RESEARCH ARTICLE
Reverse Total Shoulder Replacement with Minimal ACJ Excision Arthroplasty for Management of Massive ACJ Cyst - A Case Report
Shahril R Shaarani*, Hannan Mullett
Article Information
Identifiers and Pagination:
Year: 2014Volume: 8
First Page: 298
Last Page: 301
Publisher ID: TOORTHJ-8-298
DOI: 10.2174/1874325001408010298
Article History:
Received Date: 1/12/2013Revision Received Date: 20/8/2014
Acceptance Date: 25/8/2014
Electronic publication date: 24 /9/2014
Collection year: 2014

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.5/) which permits unrestrictive use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Massive acromioclavicular joint (ACJ) cysts are an extremely rare cause of shoulder impairment and with limited consensus in its management. We present the first published case report of a patient with a massive ACJ cyst treated with a reverse total shoulder replacement with minimal ACJ excision arthroplasty.
INTRODUCTION
Acromioclavicular joint (ACJ) cysts are extremely rare presentations of abnormal shoulder pathology. Depending on the aetiology of the cyst formation, this can impair patients’ cosmetic appearance as well as activity of daily living. There is no general consensus regarding management of this condition, as surgical excision has shown to have a mixed recurrence rates [1, 2]. We present the first published case report of a patient with a massive ACJ cyst treated with a reverse total shoulder replacement and minimal ACJ excision arthroplasty.
CASE REPORT
KM is an 83-year old right hand-dominant female who presented to the outpatient department with a six-year history of a right shoulder pain and swelling. She complained of a prominent lump over her right shoulder that was increasing in size, and pain restricting her range of movement (ROM). She had no previous treatment prior to her surgery. Her past medical history includes hypothyroidism and hypertension.
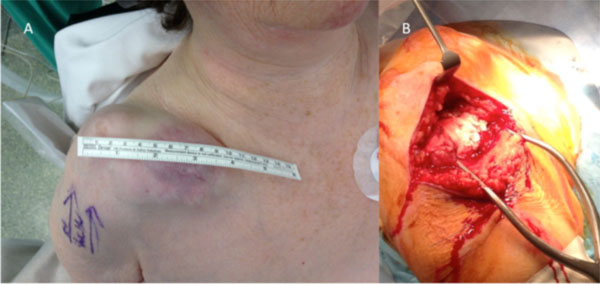
Clinical examination demonstrated a 10 x 6 x 2 cm multiloculated shoulder lump overlying the ACJ, with a globally reduced ROM consistent with rotator cuff arthropathy. Radiographs showed severe degeneration of the glenohumeral (GH) joint and proximal humeral head migration (Fig. 1). There was a lobulated soft tissue mass projected superior to the acromioclavicular joint, with moderate degenerative changes in the ACJ. Magnetic resonance imaging demonstrated a longstanding chronic full-thickness rotator cuff tear with complete atrophy of the supraspinatus and infraspinatus muscles, and of the subscapularis muscle (Fig. 2). The cyst communicates directly with the markedly degenerated GH joint on the T2-weighted MRI images.
The patient proceeded to a reverse total shoulder replacement (RTSA) following informed consent. A beach chair position was used and an antero-superior approach of the shoulder was utilised (Fig. 3a). There was a “bald head” of the humerus as there was complete tear of the rotator cuff with loss of contour of the humeral head. The ACJ cyst was documented with expression of a yellowish cheesy-like material, following the skin incision and accidental tear of the lateral aspect of the lobulated cyst. This was preceded with an ACJ excision arthroplasty (Fig. 3b). The humeral head was excised and both the glenoid and humerus were adequately prepared. A DePuy Delta CTA™ Reverse Shoulder System (Warsaw, Indiana, USA) was inserted with Palacos® (Zimmer, Warsaw, Indiana, USA) bone cement for humeral fixation. Intraoperative shoulder ROM was stable in all directions. The ACJ cyst was decompressed by the end of the procedure, with no further intervention intra-operatively besides copious wound irrigation. The rotator cuff was tagged using 2-0 Ethibond (Ethicon, Somerville, New Jersey, USA) to the best-approximated position due to its chronicity. Wound closure was with 2-0 Vicryl (Ethicon, Somerville, New Jersey, USA) subcutaneously and 3-0 Serafast (Serag-Wiessner, Naila, Germany) subcuticularly.
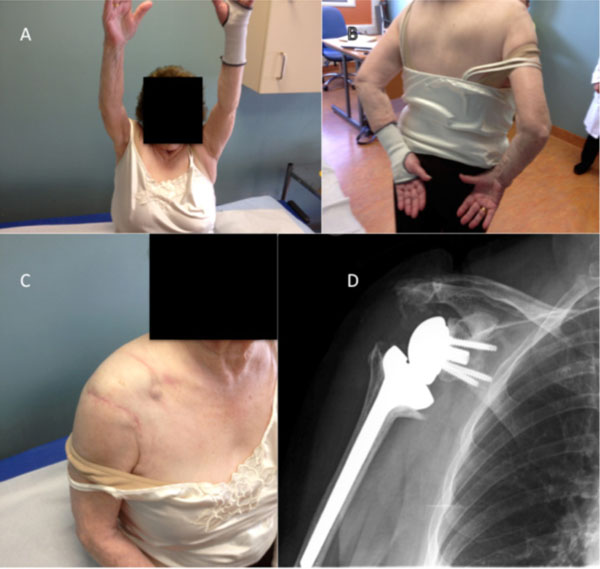
At 6-month follow-up, the incision was well healed with remission of the cyst. The patient had no pain symptoms and had excellent ROM (forward flexion 180°, abduction 120°, internal rotation to level of 4th lumbar vertebrae) and post-operative radiograph showing the prosthesis in satisfactory position (Fig. 4).
