All published articles of this journal are available on ScienceDirect.
An ICON Overview on Physical Modalities for Neck Pain and Associated Disorders
Abstract
Introduction:
Neck pain is common, can be disabling and is costly to society. Physical modalities are often included in neck rehabilitation programs. Interventions may include thermal, electrotherapy, ultrasound, mechanical traction, laser and acupuncture. Definitive knowledge regarding optimal modalities and dosage for neck pain management is limited.
Purpose:
To systematically review existing literature to establish the evidence-base for recommendations on physical modalities for acute to chronic neck pain.
Methods:
A comprehensive computerized and manual search strategy from January 2000 to July 2012, systematic review methodological quality assessment using AMSTAR, qualitative assessment using a GRADE approach and recommendation presentation was included. Systematic or meta-analyses of studies evaluating physical modalities were eligible. Independent assessment by at least two review team members was conducted. Data extraction was performed by one reviewer and checked by a second. Disagreements were resolved by consensus.
Results:
Of 103 reviews eligible, 20 were included and 83 were excluded. Short term pain relief - Moderate evidence of benefit: acupuncture, intermittent traction and laser were shown to be better than placebo for chronic neck pain. Moderate evidence of no benefit: pulsed ultrasound, infrared light or continuous traction was no better than placebo for acute whiplash associated disorder, chronic myofascial neck pain or subacute to chronic neck pain. There was no added benefit when hot packs were combined with mobilization, manipulation or electrical muscle stimulation for chronic neck pain, function or patient satisfaction at six month follow-up.
Conclusions:
The current state of the evidence favours acupuncture, laser and intermittent traction for chronic neck pain. Some electrotherapies show little benefit for chronic neck pain. Consistent dosage, improved design and long term follow-up continue to be the recommendations for future research.
INTRODUCTION
Description of the Condition
Neck pain is common, can be disabling and is costly to society. Twenty-six to 71% of the adult population can recall experiencing an episode of neck pain or stiffness in their lifetime [1-3]. Although most people with neck disorders experience a low level of disability, Cote 1998 found that 5% were significantly disabled. The prevalence of neck pain is higher in females [4-7]. The results of The Bone and Joint Decade 2000-2010 Task Force on Neck Pain reveal 12-month neck pain prevalence estimates ranging from 30% to 50% in the adult general population generally rising to middle age and then declining in later life [7]. In a U.S. study from the National Ambulatory Medical Care Survey, an average of 10.2 million visits to health care facilities for neck pain was reported [8]. Neck pain has a large impact on health care expenditure, attributed to visits to healthcare providers, sick leave and is responsible for significant disability and loss of productivity [9-11].
Description of the Intervention
The primary approach to neck pain is conservative management. Physical modalities are often a component of these management programs. Interventions may include various forms of heat and cold application, electrotherapy, ultrasound, mechanical traction, laser and acupuncture. Ultrasound is one of the most widely used modalities yet conflicting or limited evidence exists regarding its effectiveness [12, 13]. Previous to this current overview, Gross 2002 [14] and Spitzer 1995 [15] found thermal agents to be commonly used in addition to manual therapy, exercise, education and drug therapies for acute and chronic neck pain. Since physical agents are used as adjunctive interventions, it can be difficult to determine what contribution they make to augmenting treatment effects. Previous reviews have questioned the benefit of physical agents. Gross 2007 [16] found evidence of no benefit for the use of hot packs for both intermediate and long-term relief of chronic pain or improved function. In addition, infrared light and spray and stretch did not aid in short-term pain reduction. Two systematic reviews, one examining non-invasive treatment for trigger point pain [17] and the other on conservative treatment for acute neck pain not due to whiplash [18] did not report on any studies that included heat or cold therapy. Electrotherapy [Electrical Nerve Stimulation, Electrical Muscle Stimulation, Pulsed Electrical Magnetic Field] has been commonly used as one of the physiotherapeutic options to treat neck pain for many years [19]. Little is known about the efficacy of most of these subtypes as sound empirical evidence is lacking. An updated Cochrane review [19] still could not evaluate the unique contribution of electrotherapy since studies had not examined their effects in isolation. Mechanical traction is another treatment with limited evidence of effectiveness [20-24]. According to a number of existing reviews, moderate evidence suggests that acupuncture is effective in the short term for relieving neck pain [16, 25-28]. LASER is a conservative method of treating neck pain that has received relatively limited attention in the scientific literature to date.
