All published articles of this journal are available on ScienceDirect.
Staged Subtalar Fusion for Severe Calcaneus Fractures with Bone Loss
Abstract
Background:
With high energy fractures to the calcaneus there is the potential for significant bone loss. The loss of bone can make it difficult to fully regain calcaneal alignment. In addition these fractures are often associated with significant soft tissue injury. These two factors make it difficult to address this injury in a single stage, and can have significant complications. To address these issues our initial goal in treatment has been restoration of calcaneal alignment and stabilization of the surrounding soft tissue, followed by delayed/staged subtalar arthrodesis.
Methods:
Patients with calcaneus fractures treated by a single surgeon from 2002 to 2012 were reviewed. Injuries which were found to have medial extrusion of the posterior facet and bone loss, and subsequently underwent a staged protocol involving early provisional fixation and late subtalar fusion were included.
Results:
We treated 6 calcaneus fractures with bone loss. All patients were treated with staged subtalar fusion after initial irrigation and debridement and provisional fixation. No soft-tissue complications were noted after the fusion procedure in any of the six cases. Fusion occurred in all six patients at an average of 20.6 weeks (range, 13-23 weeks). All patients were able to ambulate and wear a regular shoe by one year following the initial injury.
Conclusion:
It is important in the high energy calcaneus fracture to assess for both soft tissue integrity and bone loss. A thorough debridement of both the soft tissues and any devitalized bone should be performed as well as provisional fixation which attempts to restore near normal calcaneal anatomy. Definitive fusion should not be performed until the soft tissues have fully recovered.
INTRODUCTION
The calcaneus is the most commonly fractured tarsal bone, representing 60% of tarsal fractures [1-3]. As of yet there is not a standardized treatment algorithm for approaching severe calcaneus fractures [3, 4]. For these fractures which typically have high energy mechanisms and severe presentations several different methods of treatment, including staged procedures, have been suggested [3, 5]. These include the use of external fixation and percutaneous pinning with subsequent definitive ORIF or subtalarfusion [4, 5]. Other treatment modalities such as non-operative treatment, primary subtalarfusion, percutaneous pinning, or ORIF have been advocated [4, 6, 7]. Complication rates for each of these methods vary. Overall the incidence of complications with closed calcaneal fractures ranges from 0-20%. The incidence increases with an open fracture to 0-31 % [5, 6]. Complication rates are variable with the small series numbers. However, all would agree that open calcaneus fractures have a higher complication rate.
Due to improvement in acute trauma care, patients with higher energy mechanisms of fracture are surviving to have their fractures treated [1]. Mechanism of injury ranges from falls and motor vehicle collisions in the general public to blast injuries suffered in military personnel. It is expected that with these higher energy fractures that there would be a higher incidence of complications. In a military study conducted on 102 patients with open calcaneal fractures 42 % of patient underwent amputation. Not surprisingly, predictors of eventual amputation included mechanism of injury, wound location, size of wound, and increasing Gustilo and Anderson classification types [8-10]. A retrospective review of 2 level 1 prospective databases found a much lower incidence of amputation. Only those suffering severe crush injures received early amputation and no late amputations were reported. However, they did note that patients with severe comminution did have poorer outcomes [11].
One characteristic of these high energy calcaneus fractures that has received little attention in the literature is that of bone loss. It has been our experience that either upon initial exploration of the fracture and even in subsequent procedures that there will be portions of bone lost or extruded from an open wound. The loss of bone can make it difficult to maintain the normal height, length, width, and anatomic alignment of the calcaneus. In addition non-viable bone can lead to osteomyelitis. The dead space created by lost bone can also be an environment that promotes infection. Depending on the extent of bone loss these fractures may not be amenable to certain treatment modalities. We present a series of six patients with high energy mechanism and loss of bone which were treated in a staged approach. Our goals at the primary surgery included creating a clean wound and establishing near normal calcaneal alignment. This often times required removal of non-viable portions of bone. Since outcomes can often rely heavily on soft tissue management [1, 3, 5, 12], one of our initial treatment goals has been stabilization of the surrounding soft tissue envelope. After the soft tissues were healed this was then followed by subtalar arthrodesis. In our series we demonstrated good outcomes consisting of fusion and ambulatory status in all of our subjects. We present this staged approach as an acceptable option in the setting of calcaneal fracture with bone loss.
