All published articles of this journal are available on ScienceDirect.
A Review of Management Options for Proximal Humeral Fractures
Abstract
Proximal humeral fractures are common and although the majority can be managed non-operatively, the optimal treatment of displaced or complex fractures remains controversial. Non-operative treatment is typically selected for minimally displaced fractures where union rates are high and good or excellent outcomes can be expected in approximately 80% of cases. The aims of surgical fixation are to restore articular surface congruency, alignment and the relationship between the tuberosities and the humeral head. Hemiarthroplasty provides patients with reliable pain relief and its indications include fracture dislocations, humeral head splitting fractures and some three- and four- part fractures. The key areas of surgical technique that influence functional outcome include correctly restoring the humeral height, humeral version and tuberosity position. Function, however, is poor if the tuberosities either fail to unite or mal-unite. The interest in reverse shoulder arthroplasty as an alternative option has therefore recently increased, particularly in older patients with poor bone quality and tuberosity comminution. The evidence supporting this, however, is currently limited to multiple case series with higher level studies currently underway.
INTRODUCTION
Proximal humeral fractures account for 10% of all fractures [1] and the incidence is rising [2]. Although the majority of minimally displaced fractures are successfully managed non-operatively [3] the optimal management of displaced or complex fracture remains controversial. Difficulties arise due to the risk of devascularisation of the humeral head, associated injury to the rotator cuff and the high prevalence of osteoporosis in the fracture cohorts. Current evidence has been unable to definitively conclude between prosthetic replacements, intramedullary nails, fixed-angle locked plates and conservative methods [4, 5]. A recent questionnaire of European surgeons demonstrated a trend towards surgical treatment but no consensus existed over the choice of surgical technique [6].
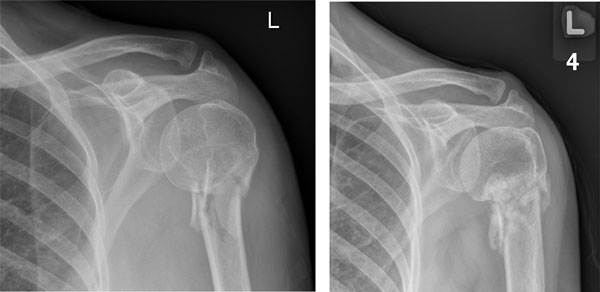
These injuries are commonly classified according to the Neer classification [7] that describes four fracture fragments: humeral head, humeral shaft, greater tuberosity and lesser tuberosity. Displacement is defined as either more than 1cm or 45° angulation. The classification is made according to the number of fracture fragments that are displaced and not the number of fracture fragments present, which may differ. Examples are given in Fig. (1). An alternative classification from the AO/OTA group is based on fracture location and status of the surgical neck, which aims to reflect the likelihood of an intact blood supply to the humeral head [8]. However, neither system has the ability to predict the ideal treatment option and both have poor intra- and inter-observer variability [9-11].

Proximal humeral fractures according to Neer Classification a) One part b) Two part c) Three part d) Four part.
An understanding of the vascular supply to the humeral head is crucial when planning surgical treatment. A fracture pattern which places the humeral head at risk of avascular necrosis may be more likely to benefit from arthroplasty surgery rather than internal fixation compared to a pattern whereby the risk of devascularisation is low. The principal blood supply to the head has been shown to originate from the anterior humeral circumflex artery through the arcuate branch [12], although more recent work suggests the role of the posterior humeral circumflex artery is greater than previously thought [13]. The presence of certain fracture patterns has been demonstrated to be associated with a higher risk of humeral head necrosis: a medial metaphyseal head extension less than 8 mm, disruption of the posteromedial hinge and any fracture pattern that disrupts the anatomical humeral head [14]. The presence of any of these features should prompt the clinician to consider arthroplasty surgery as a more reliable treatment option.
NON-OPERATIVE TREATMENT
Between 80% and 90% of patients with proximal humeral fractures can be managed non-operatively [15]. The majority of these are minimally displaced fractures and studies have shown high union rates in these patients [16, 17]. The typical treatment would involve one or two weeks of immobilisation followed by progressive mobility under the guidance of a physiotherapist. Retrospective studies have reported 77-88% of patients have a good or excellent outcome [3, 15], achieving an average of 111° to 120° of forward flexion and 100° to 106° of abduction [16, 17]. Fig. (2) illustrated a case successfully managed non-operatively.
One part fracture treated conservatively with successful union.
