All published articles of this journal are available on ScienceDirect.
Inflammatory Bowel Disease, High-Dose Steroids, Osteoporosis, or an Oncological Etiology for a Pathological Femoral Neck Fracture in a Young Adult: A Case Report
Abstract
Femoral neck fractures occur in approximately 6,000 of young adults annually (ages 18-49) (1). Of these, a high-energy traumatic event is the typical cause. Although medications and chronic diseases have been implicated as confounding causes of hip fractures, clinicians should have a high index of suspicion for an oncologic etiology of hip fractures occurring in young patients without an inciting traumatic event.
Study Design:
A case report and literature search in the English language.
INTRODUCTION
Femoral neck fractures occur in approximately 6,000 of young adults annually (ages 18-49) [1]. Of these, a high-energy traumatic event is the typical cause. Femoral neck fractures not related to trauma are uncommon in healthy young patients. In the case below, a patient with multiple medical comorbidities and long-standing osteoporosis due to high-dose corticosteroid use sustained a low-energy hip fracture. This case report reviews the medical and surgical decision making process that occurred, and the missed diagnosis of metastatic adenocarcinoma that caused the hip fracture.
CASE
A 29 year-old African-American female presented late one evening to a community hospital emergency department with severe right hip and groin pain. She stated the pain occurred during ambulation at a local store. She denied any trauma, but stated that the pain caused her to fall to the ground. She reported a three to four week history of groin and thigh pain for which she had been evaluated at a tertiary center emergency department three weeks earlier. At that time, radiographs were performed of the pelvis, hip, and sacroiliac joints (see Fig. 1). She was diagnosed with a ‘hip strain’ and referred to outpatient physical therapy and primary care physician follow-up.
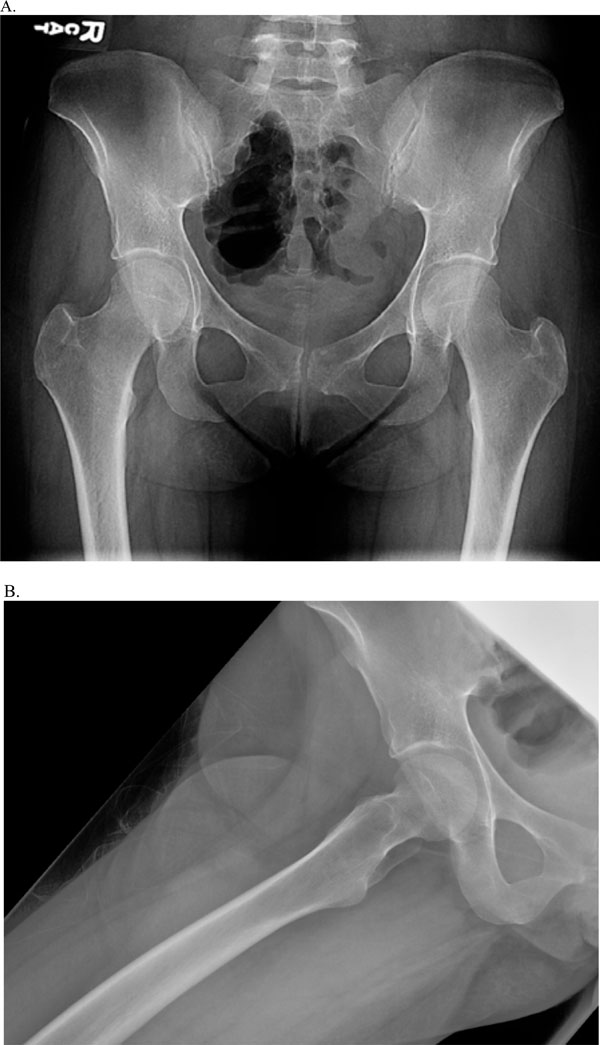
AP (A) & lateral (B) views of the pelvis and right hip 3 weeks prior to current ED presentation.
She had seen her primary care physician just prior to this current emergency department visit and admitted to receiving corticosteroid injection in the right trochanteric bursa for suspected trochanteric bursitis. Radiographs at the time of the current ED presentation are seen in Fig. (2).

AP (A) & lateral (B) views at the time of current presentation.