How the Interventions Might Work
We consider the different physiological and clinical rationale for the use of various physical modalities used by clinicians.
HEAT AND COLD
Heat and cold can be applied in multiple ways ranging from in-clinic devices to home applications, with varying thermal properties that can influence physiological effects. Therapeutic applications may include cold packs, evaporative cooling spray, superficial moist heat, shortwave diathermy, infrared heat and hydrotherapy. These therapies can assist in the healing process by providing physiological changes to a range of tissues [29] including changes in blood flow, nerve conduction, and metabolic function. Since the biophysical properties differ across cold and heat agents, the capability of reaching particular target tissues varies across modalities [29-32].
ULTRASOUND
Therapeutic ultrasound is a form of acoustic energy (sound) that has been used in rehabilitative medicine for over fifty years [33]. It is used for the purpose of stimulating soft tissue repair and inflammation management thereby resulting in the relief of pain [34] and also for bone healing [35]. Ultrasound is considered a 'deep heating modality' as it is able to increase the temperature of tissues at a much greater depth than superficial heat through the mechanical effects of sound vibration. It should be noted however, that ultrasound can be used without producing a significant rise in tissue temperature [34]. It is believed that ultrasound application increases blood flow and metabolism at the site of injury, and can thereby decrease pain and increase the rate of healing [33, 34].
MECHANICAL TRACTION
Mechanical traction for the cervical spine involves a longitudinal force applied to the neck via a mechanical system that is delivered intermittently or continuously [36]. It is often used as an adjunct therapy in outpatient rehabilitation [29]. The physiological effects of mechanical traction for the cervical spine may include separation of vertebral bodies, movement of facet joints, expansion of intervertebral foramen and stretching of soft tissue [29, 36].
ELECTROTHERAPY
Electrotherapy treatment may include: Direct current (DC), iontophoresis, electrical nerve stimulation; electrical muscle stimulation; transcutaneous electrical nerve stimulation (TENS); pulsed electromagnetic fields, repetitive magnetic stimulation and permanent magnets (albeit extremely small current). Treatment by DC or Galvanic current, reduces pain by inhibiting nociceptor activity [37]. The main indication for Galvanic current is the treatment of acute radicular pain and inflammation of periarticular structures such as tendons and ligaments. Alternating electrical current (AC) or modulated DC (Galvanic stimulation) may be effective by inhibiting pain-related potentials on the spinal and supraspinal level. Pain relief can be obtained through possible endorphinergic mechanisms of analgesia with the use of electrical muscle stimulation, TENS, or other forms of electrical nerve stimulation [38].
ACUPUNCTURE
Acupuncture has been increasingly used as an alternative to more traditional treatments for musculoskeletal pain. It is defined as the stimulation of a certain point(s) on the body, by the insertion of needles, to achieve a desirable effect. It is believed to prevent or modify the perception of pain or to alter physiological functions, including pain control for the treatment of certain diseases or dysfunction of the body [39]. One theory from western scientific research suggests that acupuncture promotes the release of endorphins from the brain through the stimulation of peripheral nerves. These endorphins then block pain pathways in the brain [40]. Traditional Chinese Medicine tracing back thousands of years, encompasses the ancient philosophy of Taoism and the concept of universal balance between Yin and Yang. To balance one’s energy by either sedating or stimulating acupuncture points, promoting the flow of Qi (life’s energy) and thereby restoring health [41, 42].
We acknowledge and respect the variations in the underpinning theory and practical application of acupuncture and related challenges it poses to our evaluation of this intervention and potential subtypes.
LASER
The term LASER is an acronym for light amplification by stimulated emission of radiation-a form of photonic therapy that uses monochromatic light with either high or low power [34]. Low power LASER devices have little to no thermal effects and are used to treat an array of musculoskeletal conditions to decrease pain, inflammation and soft tissue scars, and to promote fracture healing [34, 43-45]. Three main types of LASER are used clinically: helium-neon (HeNe wavelength 632.8nm, tissue penetration 0.8mm), the gallium-arsenide (GaAs 904nm, penetrating 5cm) and the gallium-aluminum-arsenide (GaAlAs 830nm, penetrating 2-3cm) [34, 43]. Many mechanisms of action have been proposed for LASER including the slowing of transmission of nociceptive signals, regulation of serotonin and norepinephrine and may limit the release of pro-inflammatory mediators [34, 46-48].