MATERIALS AND METHODS
A review of the medical records from 2002 to 2012 was made. Patients with calcaneus fractures which were found to have medial extrusion of the posterior facet and bone loss, and subsequently underwent a staged protocol involving early provisional fixation and late subtalar fusion were included. The method of primary fixation varied among patients depending on fracture characteristics and the amount of bone loss. All of the patients in the study had suffered their injuries as a result of MVC. All of the patients were female. Ages ranged from 18 to 58 years old with an average age of 36 years old. Information regarding associated injuries was collected. Time of initial and subsequent procedures to address the calcaneus fractures was collected. Time to fusion and weight bearing was also reported. Primary outcome measures were time to fusion and ability to ambulate after fusion.
Operative Approach
Reduction of the tuberosity and body of the calcaneus is done through the open medial wound. Debridement of all non-viable soft tissue and bone is performed. 4.5 or 5.5 screws or 3mm smooth Steinman pin placement is done through percutaneous stab wounds over either the posterior tuberosity or through the talar neck. Using smaller fixation preserves bone stock and makes it easier to use 6.5 screws for definitive subtalar fusion fixation. Poly (methyl methacrylate) (PMMA) antibiotic beads are utilized to fill in the bony defect if it is large. The open wound in all cases was medial, so the lateral skin and soft tissues was not disturbed with initial, provisional fixation. When initial provisional fixation is done early, the soft tissues have not contracted and the tuberosity can easily be pulled out to length and proper height and width re-established. The open wound is loosely closed in one layer with nylon suture.
The skin is allowed sufficient time to recover which may take several months. By that time, a portion of the calcaneal body has often healed and alignment is maintained. At this time, a planned subtalar fusion is done with tri-cortical posterior iliac crest bone graft to fill the defect. Any remaining defect can be filled with cancellous bone graft or bio-absorbable antibiotic impregnated beads. The subtalar fusion is done through a posterlateral approach to the subtalar joint as described by Gallie [13], utilizing the subtalar bone block distraction arthrodesis technique as described by Carr [14].

Lateral radiograph demonstrating void from medially extruded posterior calcaneal facet.
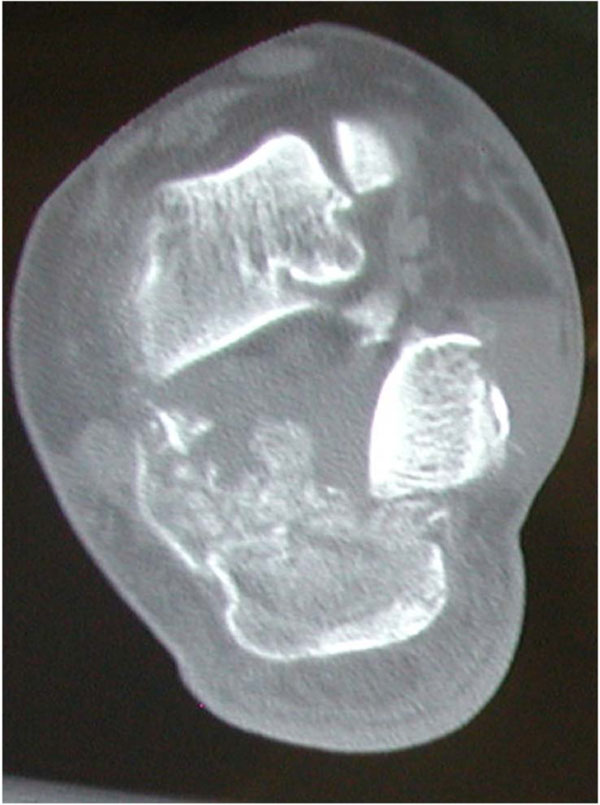
Coronal CT demonstrating medial extrusion of posterior calcaneal facet. Pressure on the soft tissues from the extruded piece led to full thickness skin necrosis.

