All published articles of this journal are available on ScienceDirect.
Invasive Electromagnetic Field Treatment in Osteonecrosis of the Femoral Head: A Prospective Cohort Study
Abstract
Introduction :
The purpose of this prospective cohort study was to compare the surgical treatment of non-ONFH in adulthood by curettage and bone grafting with treatment by curettage and bone grafting in combination with invasive electromagnetic field treatment using Magnetodyn®. This was assessed by examining whether electromagnetic field treatment has a positive additive effect on the clinical parameters modified Harris Hip Score according to Haddad, Cook and Brinker, Merle d'Aubigné hip score and visual analogue scale, and on the subsequent need for treatment by total hip arthroplasty.
Materials and Methodology :
The prospective, non-randomised study included 35 patients with unilateral or bilateral osteonecrosis of the femoral head. These were divided into two groups according to the surgical treatment regime and assessed over a 12-month follow-up period. The study group (Group 1) comprised 19 patients (14 men and 5 women) with a total of 22 non-ONFH, who underwent minimally invasive curettage, bone grafting and electromagnetic field treatment (Magnetodyn®) by implantation of a bipolar induction screw. The control group (Group 2) comprised 16 patients (12 men and 4 women) with a total of 18 non-ONFH, who underwent minimally invasive curettage and bone grafting without Magnetodyn® therapy. At the initial pre-operative examination and the 6 and 12-month follow-up, all patients were assessed by clinical examination and radiological monitoring, and by bilateral hip MRI. The clinical evaluation was based on the modified Harris Hip Score according to Haddad, Cook and Brinker, the Merle d`Aubigné hip score and the visual analogue scale (VAS).
Results :
At the time of follow-up, total hip arthroplasty (THA) had been performed in four patients in Group 1 (18%). In Group 2, four patients (22%) had received a THA (n.s.). Both procedures led to an improvement in the clinical scores (Harris Hip Score, Merle d`Aubigné score and VAS), although no significant difference was observed.
Conclusion :
The authors conclude that electromagnetic field treatment with Magnetodyn®, using the special signal protocol applied here, as an adjunct to curettage and autologous bone grafting to treat non-ONFH, does not produce better clinical results and does not offer better prophylaxis for the avoidance of total hip arthroplasty over all ARCO stages.
INTRODUCTION
Non-traumatic osteonecrosis of the femoral head (non-ONFH) can lead to a collapse of the osseous femoral head and hence require an artificial replacement of the hip joint. Various surgical treatment regimes preserving the femoral head have been developed for non-ONFH to avoid artificial replacement of the hip joint [1-3]. Alternatively, biophysical stimulation with pulsed electromagnetic fields (PEMFs) can be used to treat non-ONFH. This technique was first described in the literature by Eftekhar in 1983 [4]. Weak electromagnetic fields can have a positive influence on angiogenesis and osteogenesis [5]. Studies by Massari and Santori concluded that capacitive electromagneticstimulation with pulsed electromagnetic fields (PEMFs) in combination with core decompression and autologous bone grafting had a positive short-term effect on catabolic inflammatory response in the joint cartilage and subchondral bone oedema in non-ONFH. In addition, the above-mentioned studies concluded that there was a positive long-term effect in relation to bone remodelling and chrondrocyte protection in the treatment of non-ONFH [6, 7]. As yet, there are still no irrefutable evidence-based studies concerning electromagnetic field treatment in osteonecrosis of the femoral head. The purpose of this prospective cohort study was to compare the surgical treatment of non-ONFH in adulthood by curettage and bone grafting with treatment by curettage and bone grafting in combination with invasive electromagnetic field treatment using Magnetodyn® [8]. This was assessed by examining whether electromagnetic field treatment has a positive additive effect on the clinical parameters modified Harris Hip Score according to Haddad, Cook and Brinker, Merle d'Aubigné hip score and visual analogue scale, and on the subsequent need for treatment by total hip arthroplasty.