The role of non-operative treatment is less clear in patients with displaced fractures. Surgical intervention for young patients or those with a high functional level with displaced two part fractures is not controversial. The treatment of elderly patients and those with displaced three and four part fractures remains uncertain. The decision of whether surgical intervention is indicated is based on four key factors: age, bone quality, fracture pattern and timing of surgery [18].
The combination of a clinical history, examination findings and radiographic investigations play a critical role in aiding decision-making. Key elements of the history involve: patient age, date of injury, hand dominance, pre-injury functional level, co-morbidities, cognition, social support and ability to participate in rehabilitation. The clinical examination should confirm the integrity of the axillary nerve, brachial plexus and axillary artery. Pre-operative plain radiographs should include an anteroposterior view of the glenohumeral joint, axillary lateral and lateral scapular views. The available imaging should demonstrate the congruity of the glenohumeral joint, the number of fracture fragments, the degree of fracture displacement and the presence of features associated with risk of devascularisation. If further information is required, computed tomography (CT) scanning with three-dimensional reconstructions might be obtained, as shown in Fig. (3). Although the use of CT has not been shown to improve the rate of inter and intra-observer reliability when classifying fractures [19], it may certainly be of value to the surgeon when planning internal fixation.

Reconstruction of a pre-operative CT demonstrating a four part fracture.
SURGICAL FIXATION
The aim of surgical fixation is to preserve articular surface congruency, alignment and vascularity to the humeral head. A key principle is to achieve an accurate reduction and restore the medial calcar support [20, 21], especially as malreduction in varus risks loss of reduction and limited motion [22]. Screws should engage into the subchondral bone where the bone quality is greatest [23] and should include inferomedial screws [20, 21]. The plate should be positioned at least 5 mm distal to the greater tuberosity to avoid impingement during abduction. Biomechanical studies have shown modern locking plates to have an increased torsional and pull out strength compared to non-locking plates [24, 25], which make them favourable for use in osteoporotic bone. Following fixation of the fracture, the tuberosities must be reduced and held, this can be done using screws but more commonly these are sutured onto the plate. The shoulder should then be taken through a passive range of movement to check stability and this informs the post-operative rehabilitation. Typically passive movement will be commenced after a few days before active mobilisation several weeks post-operatively.
The surgical approach is performed through either a deltopectoral or direct extended deltoid splitting approach depending upon surgeon preference. The required dissection, however, may increase the risk of devascularisation of the humeral head. One study reports that the risk of avascular necrosis doubled when open surgery was performed [26]. A number of authors have therefore advocated percutaneous fixation to reduce the morbidity of surgical exposure although there is limited ability to accurately restore the anatomy with current evidence of this technique being limited only to case series [27-29]. The use of open reduction and internal fixation for patients with high pre-injury function with displaced two part fractures is not controversial. However its use in three- and four- part fractures especially in the elderly patients is uncertain. Where three- or four-part fractures can be reduced and the bone quality is adequate plate fixation can be performed. However if the bone is of poor quality, the articular surface damaged or the blood supply compromised then arthroplasty should be favoured, especially if the patient is elderly or has a low functional demand. If the patient is young (< 60 years) then open reduction and internal fixation can be attempted as even if avascular necrosis occurs, the anatomic union of tuberosities will be advantageous for future arthroplasty surgery.
A recent systematic review of proximal humeral fixation showed a 98% union rate, an average Constant-Murley score of 74.3, flexion of 139° and external rotation of 48° [30]. However any benefit should be balanced against a high complication risk with 13.7% requiring repeat surgery [30]. These additional complications included avascular necrosis, loss of fixation, screw perforation and mechanical impingement [22, 31]. If plate fixation fails salvage arthroplasty is possible but reported outcomes are poorer than in cases of primary hemiarthroplasty [32, 33]. Figs. (4, 5) both demonstrate complications associated with surgical fixation.
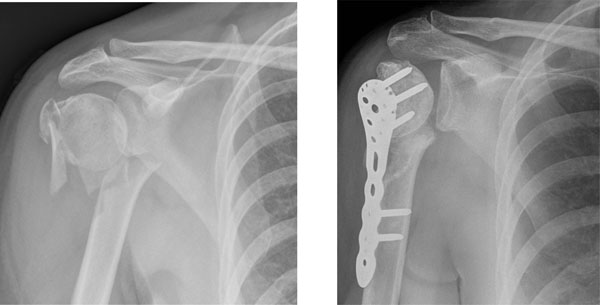
Inadequate fixation in a 51 year old lady with a four part proximal humeral fracture.

