The mean correction HVA angle achieved was 14.8º with a range between 10º and 25º and a mean correction of IMA was 7º ranging from 12º to 4º The radiologic findings remained rather stable throughout the follow-up (Table 2).
Results.
| Pat. | Sympt. Score, 3 Month | Sympt. Score, 6 Month | Sympt. Score, 12 Month | HVA Correction, Post Op | HVA Correction, 12 Months | IMA Correction, 12 Months | Shortening | Other Operations | Complications |
|---|---|---|---|---|---|---|---|---|---|
| 1 | I | I | I | 20 | 19 | 10 | 8mm | Arthrodesis | - |
| 2 | II | II | II | 22 | 17 | 12 | 9mm | Arthrodesis | - |
| 3 | I | I | I | 19 | 17 | 11 | 8mm | Tenotomy | - |
| 4 | I | I | I | 12 | 12 | 6 | 5mm | - | - |
| 5 | I | I | I | 17 | 16 | 10 | 7mm | Arthrodesis | - |
| 6 | I | I | I | 12 | 12 | 5 | 3mm | - | - |
| 7a | I | II | II | 14 | 14 | 7 | 5mm | - | - |
| 7b | I | II | II | 20 | 18 | 11 | 8mm | - | Skin Necr. |
| 8 | I | I | I | 14 | 13 | 7 | 6mm | Arthrodesis | - |
| 9 | I | I | I | 15 | 14 | 6 | 5mm | - | - |
| 10 | I | I | I | 17 | 16 | 9 | 7mm | Arthrodesis | - |
| 11 | I | I | I | 13 | 13 | 7 | 5mm | - | - |
| 12 | I | I | I | 18 | 17 | 8 | 7mm | Tenotomy | - |
| 13 | I | I | I | 14 | 14 | 6 | 5mm | - | - |
| 14a | II | II | II | 24 | 20 | 12 | 9mm | Arthrodesis | - |
| 14b | I | I | I | 12 | 12 | 6 | 4mm | - | - |
| 15 | I | I | I | 21 | 19 | 10 | 8mm | Arthrodesis | Skin Necr. |
| 16 | I | I | I | 16 | 16 | 8 | 7mm | Arthrodesis | - |
| 17 | I | I | I | 11 | 11 | 6 | 4mm | - | - |
| 18 | I | I | I | 15 | 13 | 7 | 6mm | Tenotomy | - |
| 19 | I | II | II | 17 | 16 | 10 | 7mm | Arthrodesis | - |
| 20a | I | I | I | 15 | 13 | 7 | 5mm | - | - |
| 20b | I | I | I | 14 | 14 | 6 | 4mm | - | - |
| 21 | I | I | I | 11 | 11 | 6 | 4mm | - | - |
| 22 | I | I | I | 24 | 21 | 10 | 8mm | - | - |
| 23a | I | I | I | 11 | 10 | 6 | 5mm | - | Skin Necr. |
| 23b | II | II | II | 24 | 19 | 10 | 9mm | Arthrodesis | - |
| 24 | I | I | I | 14 | 12 | 6 | 5mm | Tenotomy | - |
| 25a | I | I | I | 18 | 16 | 9 | 7mm | Arthrodesis | - |
| 25b | I | I | I | 15 | 14 | 7 | 6mm | Tenotomy | - |
| 26 | I | I | I | 17 | 17 | 8 | 7mm | - | - |
| 27 | I | I | I | 16 | 15 | 6 | 6mm | - | - |
| 28 | I | I | I | 18 | 18 | 8 | 7mm | Arthrodesis | - |
| 29 | I | II | II | 16 | 13 | 7 | 6mm | Arthrodesis | - |
| 30 | I | I | I | 10 | 10 | 4 | 4mm | - | - |
| 31a | I | I | I | 13 | 12 | 6 | 6mm | Tenotomy | - |
| 31b | I | I | I | 12 | 12 | 6 | 5mm | - | - |
| 32a | I | I | I | 20 | 19 | 10 | 8mm | - | - |
| 32b | I | I | I | 14 | 14 | 6 | 5mm | - | - |
| 33a | I | I | I | 15 | 14 | 7 | 6mm | Arthrodesis | - |
| 33b | I | I | I | 15 | 15 | 6 | 6mm | Arthrodesis | - |
| 34 | I | I | I | 14 | 13 | 6 | 5mm | Arthrodesis | - |
| 35 | I | I | I | 11 | 11 | 5 | 4mm | - | - |
| 36a | I | I | I | 10 | 10 | 4 | 5mm | - | - |
| 36b | I | I | I | 13 | 12 | 7 | 6mm | Tenotomy | - |
| 37 | I | I | I | 12 | 12 | 6 | 5mm | - | - |
| 38a | I | I | I | 13 | 12 | 6 | 5mm | Tenotomy | - |
| 38b | I | I | I | 14 | 14 | 7 | 6mm | - | - |
| 39 | II | II | II | 25 | 18 | 11 | 9mm | Arthrodesis | Skin Necr. |
| 40 | I | I | I | 11 | 10 | 5 | 4mm | - | - |
| 41a | I | I | I | 10 | 8 | 4 | 3mm | - | - |
| 42b | I | I | I | 13 | 12 | 6 | 5mm | - | - |
| 43 | I | I | I | 14 | 13 | 8 | 6mm | Tenotomy | - |
| 44 | I | I | I | 11 | 11 | 5 | 4mm | - | - |
| 45 | I | I | I | 12 | 11 | 4 | 4mm | - | - |
| 46a | I | I | I | 14 | 14 | 7 | 6mm | Tenotomy | - |
| 46b | I | I | I | 12 | 11 | 6 | 4mm | - | - |
| 47 | I | I | I | 11 | 10 | 5 | 4mm | - | - |
| 48 | I | I | I | 17 | 16 | 8 | 7mm | Tenotomy | - |
(HVA and IMA values are presented in degrees and represent [preoperative value – postoperative value]).