Lateral radiograph demonstrating provisional fixation with antibiotic spacer bead strung on a wire.

Lateral radiograph demonstrating subtalar fusion.
REPRESENTATIVE CASE
Case 2
A 19-year-old woman was transferred to our trauma center from another facility for treatment of injuries she sustained as the unrestrained driver in a motor vehicle accident. She was found to have an open right calcaneus fracture, in which a 2 cm x 3 cm bone fragment from the posterior calcaneal facet had been extruded out the medial-sided 6 cm skin laceration. A CT scan was obtained, which demonstrated a comminuted intra-articular calcaneus fracture.
The patient was taken to the operating room that night for irrigation and debridement, where it was determined that the extruded bony fragment contained approximately two-thirds of the posterior facet of the calcaneus. It reportedly had a thread of attached viable soft tissue, and thus it was reduced back to its anatomic position. The patient was taken back to the operating room for repeat irrigation and debridement. At this time, it was felt that the bony fragment was no longer viable, and it was therefore excised. Three Steinmann pins were used for fixation of the remaining fragments, and the void left behind from excision of the posterior facet fragment was filled with a strand of antibiotic beads consisting of polymethyl methacrylate (PMMA) mixed with tobramycin and strung on a wire. The skin was closed without tension.
The medial wound healed over the course of two months and the skin recovered. The patient was taken to the operating room at 12 weeks after her initial injury for hardware removal, removal of the beads, and subtalar bone block fusion using iliac crest bone graft and resorbable beads mixed with tobramycin. She was allowed to bear full weight on her right lower extremity seven weeks postoperatively. Radiographic evidence of solid fusion was noted 15 weeks postoperatively.
The patient was able to wear a regular shoe and return to full time employment as a factory worker.
Selected Images From Cases 2 and 4 (Figs. 1-4)
RESULTS
We treated 6 calcaneus fractures with bone loss. Four fractures were open and two were closed. The two closed fractures had coupled medial dislocation of the posterior calcaneal facet which came to rest subcutaneously and resulted in a full thickness pressure wound which required excision. Of the 6 patients, 4 sustained additional injuries.
All patients were treated with staged subtalar fusion. Patients on average received 3 surgeries for definitive treatment (Range 2-4). Time to primary surgery was on average 5 days (Range 1-21 days) Of those receiving more than 2 surgeries all required 1 or more I&D procedures. One of these was as a result of suspected osteomyelitis which was adequately addressed with removal of devitalized bone and placement of antibiotic impregnated beads. 2 additional patients received antibiotic impregnated beads for prophylaxis and to fill space left by bone loss. 5 of the six patients required some form of structural graft. 4 of the six patients received iliac crest bone grafting, 1 of which, having had osteomyelitis, additionally received antibiotic impregnated bio absorbable beads. Antibiotic impregnated calcium sulfate beads alone were used to fill the bony void in 1 case. One patient was felt to have enough stability without structural grafting. The patient with osteomyelitis underwent long term antibiotic treatment post fusion. No soft-tissue complications were noted after the fusion procedure in any of the six cases. Follow up and repeat x-rays were possible for all six patients. Fusion occurred in all six patients at an average of 20.6 weeks(range, 13-23 weeks). All patients were able to ambulate and wear a regular shoe by one year following the initial injury. Complications at the time of fusion or at post fusion follow-up included: equinus deformity, clawing of the toes, hallux valgus deformity, and avascular necrosis of the talus. No amputations were required (Table 1).