MULTIMODAL TREATMENTS
Multimodal treatment plans are common in outpatient rehabilitation with physical modalities often used as a component of the total intervention. Modalities are typically not used exclusively. For that reason, many randomized trials do not examine the use of modalities in isolation but rather in combination with other treatments such as exercise or manual therapy. It is common to see one group of interventions compared to a completely different set of combined interventions. These types of studies may determine a treatment grouping that is more effective than another. Although this makes clinical sense, the independent contribution of a particular modality alone cannot be evaluated and designs that might disaggregate the separate treatment effects are rarely used [49]. Clinically, these various modalities are used for improving physiologic functions that promote healing; or, short-term pain reduction, improved joint and muscle motion. Also, modalities are sometimes used prior to exercise to improve exercise tolerance.
Why it is Important to do this Overview
Conflicting or unclear evidence regarding the effectiveness of physical modalities for whiplash-associated disorders (WAD) remains prominent in the literature due in part to poor methodological quality of efficacy trials [23, 50]. Despite more recent studies over the last decade with sound methodology, the best evidence for treatment of WAD patients remains relatively unchanged [51]. The evidence for treatment of cervicogenic headache and radiculopathy are underrepresented in the current literature and there is no evidence of the optimal dosage of non-invasive treatments [51]. Chronic neck pain accounts for $150-$200 billion US each year in economic loss due to lost work days and rehabilitation, yet relatively little is known about how best to manage this condition [16, 52, 53]. Overall, limited definitive knowledge as to what modalities including dosage is most effective to address the management of neck pain.
The purpose of this overview was to systematically review existing reviews and to establish the evidence-base recommendations on the treatment of acute to chronic neck pain (specific and non-specific) with physical modalities. These included heat and cold application, electrotherapy, ultrasound, mechanical traction, laser and acupuncture. We specifically focused on evidence that evaluated use of physical modalities for reducing pain and improving function, quality of life, patient satisfaction or global perceived effect compared to a control with immediately post treatment to long term follow up.
METHODS
Our systematic overview process included comprehensive computerized search strategies including MEDLINE, EMBASE, CINAHL, ILC, CENTRAL and LILACS from January 2000 to August 2010, selection criteria (Table 1). Independent assessments by at least two members of our review team were performed for a systematic review of methodological quality using the AMSTAR tool [54], qualitative assessment of the strength of evidence using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach [55, 56] and the recommendation presentation. Two separate searches were performed, one for treatment and one for harms. This methodology is detailed in our International Collaboration on Neck (ICON) methods report [57] including full search terms; this protocol was not registered. Further, we complemented this search by identifying on-going systematic reviews near completion such as Cochrane Reviews up to July 2012, by contacting our expert panel and by systematically checking reference lists of primary studies to minimize the risk of missing relevant reviews and trials.
Inclusion and Exclusion Criteria Set a Priori
| PICOSS | Criteria |
|---|---|
| Participant | Adult (≥18 year), acute to chronic neck pain with or without cervicogenic headache or radiculopathy or whiplash |
| Intervention | Acupuncture, electrotherapy, laser, cold or heat, mechanical traction, ultrasound as single treatment |
| Comparison | Control or comparison (i.e. standard care, another treatment) |
| Outcomes |
Primary: Pain, function, disability, work related, quality of
life Secondary: global perceived effect and patient satisfaction |
| Study Design | Systematic reviews of randomized trials; narrative reviews were excluded |
| Study Timeframe | Immediate post-treatment (IP), short-term (ST: closest to 3 months); intermediate term (IT: closest to 6 months; long term (LT: closest to 1 year) |
Data extraction was performed using pre-piloted forms by one reviewer and checked by a second with disagreements resolved by consensus. We systematically extracted data from selected reviews and developed evidence tables. Extractable data from the reviews included the following: author, year of publication, disorder type with duration of symptoms, the intervention, the type of comparator (placebo, no care, usual care, other treatment), the search period, the original authors of primary studies, the AMSTAR score, the effect direction, effect size for reported primary outcomes with duration follow-up period, reported harms, quality ranking system, evidence statement and final GRADE. Harm information was summarized qualitatively from both the treatment reviews that reported any adverse events and directly from the harms reviews.
We utilized the following triage rules (set a priori) to guide decisions and to group treatment reviewed:
- Type of treatment was used to group reviews by physical modality (heat and cold application, electrotherapy, ultrasound, mechanical traction, laser and acupuncture).