MATERIALS AND METHODOLOGY
From June 2003 to October 2005, 35 patients with unilateral or bilateral non-ONFH were divided prospectively into two groups according to the surgical treatment regime, at the surgeon's discretion and without applying selection criteria, and were assessed over a 12-month follow-up period. The Magnetodyn® treatment consisted of an external magnetic field coil and an invasive bipolar induction screw system (Fig. 1). The stimulation parameters used were a sinus-shaped external magnetic field of ~20 Hz with magnetic flux density of ~5 mT and induced voltage of up to ~700 mV at the implant, with the aim of generating an electric field strength of 50-700 mV/cm in the bone tissue. The study group (Group 1) comprised 19 patients (14 men and 5 women) with a total of 22 osteonecroses of the femoral head, who underwent curettage, autologous bone grafting (autograft) from the greater trochanter and proximal femur using a 8 mm hollow – core drill and plug in the core the reverse direction in combination with electromagnetic field treatment (Magnetodyn®). Three of these 19 patients had a bilateral non-ONFH. The control group (Group 2) included 16 patients (12 men and 4 women) from the total patient collective (18 non-ONFH), who were treated with curettage and autologous bone grafting without Magnetodyn® therapy. Two of these 16 patients had a bilateral non-ONFH. The mean age of Group 1 at the time of surgery was 41.2 years (range: 33-54 years). The mean age of Group 2 at the time of surgery was 42.5 years (range: 33-54 years). None of the patients in either group had received bone-building medication. At the initial pre-operative examination and the 6 and 12-month post-operative follow-up, all patients were assessed by clinical examination and radiological monitoring with pelvic view and axial projection of the hip joint, and by bilateral hip MRI. After three months, clinical and radiological monitoring were performed in Group 1, and implant removal in the fourth month post-surgery was planned. The stage of non-ONFH was determined in both groups using the ARCO (Association Research Circulation Osseous) classification [9]; where this paper refers to 'stages', without further addition, it is this classification that is meant. The clinical evaluation was based on the modified Harris Hip Score according to Haddad, Cook and Brinker [10], the Merle d`Aubigné hip score [11], the visual analogue scale (VAS) [12] and the subsequent need for treatment by total hip arthroplasty. The data were evaluated using MS Excel IBM SPSS Statistics at a 95% level of significance. The study was planned in accordance with the Consolidated Standards of Reporting Trials (CONSORT) policy and conducted according to the ethical and legal jurisdication.

Magnetodyn® screw in situ in two planes.
RESULTS
Pre-operatively, Group 1 had 22 non-ONFH with three (14%) at stage 2A, eight (36%) at stage 2B, seven (32%) at stage 2C and four (18%) at stage 3C. Group 2 had a total of 18 non-ONFH, with four (22%) at stage 2A, nine (50 %) at stage 2B, two (11%) at stage 3B and three (17%) at stage 3C.
A Mann-Whitney test performed to assess age homogeneity revealed no significant difference between Group 1 and Group 2 with regard to age structure.
In Group 1, total hip arthroplasty (THA) was performed in two patients (29%) at stage 2C and in two patients (50%) at stage 3C. In Group 2, one patient (11%) at stage 2B, one patient (50%) at stage 3B and two patients (67%) at stage 3C received a THA.
Evaluation of the Merle d`Aubigné Score
The Mann-Whitney test to compare the groups over all ARCO stages was used (Fig. 2). No significant difference between the two groups could be found at any point of time regardless of ARCO stage.
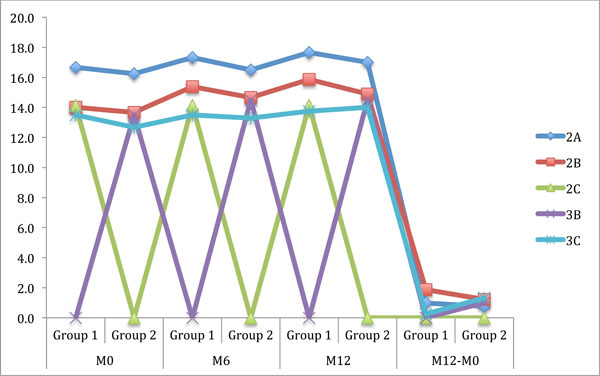
Merle d`Aubigné score of the ARCO stages for the examination times pre-op (M0), 6 months (M6) and 12 months (M12), post-op and the examination period 12 months to pre-operative examination (M12-M0).
The Wilcoxon test to compare examination times M0 and M12 over all ARCO stages showed (p=0.002 for M0/M12) that both procedures were promising up to stage 2A.
The Mann-Whitney test to compare the groups at ARCO stage 2B showed no significant differences in Merle d`Aubigné scores between Group 1 and Group 2 at any time. An improvement in the Merle d`Aubigné score in Group 1 (1.9) compared with Group 2 (1.2) at stage 2B was a descriptive observation, but it was not statistically significant.
The Mann-Whitney test to compare the groups at ARCO stages above 2B showed no significant differences in Merle d`Aubigné scores between Group 1 and Group 2 at any time. There was no significant improvement or deterioration in scores between Group 1 and Group 2 at higher stages.
Evaluation of the Harris Hip Score
Both, overall and for each ARCO stage individually, the Harris score showed no significant differences between Group 1 and Group 2.
The Wilcoxon test to compare the groups over all ARCO stages showed that both procedures were promising up to stage 2A.
Evaluation of the Visual Analogue Score (VAS)
There were no significant differences in VAS between Group 1 and Group 2. Over all stages, no significant improvement or deterioration was observed as a result of the procedure used in Group 1.