Inadequate fixation of two part fracture resulting in varus displacement and penetration of screws through humeral head necessitating removal.
INTRAMEDULLARY NAILING
Traditionally intramedullary nailing has been used to treat humeral shaft fractures. The development of nails with polyaxial screws has given the implant more stability making it a valid option for the management of proximal humeral fractures. Difficulties in accurately reducing the fracture and fixing the tuberosity fragments make two-part fractures more amenable to nail fixation than three- or four-part fractures and even then this may be inferior to fixation with locking plates. The advantage of the technique is that less soft tissue disruption is required at the fracture site lessening the risk of devascularisation of the humeral head and fracture fragments. However care should be taken when treating proximal and comminuted fractures to avoid propagation of fracture [34-36] and the entry point violates the rotator cuff and has been reported to lead to residual shoulder pain [37]. An example case managed with an intramedullary nail is shown in Fig. (6).

Two part fracture in 74 year old man treated successfully with an intramedullary nail.
The current literature on intramedullary nails is mainly based on small case series with mean Constant scores ranging from 62 to 74.5. The reported complication rate is high with 10% developing impingement, 31% requiring removal of metalwork, 12% developing AVN and 4% requiring early revision [37-39]. Giannoudis et al. performed a review of the literature on the Polarus nail and reported union rates of 95.8% and variable complication rates from 9.3% to 70% [39].
HEMIARTHROPLASTY
Neer first described the use of hemiarthroplasty for proximal humeral fractures reporting a 98% satisfactory or excellent rate [27, 40]. The procedure provides immediate stability and provides patients with reliable pain relief following surgery. However its ability to restore normal shoulder kinematics and function is debated [41].
Indications for hemiarthroplasty include fracture dislocations and humeral head splitting fractures [42, 43]. A head splitting fracture in a young patient can pose a real treatment dilemma as the surgeon wants to avoid arthroplasty but this may not be technically feasible. The use of hemiarthroplasty in the management of displaced three and four part fractures is controversial and dependent on both patient and fracture factors. Patients who are elderly, have low functional requirements, have high co-morbidities and have poor bone quality are more likely to benefit from hemiarthroplasty. Fractures that are comminuted, severely displaced, have features associated with avascular necrosis [14] and are delayed in presentation are also more likely to benefit from hemiarthroplasty.
Three key principles of surgical technique have been shown to improve outcome following hemiarthroplasty; humeral height, retroversion and tuberosity reduction/reconstruction [44]. An incorrect humeral height impairs shoulder function, lengthening may result in tuberosity detachment, rotator cuff failure and impingement, whereas shortening reduces the length and tension of the deltoid muscle impairing its function [45]. Excessive retroversion of the prosthesis is associated with joint dislocation [46] and failure of the tuberosities to unite [44]. Tuberosity malunion leads to impaired functional outcome [45] and reconstruction 10 to 16mm distal to superior margin of prosthetic head is optimal [47]. Optimal outcomes are reliant on a proper rehabilitation program [48, 49]. Typically this will involve 4 to 6 weeks of shoulder support with pendulum and passive movement guided by the stability during surgery. Active movement commences from 6 weeks if signs of radiographic healing are present.
A recent systematic review of hemiarthroplasty for fractures reported a mean post-operative forward flexion of 105°, abduction 92° and Constant score of 56 [41]. The reported complications included tuberosity non-union (11%), heterotopic ossification (9%), proximal migration of the prosthesis (6.8%), infection (2%) and nerve injury [41]. In addition the implant can wear the glenoid leading to pain and need for further surgery [50]. Fig. (7) demonstrates a three part fracture dislocation treated with hemiarthroplasty.

3 part fracture dislocation in a 61 year old lady treated with primary hemiarthroplasty.
REVERSE ARTHROPLASTY
Traditionally the reverse shoulder arthroplasty was designed and used for degenerative rotator cuff arthropathy [46]. The reverse arthroplasty functions by medialising and lowering the centre of rotation of the glenohumeral joint. This improves the torque of the deltoid, by increasing tension and recruiting more muscle fibres, and allows greater shoulder elevation independent of the rotator cuff [51, 52]. Its indications were extended to fracture surgery as function may be restored without reliance on tuberosity healing which is especially unreliable in elderly patients with poor quality tuberosities with comminution. An example case is demonstrated in Fig. (8). An important pre-requisite, however, to performing reverse arthroplasty for fractures is to ensure that the axillary nerve is functioning prior to surgery as denervation of the deltoid would result in limited function.