PAST MEDICAL HISTORY
The patient had a complex past medical and surgical history as summarized in Fig. (3). Of particular clinical significance, she was diagnosed with ulcerative colitis at age seven, and had a long history of using high-dose oral corticosteroids for flares of this disease. At age 24, the patient was diagnosed with osteoporosis via Duel-Energy X-ray Absorptiometry (DEXA) scan despite vitamin D, calcium, and bisphosphonate use. At age 28, the patient underwent total proctocolectomy. Vitamin D deficiency was diagnosed and she was treated with weekly high-dose vitamin D replacement and then with daily vitamin D supplementation.
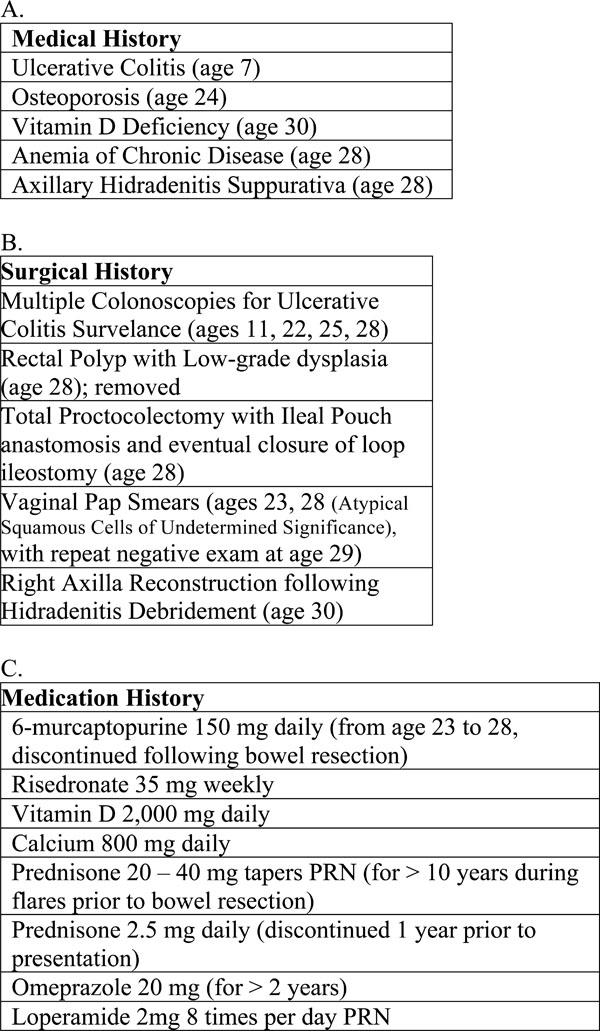
Past medical (A), surgical (B), and medication (C) histories.
The patient had a Body Mass Index of 23 prior to her ED presentation, however she complained of losing approximately 15 pounds over the last 12 months. The patient’s outpatient gastroenterology team felt the weight loss to be related to her bowel surgery and dysfunctional eating habits. HIV and other potential infectious etiologies were tested as an outpatient prior to presentation and were negative.
EMERGENCY ROOM MANAGEMENT
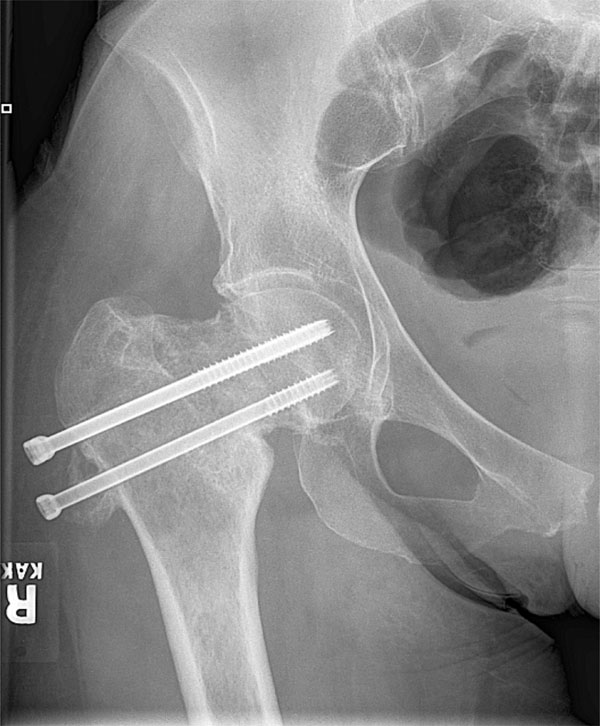
While in the emergency room, the patient initially had a CT scan of her right hip that revealed a minimally displaced femoral neck fracture as seen in Fig. (4). The orthopedic service was notified and x-rays were ordered to accompany these CT images as seen in Fig. (2). The diagnosis of a Pauwels type 2 [2,3] partially displaced femoral neck fracture was made and the patient was taken to surgery within 12 hours of presentation. Gentle closed reduction with a Leadbetter manuerver [4] was performed and a percutaneous pinning of the right hip was done on a fracture table utilizing 6.5 mm cannulated screws in a reverse-triangle orientation (see Fig. 5).