The Wilcoxon test to compare between M0 and M12 over all ARCO stages showed (p=0.000 for M0/M12) that both procedures were promising up to stage 2A.
DISCUSSION
Curettage and bone grafting is an established, safe and effective surgical treatment for non-ONFH. There are indications in the literature that biophysical stimulation of non-ONFH with PEMFs has an additional positive effect as an adjunctive treatment [6, 7]. The central question addressed by our study was whether invasive electromagnetic field treatment with Magnetodyn® [5] as an adjunct to curettage and bone grafting in non-ONFH produces better clinical results than a procedure without invasive electromagnetic field treatment. Treatment of non-ONFH by the two procedures compared in this study was equally promising in Group 1 and Group 2 with regard to the measurement parameters Harris Hip Score, Merle d`Aubigné score and VAS, up to stage 2A. At higher stages, there were no significant differences in final treatment outcomes between the two groups.
Operative complications implanting an invasive bipolar induction screw system such as subtrochanteric and femoral neck fracture, hematoma, infection and heterotopic ossification were not be seen.
In 2012 Kang et al. published a pilot study of multiple drilling and alendronate for osteonecrosis of the femoral head compared to multiple drilling alone with a reduction of pain and a delay of progression for early-stage non-ONFH [13]. None of the patients in either group had received bone-building medication.
In a 1990 study, Steinberg et al. also concluded that electrical stimulation therapy, here in the form of non-invasive capacitive coupling, as an adjunct to decompression and autologous bone grafting in non-ONFH, did not produce better results than decompression and autologous bone grafting alone [14]. The data in our study support this finding, even though the coupling in the above-mentioned study was not magnetic and was non-invasive.
An earlier (1989) study by Steinberg et al., which compared the results of core decompression and bone grafting with and without direct electrical stimulation in the form of a coil inserted invasively into the femoral head, concluded that the adjunctive invasive electrical treatment improved the clinical results [15]. This finding contradicts the results of our study. A possible reason for this might be the different types of coupling: magnetic coupling by external coil in our study contrasted with direct coupling with an invasive coil in the femoral head in the above-mentioned study. A review by Aaron and Steinberg of invasive and non-invasive electrical stimulation of osteonecrosis of the femoral head concluded that PEMF is a highly promising technique but that the optimal signal protocols and user designs are still unknown [16]. An altered signal protocol of the electromagnetic field treatment with Magnetodyn® used in our study might lead to an improvement in the clinical results.
In a further study (in 1995) of 300 stage I to IVA osteonecroses of the femur treated with core decompression, Steinberg had to treat 35% of the patients with a THA. The hip joints with small areas of osteonecrosis at stages I and II showed much better clinical results than the hip joints with larger areas of osteonecrosis. The joints with small areas of osteonecrosis required endoprosthetic treatment following decompression and bone grafting in only 7% of cases [3]. A literature review by Marker et al. regarding core decompression outcomes between 1992 and 2007 summarised the data from 1268 cases of osteonecrosis of the femoral head. The average follow-up was 63 months (1-176 months), with a failure rate of 30% of the patients who had to be treated with THA [17]. One cohort study of 52 patients (79 hips) with an average follow-up of 24 months which was evaluated by Marker in this literature review showed a 34% THA failure rate. At 18% in Group 1 and 22% in Group 2, the THA failure rate in our study is therefore approximately within the range reported in the literature.
CONCLUSION
To summarise, it can be stated with justification that minimally invasive curettage/decompression in combination with autologous bone grafting is a decisive treatment factor in both procedures. This is sufficiently supported by the literature [6, 17-19].
The invasive electromagnetic field treatment used additionally in Group 1 in this study did not produce better clinical results than were achieved in Group 2. The authors conclude that electromagnetic field treatment with Magnetodyn®, using the special signal protocol applied here, as an adjunct to curettage and autologous bone grafting to treat non-ONFH, does not produce better clinical results and does not offer better prophylaxis for the avoidance of total hip arthroplasty over all ARCO stages.
AUTHORS` CONTRIBUTIONS
Christoph Windisch: Design of the study, and preparation of the manuscript.
Werner Kolb: Design of the study.
Eric Röhner: Analysis and interpretation of data, preparation of manuscript.
Markus Wagner: Analysis and interpretation of data, preparation of manuscript.
Andreas Roth: Revision of manuscript.
Georg Matziolis: Analysis and interpretation of data, preparation of manuscript.
Andreas Wagner: Analysis and interpretation of data, preparation of manuscript.
CONFLICT OF INTEREST
Authors confirm that this article content has no conflict of interest.
LIST OF ABBREVIATIONS
ACKNOWLEDGEMENTS
Declared none.