DISCUSSION
There is limited evidence in the management of giant ACJ cyst as this condition is rare. However, the general consensus is to resolve the underlying shoulder pathology [3]. This is the first case report that combined RTSA with an excision ACJ arthroplasty for this condition.
Hiller et al. classified the cyst depending on its aetiology: (i) type 1 ACJ cyst which can form superficially, with an intact rotator cuff and no communication with the GH joint (ii) type 2 ACJ cyst which follows a massive rotator cuff tear, followed by increased intra-articular synovial fluid production, proximal migration of the humeral head, erosion of the ACJ and a Geyser fluid migration from the GH joint into the ACJ superiorly [4]. The majority of cases published in current literature are mainly type 2 cysts, with 8 times increased incidences [4]. However there could be a publication bias due to the rarity of this condition. The patient presented in this case report has a type 2 ACJ cyst, with significant pain and reduced ROM which proceeded to her planned surgery.
The “Geyser sign” was first described by Craig et al. in 1984 following a shoulder arthrogram in a patient with ACJ cyst with a rotator cuff tear [5]. This sign was due to the leakage of contrast from the GH joint into the subdeltoid bursa due to the presence of a tear in the inferior articular capsule in the ACJ. Other modality of investigation such as ultrasound is more accessible but operator dependent [6]. The advent of MRI has modernised this sign radiologically, as T2 or proton-density weighted sequence would demonstrate bright signal changes from the synovial fluid extravasation without the need of a contrast. Ultrasound has a better ability in distinguishing partial tear of the rotator cuff when compared to MRI [7]; but MRI would be essential when the rotator cuff is not easily visualised or to exclude any malignancy [8].
The management options of ACJ cyst in the literature include conservative measures, aspiration, excision of the cyst with concurrent repair of the rotator cuff tear, ACJ excision arthroplasty, and shoulder hemiarthroplasty (humeral head replacement). There are only 2 reported cases of spontaneous remission of the cyst [9,10]. Aspiration and simple cyst excision is frequently unsuccessful due to failure to correct the underlying rotator cuff pathology [11-13]. There has been only one report of successful arthroscopic treatment with an irreparable rotator cuff [14]. The cyst was decompressed arthroscopically followed by ACJ excision arthroplasty to remove the pinch valve effect [14]. The evidence would show a benefit in removing this pinch valve effect by excising the distal clavicle [2, 12, 15]. Shoulder hemiarthroplasty is also an acceptable surgical option for cuff tear arthropathy due to patients’ symptoms [12]. Interestingly in this hemiarthroplasty case series, no operative procedure was directed on the ACJ and the cyst demonstrated a complete resolution at mean follow-up of 27 months [12]. Furthermore, Skedros et al. managed their patient primarily with resection of the ACJ cyst only without addressing the end-stage rotator cuff arthropathy [16]. This resulted in their patient to have unresolved shoulder pain and restricted ROM postoperatively to approximately 90 degrees forward flexion. Hence in our case report the patient proceeded to a RTSA in combination with a minimal ACJ excision arthroplasty.
The reverse geometry total shoulder replacement is biomechanically more stable as it provides an efficient fulcrum and decreases the shearing forces at the glenoid-bone interface when compared to other total shoulder arthroplasty techniques [17]. The functional shoulder score, pain symptoms and active elevation were significantly better in RTSA compared to hemiarthroplasty when treating for rotator cuff arthropathy [18]. Patient selection is crucial as RTSA is reserved for the more elderly patients above 70 years of age with low-demand activities, pseudopareisis of the shoulder with incapability to abduct above 90° and functional impairment not alleviated by nonoperative measures [3]. The antero-superior approach to the humeral head during RTSA serves two functions: (i) it increases the exposure preceding resection of the humeral head (ii) it further proceeded to the ACJ excision arthroplasty which removes the pinch-valve effect of the giant ACJ cyst as stated by Mullet et al. [14]. Hence RTSA resolves the glenohumeral arthritis with the irreparable rotator cuff as well as permanently decompressing the giant ACJ cyst through a single skin incision.
CONCLUSION
To our knowledge we describe the first case of RTSA with minimal ACJ excision arthroplasty in the setting of a massive ACJ cyst with improvement of patient’s symptoms and ROM. The reverse geometry design has been reintroduced as a treatment of rotator cuff athropathy. In this case, RTSA was combined with minimal ACJ excision arthroplasty to increase shoulder ROM and to decompress the giant ACJ cyst through a single antero-superior skin incision. The data for long-term functional outcomes for RTSA are still emerging, however this is a viable option for this rare condition.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.