Summary of Cases
| Case | Age | Sex | Mechanism | Associated Injuries | Day of Provisional Fixation | Time to Subtalar Fusion | Total # Surgeries | Outcome/Time to Follow Up |
|---|---|---|---|---|---|---|---|---|
| 1 | 18 | F | MVC | R Medial Malleolus Fx L Midfoot Fxs. Facial Fxs |
HD#4 | 4 months p/o | 2 | Fusion 21 weeks po Ambulation/RTW at 10 months p/o |
| 2 | 19 | F | MVC | HD #1 | 12 wks. | 3 | Fusion at 15 wks. w/RTW | |
| 3 | 46 | F | MVC | R Pilon Fx L Talus Fx Subtalar Dislocation Left Distal Fibula Fx Left cuboid fx |
HD #1 | 10 wks. | 3 | Fusion at 16 wks. Avascular necrosis of talus(Non-op) Clawing of L 1-4 toes leading to tenotomy and fusion. RTW at 2 years |
| 4 | 58 | F | MVC | Facial Fxs Transection Thoracic Aorta Subtalar Dislocation |
3 wks. | 6.5 mths | 4 | Fusion at 13 wks. Weight bearing at 5.5 months. Hallux Valgus Clawing of Second Toe. Stiff Midfoot |
| 5 | 25 | F | MVC | HD #1 | 14 wks. | 3 | Fusion at 27 wks. Full weight bearing |
|
| 6 | 54 | F | MVC | R patella Fx R medial Mal Fx R D Fibula Fx |
HD #4 | 12 | 3 | Fusion at 32 wks. Full weight bearing |
Legend: MVC: Motor Vehicle Collision Fx: Fracture HD: Hospital Day RTW: Return to Work.
DISCUSSION
There is no consensus in the current literature regarding the optimal treatment of intra-articular fractures of the calcaneus [4]. In addition, the decision to choose one approach over another is surgeon specific and does not follow a standardized approach. In a series of 25 patients with intra-articular calcaneus fractures, Lamichhane A et al. advocate a single stage combined percutaneous and minimal internal fixation method after resolution of soft tissue swelling. They reported no deep surgical infections, and superficial infections in 3 patients. All fractures showed union by 8 weeks [4]. The authors did not comment on the initial state of the soft tissues or bone loss. In a study published in 2001 Benirschke et al. reported on a retrospective review of 218 displaced intra-articular fractures. 5.5% of these fractures were open. These were treated with ORIF via a lateral approach at an average of 9.5 days. 3.2 % of patient developed infections. All of these had closed fractures. 43.5% required some subsequent procedure. Hardware removal in 93% and Subtalar fusion in 5.2% were the most common. One below-knee amputation was performed secondary to infection. The authors do not comment on bone loss. The authors concluded that primary open reduction internal fixation of displaced intra-articular fractures was an acceptable method of treatment [15]. In a separate series in 2010 Benirschke et al. reported on 14 open Type 2 or 3a fractures with medial sided wounds. The patients were treated with initial irrigation and debridement coupled with temporary percutaneous pinning within 8 hours of presentation. The goal of the initial procedure was to attempt to restore calcaneal anatomy and stabilize soft tissues. Definitive treatment was open reduction and internal fixation through a lateral approach. This was carried out when soft tissues were closed, which occurred at an average of 18 days after presentation. Both superficial and deep infections occurred at a rate of 7.14%. The deep infection required hardware removal and antibiotics for resolution. Union occurred at an average of 19 months. No amputations were reported. The authors do not mention bone loss or comminution [5]. In a study published in march of 2013 Cohen et al. advocate the use of a minimally invasive technique over the extensile lateral approach in treating intra-articular calcaneal fractures. Although all patients in the study went on to union, they reported improved wound complications (6% vs 29%), and secondary surgeries (0.89% vs 9%) in the minimally invasive and extensile approach respectively. Additionally patients in the minimally invasive groups had improved FFI scores, VAS pain scores, and overall patient satisfaction scores. Patients with open fractures were not included in the study [16]. The authors did not comment on the incidence of superficial or deep infection. No comment was made on bone loss. A separate study by Abdelgaid also advocated the use of a percutaneous approach for the treatment of intra-articular fractures, especially in settings where ORIF might be contraindicated due to soft tissue compromise [17]. Other methods including primary arthrodesis, and combined external and internal fixation have been suggested for addressing this problem [18, 19].