Coronal (A) and Axial (B) CT images at the time of presentation.

AP (A) and lateral (B, C) intraoperative fluoroscopic views during pinning surgery.
The patient went on to have an uneventful hospital course and was discharged to home three days after presentation. She was instructed to remain nonweight-bearing to the right lower extremity. The patient was followed in two-to-three week intervals, and at the six week follow-up visit, the patient had little to no groin pain with active and passive range of motion to the right hip.
The patient progressed to partial weight bearing at the eight week post operative visit and progressed to weight bearing as tolerated at the 12 week visit. Nearly complete resolution of symptoms had occurred, although some complaints of a persistent limp was noted. Some mild settling of the fracture was seen on serial radiographs, however, no signs of avascular necrosis of the femoral head were appreciated (see Fig. 6). At approximately 6 months after surgery, formalized physical therapy was initiated for persistent limp and weak abductors, and the patient remained off work.

AP (A) & lateral (B) x-rays at 6 months post operatively.
By the seven month post operative visit, the patient reported increasing pain and radiographs at that time were concerning for either a nonunion or infectious process (see Fig. 7). Triphasic technetium-99 bone scan was performed and revealed increased uptake in the entire proximal femur. Differential diagnosis included nonunion, refracture, or infection. Subjective signs and symptoms as well as laboratory values (serum white blood cell count, erythrocyte

AP (A) & lateral (B) views 7 months post op showing mottled bone within the femoral neck.
sedimentation rate, C-reactive protein) did not reveal any signs of infection. An MRI was ordered and can be seen in Fig. (8). This revealed a marrow-replacing lesion in the proximal femur. Biopsy by the oncologic team proved to be metastatic adenocarcinoma of unknown origin, and the patient underwent removal of hip hardware and conversion to a cemented bipolar hemiarthroplasty.
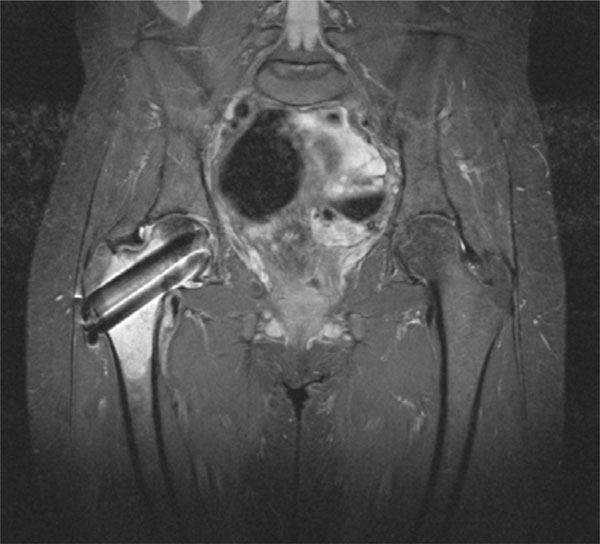
A Coronal T2 weighted STIR image demonstrating an 8.9cm by 3.8cm marrow replacing lesion of the proximal right femur.
DISCUSSION
The patient in the above case presented to our emergency department with a low-energy hip fracture. At the time of initial treatment, the patient’s hip fracture was thought to be due to her long-standing osteoporosis from high-dose corticosteroid use for the treatment of her ulcerative colitis. Long-term use of steroids leading to osteoporosis and increased risk of fractures has been well documented in the literature [5-7]. Gasterointestinal diseases in childhood have also been implicated as a cause of osteoporosis [8]. Following bisphosphonate treatment, the patient continued to have DEXA scans showing osteoporosis despite normal calcium and vitamin D levels [9].
