All published articles of this journal are available on ScienceDirect.
Acetabular Component Anteversion in Primary and Revision Total Hip Arthroplasty: An Observational Study
Abstract
Purpose:
In a prospective manner to evaluate the range of acetabular component anteversion actually achieved by the use of a cup positioner in cementless revision and primary THA.
Methods:
We operated 71 patients with cementless primary THA, and 26 patients with cementless acetabular revision surgery. We aimed to obtain cup anteversion of 10 to 30° with an impactor-positioner. In all cases we used elevated liners and a ceramic head with diameter 28. At 3 months postoperatively the component versions were measured using CT with the patient in supine position.
Results:
The acetabular component version in the primary hips ranged from 28° of retroversion to 42° of anteversion with a mean of 17.4 ± 14.0°, while the cup version in the revision hips ranged from 4° of retroversion to 32° of anteversion with a mean of 15.0 ± 9.6°(p=0.427). The anteversion of 40 (56%) of the primary acetabular components were within the target zone of 10 to 30°, while 19 (27%) were below the target zone and and 12 (17%) were above the target range. The anteversion of 19 (73%) of the revision acetabular components were within the target zone, while 6 (23%) were below the target zone and 1 (4%) were above the target range. The differences in distribution between the primary and revision operations were not significant (p=0.183).
Conclusions:
The intraoperative estimation of acetabular anteversion by free hand technique in many cases was not within the intended range of 10 to 30° in either primary or revision THA and with no differences between the two series
INTRODUCTION
Appropriate orientation of the acetabular cup is an important determinant to achieve adequate range of motion and stability in total hip arthroplasty (THA). Malpositioning has been associated with impingement, dislocation, accelerated polyethylene wear, pelvic osteolysis, component loosening and migration [1-4]. Generally, cup positioning is performed with the use of mechanical guides, but as intraoperative pelvic positioning varies, especially in the lateral position [5] these techniques often result in inaccurate cup anteversion with cups placed outside the predefined safe zone as described by Lewinnek et al. (i.e. anteversion of 15 ± 10°) [6-12].
In revision surgery loss of bone stock can make reconstruction of the failed acetabular component challenging, and intraoperative landmarks that are mandatory for appropriate cup orientation may be deteriorated. However, there is no published information about acetabular component orientation with freehand techniques in revision surgery of the failed acetabular component. Furthermore, no studies have compared cup anteversion in revision with primary THA surgery.
In this observational study we obtained CT scans postoperatively with the patient in supine position to measure the version of the acetabular component in patients who underwent revision and primary THA to answer what is the range of cup anteversion actually achieved in revision surgery to clarify whether there are differences in revision as compared to primary cases of THA. Our null hypothesis was that there are no differences in acetabular component version between primary and revision THA with the use of a cup positioner with an alignment frame.
PATIENTS AND METHODS
The study was approved by the local ethical committee and performed in accordance with the ethical standards of the 1964 Declaration of Helsinki as revised in 2000. It was prospectively performed in 97 patients (97 hips). Seventy-one patients (48 women and 23 men) aged 45 to 90 (mean 65) years underwent cementless primary THA, and 26 patients (19 women and 7 men) aged 47 to 81 (mean 70) years underwent cementless acetabular revision surgery 8 to 16 years after primary THA. The patients were operated during the year 2008, and they were consecutively enrolled in the study. In revision surgery we intend to obtain at least 50% contact between a cementless cup and host bone, and if the preferable version was not possible because of major acetabular defects as judged by the surgeon, we had to compromise between the preferred version and bone contact of the cup, and these cases were excluded from the study, which left 26 revision patients to be included.
Five senior surgeons at our hospital operated the patients, and they were all informed of the study. The operations were performed with the patients in the lateral position, using a standardized lateral or posterior approach. In all cases we used a porous coated hemispherical press fit cup (Trilogy, Zimmer, Warsaw, In, USA), and we aimed to obtain acetabular antversion of 10 to 30° using a cup positioner with an alignment connector and frame provided with the implant. This is designed to obtain 20° of anteversion if the alignment rod is in line with the longitudinal axis of the patient. In all the primary cases we obtained press fit stabilization of the implant shell, while it is our routine to secure the implant shell with 2-3 screws in revision cases (Figs. 1, 2). We used elevated liners to provide optimal femoral head coverage, and we used ceramic heads with a diameter of 28 mm.
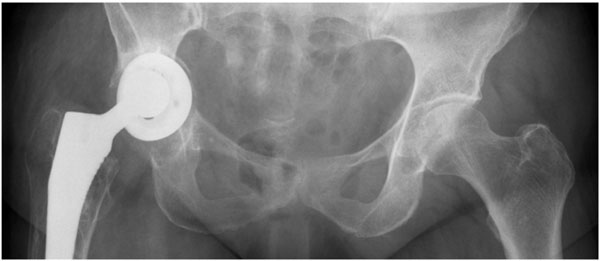
Failed acetabular component.