As it has been demonstrated there are many different approaches that can be taken when addressing calcaneus fractures. In addition to the fracture characteristics themselves, other factors such as the state of the soft tissue, as well as any bone loss should be considered. In a study published in 2003 Sanders et al. presents the importance of soft tissue injury in determining outcome of calcaneal fractures. This study compares the outcome of 42 open calcaneal fractures. These fractures were graded according to the Gustilo Anderson classification system [8, 9]. An increased complication rate was found with more severe soft tissue injury. The fractures were treated with a staged protocol consisting of antibiotics, I&D, temporary coverage and initial stabilization followed by definitive fixation after the wound was clean and soft tissue swelling had decreased. 37.5% of type 2, 25% of type 3a, and 76.9 % of type 3B fractures had infection as a complication. 60% of the infections from the type 3 B group developed osteomyelitis with 50% of those requiring eventual amputation. It was concluded that despite an aggressive staged approach that open calcaneus fractures have a high likelihood of infection. The importance of early soft tissue coverage was highlighted [12]. Benirschke et al. also points out the increased rate of soft tissue complications with soft tissue compromise [1].
In addition to the state of the soft tissues it is important to know the state of the underlying bone. It has been emphasized in several studies the importance of regaining, as near as possible, the normal anatomic alignment of the calcaneus [2, 3, 5, 6]. However, little is mentioned in regards to the loss of bone and its effects on the ability to meet this goal initially or in a staged approach. In addition to the difficulty in realigning the bone, devitalized or frankly absent bone can become a risk factor for infection. In the representative case it is evident that by allowing devitalized bone to remain in the wound that there is a potential for osteomyelitis. This puts the integrity of any initial fixation at risk as well as requiring further procedures or intervention to address the infection. For bone that is removed during initial debridement a dead space is created which allows for an environment where fluid can collect and infection can arise. Dead spaces also can be filled with fibrous in-growth which can complicate definitive fusion. The staged approach addresses this problem. During our initial irrigation and debridement procedure we were able to assess the soft tissue as well as the integrity of the underlying bone. In cases where sufficient bone loss was found that would otherwise prevent reduction and internal fixation definitively, we elected to follow a staged approach leading to fusion. Devitalized bone was removed, and where necessary, the void was filled with antibiotic eluting spacer beads. These spacer beads fill the dead space preventing fibrous in growth and fluid collection as well as preventing infection through high levels of local antibiotic delivery [20]. We were able to, as much as possible, restore the anatomic alignment of the calcaneus at the index surgery. We then allowed the soft tissues to heal. Once the soft tissues were healed we then had an excellent environment for performing our definitive fusion. Often times at the definitive subtalar fusion surgery it was still required that we address some form of void caused by initial bone loss. This was accomplished with either iliac crest bone graft or antibiotic impregnated bio absorbable material.
All 6 of our patients treated in this manner went on to fusion and were able to ambulate in a normal shoe one year after their injury. Further studies will be necessary to compare this treatment strategy to other previously defined protocols.
CONCLUSION
It is important in the high energy calcaneus fracture to assess for both soft tissue integrity and bone loss. A thorough debridement of both the soft tissues and any devitalized bone should be performed. In cases with significant bone loss, provisional fixation which attempts to restore near normal calcaneal anatomy should be performed. Any residual deformity will be difficult if not impossible to restore at the time of fusion [3]. Any large defects can be addressed with some form of bio absorbable material, with or without the addition of antibiotics. Definitive fusion should not be performed until the soft tissues have fully recovered.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