In addition to corticosteroid use, the patient had a history of using proton pump inhibitor (PPI) medications for several years prior to presentation. Although controversial, there appears to be an association between prescription-strength PPIs and fractures, particularly in women or in those with other risk factors for fracture [10-14].
Although the patient’s hip fracture was initially treated appropriately (near anatomic reduction, stabilization within 12 hours, three cannulated screws in the reverse-triangle configuration, tip-to-apex distance less than 25 mm), [15-23] a high index of suspicion should have prompted further investigation into the etiology of the fracture. A review of the literature reveals several instances of low-energy avulsion fractures and hip fractures in the young adult,
however the majority of these cases are due an oncologic process, especially in patients with no traumatic event [24-33].
OUTCOME
The patient had a full oncologic workup, including CT scans of the chest, abdomen, and pelvis, as well as ultrasounds of the abdomen, ovaries, and breasts. Mammograms revealed biopsy proven calcifications with no signs of breast carcinoma. Radiation treatment of the right hip was initiated to prevent further bony destruction. Initially the patient did well, but pain and hardware failure occurred six months following radiation treatment (see Fig. 9) and cemented bipoloar hemiarthroplasty was performed by the orthopaedic oncologic team (see Fig. 10). The patient has continued multispecialty surveillance of her adenocarcinoma of unknown origin by the general surgery and gastroenterology teams with no other lesions or progression being noted.
AP x-ray of the right hip several months after radiation therapy.
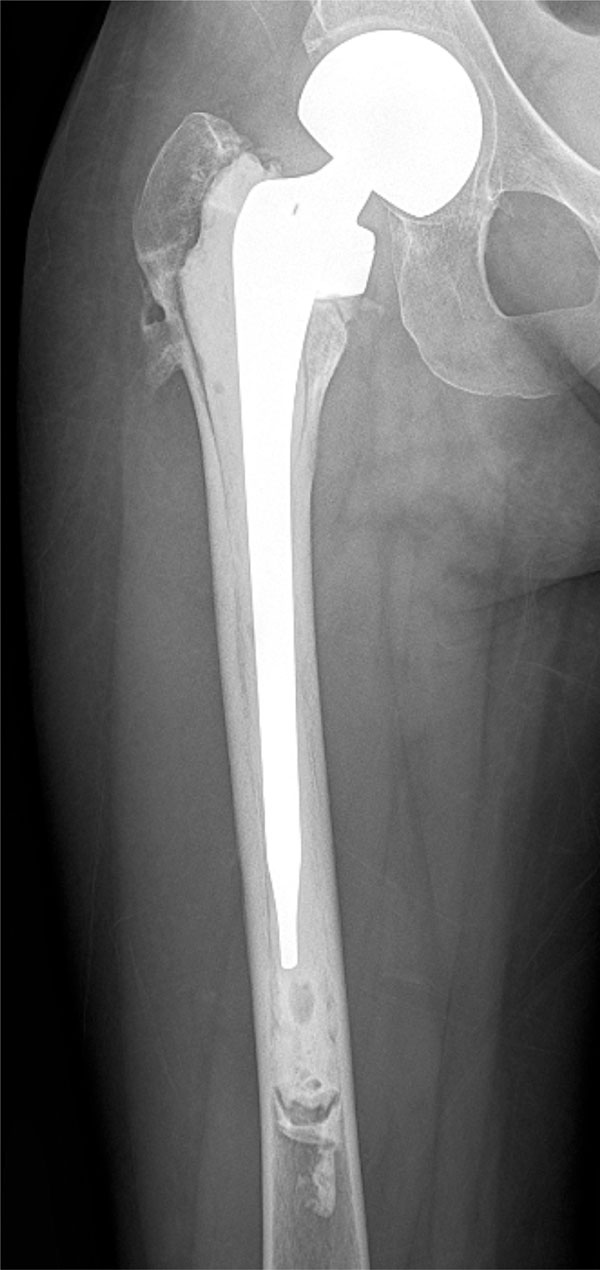
AP of the right hip following hemiarthroplasty surgery.
CONCLUSION
The case presented above describes an unusual presentation of a non-traumatic hip fracture occurring in a young adult. Although initially treated appropriately, a higher index of suspicion for a possible oncologic process, as well as a more thorough radiographic workup with an MRI of the hip should have been completed.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