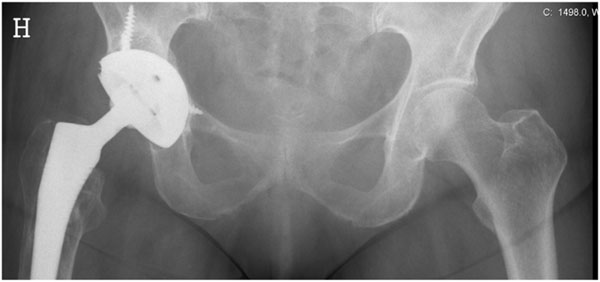
Revision of the failed acetabular component.
At 3 months postoperatively, and after informed consent in all patients, acetabular and femoral component version was measured using CT (General Electric LightSpeed Pro 16 Milwaukee, Wi, USA). Single scans, 5 mm of thickness, were made through the centre of the femoral head, and we defined acetabular component version as the angle between a line connecting the lateral anterior and posterior margins of the acetabular component and the coronal plane defined as the plane perpendicular to a line connecting 2 identical points on either side of the pelvis (Fig. 3). The same specialist in radiology made all assessments.
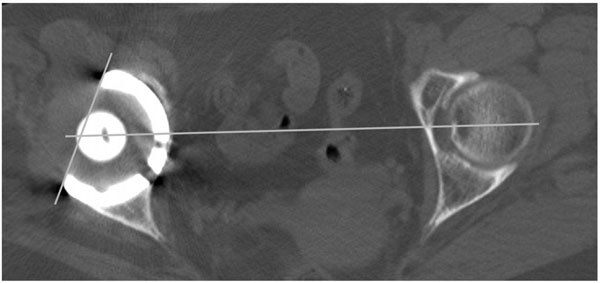
Anteversion of the revised acetabular component defined as the angle between a line connecting lateral anterior and posterior margins of the component and the sagittal plane defined as the plane perpendicular to a line connecting two identical points on either side of the pelvis.
Descriptive statistics is mean, standard deviation, 95% confidence interval (CI) and ranges. Differences between groups were tested using a two-sample t-test. P<0.05 was considered significant. Power analyses were not performed because aiming of cup position as well as results are differently described in the literature and there are no data on cup positioning in revision THA. Thus, power calculations would be questionable.
RESULTS
The acetabular component version in the primary hips as measured from the CT scan ranged from 28° of retroversion to 42° of anteversion with a mean of 17.4 ± 14.0° (CI 14.1°, 20.7°), while the cup version in the revision hips ranged from 4° of retroversion to 32° of anteversion with a mean of 15.0 ± 9.6° (CI 11.1°, 18.9°) (p=0.427) (Fig. 4). The anteversion of 40 (56%) of the primary acetabular components were within the target zone of 10 to 30°, while 19 (27%) were below the target zone and thus was surgically overestimated, and 12 (17%) were above the target range and thus was surgically underestimated. The anteversion of 19 (73%) of the revision acetabular components were within the target zone, while 6 (23%) were below the target zone and thus were surgically overestimated, and 1 (4%) were above the target range and thus was surgically underestimated. The differences in distribution between the primary and revision operations were not significant (p=0.183) (59% versus 63% within the target zone).
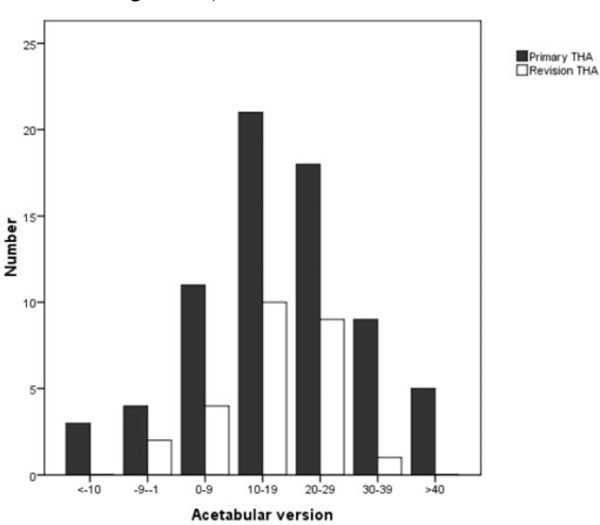
Distribution of acetabular component version in patients operated with primary or revision total hip arthroplasty.
There were no significant differences in acetabular component version between the cases operated by posterior (16.8 ± 12.7°, CI 13.1°, 20.6°) versus direct lateral approach (17.3 ± 12.9°, CI 14.4°, 20.2°), and the cups were positioned in 59% versus 63% within the target zone. During a 4-5 years follow up there have been no dislocations or other complications.