- Within a treatment modality we grouped review data with respect to comparator treatments.
- Once the studies had been grouped by these two categories, a decision was made PER grouping; if there were few reviews within a treatment category and with unique comparators, we did not eliminate any further reviews.
- If there were several reviews on the same treatment and comparator, we prioritized to obtain the best quality reviews by considering the approach recommended by Whitlock et al. [58] as follows:
-
Year of publication. Within the group of systematic reviews
- If there were reviews that were very similar across multiple years, we focused on reviews that were the most up-to-date AND if the studies included in the older review were also INCLUDED in the more recent review.
- We cross-checked to ascertain that the conclusions were similar to the more current systematic review.
- AMSTAR- Risk of Bias. Reviews were considered low risk of bias if they scored 8 or higher on the 11-point AMSTAR scale, moderate risk of bias if scored between 5 and 7, and high risk of bias if scored 4 or under. We used this process to focus on the best quality reviews. These were synthesized in a summary of findings table to help provide definitive summaries to inform clinical practice (Table 2). Inconsistency and discordance were highlighted and discussed in our methods paper [57].
Table 2.AMSTAR Rating
Ref# Author 1 2 3 4 5 6 7 8 9 10 11 107 Baxter et al. 2008 Y N Y N N Y Y Y NA N N 4408 Bronfort et al. 2009 Y Y Y Y Y Y Y Y NA N N 157 Bronfort et al. 2010 Y N Y N N N Y Y NA N N 1737 Chow & Barnsley 2005 Y N Y Y Y Y Y N NA N N 15 Chow et al. 2009 Y Y Y Y N Y Y N Y Y N 1747 Conlin et al. 2005 Y N Y N N Y Y Y Y N N 25234 Ernst et al. 2011 Y CA Y N N Y N NA NA N N 106 Fu et al. 2009 Y Y Y N Y Y Y N Y N N 20018 Furlan et al. 2010 Y Y Y Y Y Y Y Y Y N N 87 Graham et al. 2006 Y Y Y Y N Y Y Y Y N N 46 Graham et al. 2008 Y Y Y Y Y Y Y Y Y N N 20024 Graham et al. 2008 Y Y Y Y Y Y Y Y Y N N 69 Gross et al. 2007 Y Y Y Y N Y Y Y Y N N 5 Gross et al. 2010 Y Y Y Y Y Y Y Y Y N N 20041 Gross et al. 2012 Y Y Y Y N Y Y Y Y Y N 36 Haines et al. 2009 Y Y Y Y Y Y Y Y Y N N 83 Haraldsson et al. 2006 Y Y Y Y Y Y Y Y Y N N 53 Hurwitz et al. 2008 Y N N Y N Y Y Y NA N N 193 Itoh & Kitakoji 2007 Y Y Y N N Y Y Y NA N N 166 Kay et al. 2009 Y Y Y Y Y Y Y Y Y N N 12 Kroeling et al. 2009. Y Y Y Y Y Y Y Y Y N N 20048 Kroeling et al. 2013 Y Y Y Y Y Y Y Y NA N N 1445 Las Penas et al. 2005 Y N Y N N Y Y Y NA N N 7575 Leaver et al. 2010 Y Y Y N N Y Y Y Y N N 149 Lee et al. 2010 Y Y Y N N CA Y Y NA N N 145 Lin et al. 2009 Y Y Y N Y CA N NA N N N 303278 Lin et al. 2012 Y Y Y Y Y Y Y Y NA N N 6020 Miller et al. 2010 Y Y Y Y N Y Y Y Y N N 3333 Peake & Harte, 2005 Y N Y N N Y Y Y NA N N 495 Peloso et al. 2007 Y Y Y Y Y Y Y Y Y Y N 1432 Reid & Rivett 2005 Y CA Y N N Y Y Y NA N N 226 Rickards 2006 Y N Y N Y Y Y Y NA N N 241 Teasell et al. 2010 Y N Y N N Y Y Y NA N N 11690 Teasell et al. 2010 Y N Y N N Y Y Y NA N N 25360 Trinh et al. 2006 Y Y Y Y Y Y Y Y Y N N 213 Trinh et al. 2007 Y Y Y Y Y N Y Y Y N N 170 Tsakitzidis et al. 2009 Y Y Y Y N Y Y Y NA N N 185 Verhagen et al. 2007 Y Y Y N Y Y Y Y Y N N 75 Vernon & Humphreys 2007 Y N Y N N Y Y Y NA N N 413 Vernon & Schneider 2009 Y N Y N N N Y Y NA N N 1736 Vernon et al. 2005 Y CA Y N N Y Y Y NA N N 511 Vernon et al. 2006 Y N Y N Y Y Y N NA N N 71 Vernon et al. 2007 Y Y Y N Y Y Y Y NA N N 473 Wang et al. 2008 Y Y Y N Y Y Y Y Y N N 99 Wang et al. 2009 Y Y N N N Y N NA NA N N 57 Williams et al. 2007 Y Y Y N N Y Y Y Y N N Key: Y-Yes; N -No; NA-not applicable; CA-can`t assess AMSTAR Questions:
- Was an 'a priori' design provided? The research question and inclusion criteria should be established before the conduct of the review.