DISCUSSION
As a clinical entity, hallux valgus is a disorder of the forefoot for the correction of which numerous techniques have been proposed. The rational indicates that no single technique can be used to address all the degrees and complex deformities of the forefoot, this opinion represents the opinion of the writers, too. As so, modifications to basic techniques have been proposed by various authors, which address the weak points of each technique and can be used to increase the effective range of deformities they can correct. The proposed set of modifications is the result of study and experience. Most of them are being used or have been proposed as parts of other techniques but haven’t been performed as a combined set with Wilson’s osteotomy. Wilson’s osteotomy has been selected as the base technique, because of its ease to perform. It has a relatively predictable post-operative behavior and has been well studied [19, 20]. As a nature it can be used effectively to correct 25-40 degrees of Hallux Valgus Angle and 12-16 degrees of First Intermetatarsal Angle. It is a broad osteotomy, requiring little stabilization, although it is inherently unstable. It is oblique thus has a reduced risk of nonunion, and retains a large distal fragment thus providing a low risk of avascular necrosis. Our proposed modifications address the weak points of Wilson’s initially proposed technique. The incision runs medially in the internervous plane and provides good exposure of the bunion and capsule and good aesthetic result. The plantar tilting of the osteotomy provides an even larger contact surface for the osteotomy and prevents the distal fragment from displacing dorsally, which resulted in “sticking toe” deformity [21] and also increases the weight bearing forces received, decreasing this way the strain on the rest of the heads of the metatarsals in a similar sense as proposed by Klareskov et al. [22]. The stabilization via k-wire both addresses the inherent instability of the osteotomy and reduces the excessive shortening of the metatarsal which is a common cause of metatarsalgia especially of the 2nd metatarsal [20]. The “Y-V” capsulotomy and capsuloplasty, allows for “fine” adjustment of the corrections and further increases the stability of the area. These modifications resulted in a relative stability post-operatively which did not necessitate plaster, or other means of stabilization [23]. Thus, patients initiated heel weight bearing as soon as pain allowed (encouraged to do so from the 2nd post-operative day), resuming simple daily activities fairly quickly.
The selection of an appropriate technique for the treatment of forefoot malformations related with hallux valgus has been a topic of debate with mid-shaft osteotomies, e.g. Scarf, gaining many supporters, mainly due to the increased range of HVA and IMA it can address. It is generally accepted that it is very technically demanding, with a long learning curve, and difficult to treat complications. Its results remain comparable to the simpler Chevron osteotomy for the same range of angles [24]. Also the results of proximal Chevron osteotomy over distal, have been comparable, but the risk of avascular necrosis on a long term remains to be determined [25]. A comparative study between unmodified Wilson’s osteotomy and Mitchell’s osteotomy [26], concluded that shortening was more frequent with Wilson’s osteotomy, thus adding to the known opinion that more than 10mm shortening is usually poorly tolerated and is associated with future metatarsalgia [27], but that is the main weak point of Wilson’s. This is one of the main reasons the writers of this articles consider very important the stabilization of the osteotomy.
CONCLUSION
Hallux valgus deformity is a very frequently encountered clinical entity in orthopedic practice. A vast number of surgical techniques have been proposed to correct the deformity and indications have been proposed for the selection of the appropriate technique according to each case. Special anatomic plates and power tools have been introduced and surgical skill requirements have vastly increased in time.
Wilson’s osteotomy with the proposed modifications is a technically straightforward approach, requiring minimum and easily accessible surgical tools and materials and has provided predictable and well accepted results in our practice. We consider it gives a foothold, even for young orthopaedists, to address a good range of hallux valgus deformity patients and we strongly recommend it.
CONFLICT INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