DISCUSSION
Improper acetabular component orientation negatively affects the outcome of total hip arthroplasty. With conventional techniques, numerous variables may contribute to variability in cup positioning during surgery. We found that using a cementless porous coated and hemispherical cup, there was a wide range of component version, but this was not significantly different in revision as compared to primary THA. Our null hypothesis that there are no differences in acetabular component version between primary and revision THA with the use of a cup positioner with an alignment frame was confirmed. The clinical impact is that a cup positioner with an alignment frame in revision of the acetabular component may be as reliable as in primary THA.
Strength of our study is that we used the same type of acetabular prosthesis in all cases. It has been shown that different types of prostheses may influence the results [13]. A weakness of the study is that 5 different surgeons might operate the cup positioner differently. However, this might also be considered strength of the study, as it is regular in orthopedic practice that there are different surgeons doing THA at the hospitals. It has been shown that senior surgeons do better than residents [13]. In our study the surgeons were all experience, and no one differed systematically form the others in doing cup positioning. Another weakness of the study is that we used two different surgical approaches, but as there were no differences between them in cup positioning, we consider this as a minor weakness.
The use of CT to measure cup version is considered more accurate than plain radiography with a standard deviation of interobserver error of about 3° [14-16]. But even CT studies of the cup position should be interpreted with caution because there are variations of the pelvic orientation depending on patient positioning, and different conventions are used to describe the cup orientation [17-19]. The patients were CT examined in the supine position while they were operated in the lateral decubitus position. In the lateral decubitus position correct positioning of the patient may be more difficult than in the supine position because the true anatomic conditions can just be approximated [20, 21].
We used an uncemented cup, and in all our revision cases we had more than 50% contacts between the cup and the host bone as evaluated by the surgeon. In reconstructions of the failed acetabular component, a porous-coated cup secured to host bone with multiple screws is a method of choice [22]. For the intraoperative assessment of cup orientation, anatomic landmarks is mandatory, but loss of bone stock in our revision cases did not influence cup positioning as compared to primary THA with the use of the acetabular cup positioner. In all revision cases we used screws than may slightly have modified the position of the implant shell. However, this could hardly have been of any significance as there were no differences between the primary cases were no screws were used and the revision cases.
In a retrospective CT-controlled study, Saxler et al. [8] showed that only 27 out of 105 cups (26%) in primary THA were placed within the safe zone of Lewinnek [6]. In a second study DiGioa et al. [7] used a specific mechanical acetabular alignment guide, and the results were controlled preoperatively with a hip navigation system. In 74 hips only 22% of the cups were placed within the Lewinnek’s safe zone. In these studies there was a tendency to underestimate the anteversion of the acetabular component. We therefore aimed to position the cup 5° more anteverted than the safe zone of Lewinnek, and our data demonstrate better accuracy of cup positioning. We overestimated the acetabular component version more frequently than it was underestimated in relation to our intraoperative aim. However, it has been shown that CT measurements of the acetabular anteversion in the supine position are about 10 degrees lower than in the standing position as evaluated by biplanar imaging [23]. On the other hand, as compared to the safe zone of Lewinnek more cups were positioned above this zone than below. Coventry et al. [24] found a significant association between acetabular retroversion and posterior dislocation. On the other hand, Lewinnek et al. [6] reported a higher incidence of anterior dislocations in THA with more than 25° of acetabular component anteversion. Then, both excess anteversion and retroversion need to be avoided to prevent dislocation. However, the risk factors that predispose to dislocation are multivariate and include patient-related, operative and implant design variables [25]. We used a rather small head, but malpositioning and the use of a small head in our series may have been compensated for by the elevation of the polyethylene insert. During a follow-up period of 4-5 years we have had no dislocations.
At present, computer navigation system seems to be a most reliable tool for cup positioning [8, 10, 26, 27]. However, the use of this system is not widely adopted due to its high costs, complexity and operating time, and individual studies are too small to allow conclusive statements on the potential benefit. Alignment guides have been developed to improve free hand techniques in cup positioning, but still we found variable accuracy of cup positioning both in primary and revision THA. The reason that the variability was equal in primary and revision cases may be that the alignment rod is positioned according to the body axis and loss of bone stock in revision cases thereby is of less significance. The clinical application of our study is that we would recommend an increased target zone from 10° to 30° rather than the safe zone defined by Lewinnek.
Apart from cup orientation, outcomes of THA such as longevity, range of motion, impingement and dislocation further depend on the head-neck ratio, the offset and the stem orientation [28, 29]. In addition, surgical approach and endogenous factors such as comorbidity and muscular status may contribute to the fate of the hip joint [30, 31]. In our study we found variable accuracy of acetabular cup positioning, but with the use of an acetabular positioner that relies on the body axis there are equal results in revision as in primary THA.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