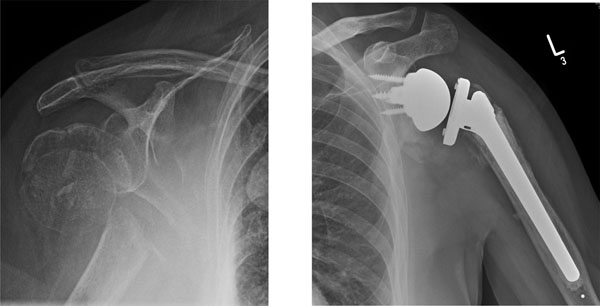
3 part fracture in an 82 year old lady treated with primary reverse arthroplasty.
The procedure has been recommended for patients over 75 years with three and four part fractures as it provides similar pain relief to hemiarthroplasty without reliance on tuberosity union for function in this elderly group [52]. Although studies to date are retrospective, they report comparable function to other surgical techniques with an average forward flexion of 123°, abduction of 112° and Constant score 68 [53]. In addition, the procedure has been advocated as a salvage operation following failure of hemiarthroplasty with 80% satisfaction rate reported [54]. The complication rate is high including neuropraxia (11.6%), reflex sympathetic dystrophy (7%), anterior dislocation (2.3%), displacement of tuberosities (44.2%) and scapular notching (23.2%) [55]. Additional concern over the longer term results of the prosthesis have been raised following reports that 63% have radiographic evidence of glenoid loosening at a mean of 6 years follow up [53]. Firm conclusions cannot be drawn until both longer follow up is available and randomised controlled trials (RCT) compare this modality against other primary treatments.
DISCUSSION
The majority of proximal humeral fractures are minimally displaced and can be successfully managed non-operatively. However the treatment of displaced fractures remains controversial [4-6] and it remains unclear when surgical intervention is beneficial and if so which surgical technique should be utilised. Comparative studies of the different techniques employed are infrequent and those that are available are typically comparative case series and provide low levels of evidence. The lack of adequately powered randomised controlled trials (RCT) precludes definitive conclusions being drawn over the optimal treatments.
One RCT comparing hemiarthroplasty and non-operative management in displaced four part fractures reported an improvement in quality of life in those treated with hemiarthroplasty compared to conservative treatment [56]. The study also showed a trend to improved function and pain relief following hemiarthroplasty but failed to demonstrate any statistical significance in these outcomes. Although this paper shows improved quality of life after hemiarthroplasty, it does not definitively prove if function also improves and does not address those patients with three part fractures. Therefore it remains unclear whether hemiarthroplasty or non-operative treatment results in improved functional outcomes. Of two RCTs comparing plate fixation with non-operative management, neither reported any statistically significant difference between the two groups in terms of functional outcomes [16, 57]. Three further retrospective comparative case series also showed no difference between the groups [58-60]. The studies did show that surgical fixation was associated with a higher rate of complications against which any potential benefit of surgical fixation should be balanced.
One RCT comparing hemiarthroplasty and locking plate fixation for four part fractures has reported no significant difference in functional outcomes between the groups [61]. However only 32 patients were recruited into the study and this low number is a significant limitation. In addition, the study only addressed four-part fractures. A number of retrospective reviews have compared the two modalities with two reporting no difference [62, 63] and two showing plate fixation to have superior functional outcomes [5, 64] however significant limitations in methodology weaken any definitive conclusions that can be drawn from these. Further adequately powered RCTs comparing plate fixation and hemiarthroplasty are required.
Prospective comparative studies of intramedullary nailing and locking plate fixation showed no difference between the two groups in terms of function at twelve months or complications [37, 65] but these studies provide only low-level evidence. Case series and a recent systematic review have reported comparable functional results with both reverse arthroplasty and hemiarthroplasty [52, 66, 67]. The reverse arthroplasty is receiving increasing support due to its ability to restore function independent of tuberosity union but adequately powered comparative RCTs are required to provide a definitive answer.
CONCLUSION
The treatment of three- and four- part proximal humeral fractures remains controversial. Current evidence does not provide a definitive answer and decision-making should be made on an individual basis dependent on patient and fracture factors. Reverse arthroplasty provides a reliable option for complex fractures in elderly patients but high quality comparative studies are required.
CONFLICT OF INTEREST
The authors received no financial contributions to the work reported and no other potential conflict of interest exists.
ACKNOWLEDGEMENTS
Declared none.