- Was there duplicate study selection and data extraction? There should be at least two independent data extractors and a consensus procedure for disagreements should be in place.
- Was a comprehensive literature search performed? At least two electronic sources should be searched. The report must include years and databases used (e.g. Central, EMBASE, and MEDLINE). Key words and/or MESH terms must be stated and where feasible.
- Was the status of publication (i.e. grey literature) used as an inclusion criterion? The authors should state that they searched for reports regardless of their publication type. The authors should state whether or not they excluded any reports.
- Was a list of studies (included and excluded) provided? A list of included and excluded studies should be provided.
- Were the characteristics of the included studies provided? In an aggregated form such as a table, data from the original studies should be provided on the participants, interventions and outcomes. The ranges of characteristics in all the studies analyzed e.g. age, race, sex relevant socioeconomic data, disease status, duration, severity, or other diseases should be reported.
- Was the scientific quality of the included studies assessed and documented? 'A priori' methods of assessment should be provided (e.g., for effectiveness studies if the author(s) chose to include only randomized, double-blind, placebo controlled studies or allocation concealment as includion criteria); for other types of studies alternative items will be relevant.
- Was the scientific quality of the included studies used appropriately in formulating conclusions? The results of the methodological rigor and scientific quality should be considered in the analysis and the conclusions of the review, and explicitly stated in formulating recommendations.
- Were the methods used to combine the findings of studies appropriate? For the pooled results, a test should be done to ensure the studies were combinable, to assess their homogeneity (i.e. Chi-squared test for homogeneity, 2). If heterogeneity exists a random effects model should be used and/or the clinical appropriateness of combining should be taken into consideration (i.e. is it sensible to combine?)
- Was the likelihood of publication bias assessed? An assessment of publication bias should include a combination of graphical aids (e.g., funnel plot, other available tests) and/or statistical tests (e.g., Egger regression test).
- Was the conflict of interest stated? Potential sources of support should be clearly acknowledged in both the systematic review and the included studies.
-
Year of publication. Within the group of systematic reviews
- Effect Size estimates: We selected the effect size as the primary summary measure for our overview. We determined that within a grouping for treatment and comparator, we selected a review to represent the BEST estimate of effect size or related meta-analysis and as needed reported the range of estimates for other included reviews. In cases where there was discordance between reviews, we reported the combined results of the individual included studies. Additional data on magnitude of effect such as number-needed–to-treat (NNT) and weighted mean difference (WMD) were extracted when available.
- Strength of Evidence using GRADE approach: We used this same representative systematic review or meta-analysis from which to judge an overall GRADE for the strength of the body of evidence for treatment. This did not include the harms evaluation that was observational. The selected reviews may have already had a GRADE table. We estimated the quality of the evidence using the GRADE approach for primary trials within reviews using reported information on: design [randomized controlled trials (RCT), immediately post treatment to long term follow-up]; risk of bias (equivalent methodological criteria for risk of bias reported in the review i.e. JADAD [59] or PEDro [60]); imprecision (sample size); inconsistency; indirectness; and reporting bias.
We excluded reviews that did not meet our inclusion criteria with rationale for exclusion. Multimodal treatments were not included if contributions of individual interventions could not be determined. Once reviews were deemed relevant and of at lower risk of bias, we extracted and reported individual trial findings by “overall strength of evidence” using GRADE approach and stratified by “treatment category” for the Summary of Findings Table (Table 3). Conflicting evidence was recorded (Table 4). The final core recommendations are reported in Evidence-Based Recommendations (Table 5).
Summary of Findings by GRADE (Quality of Evidence)
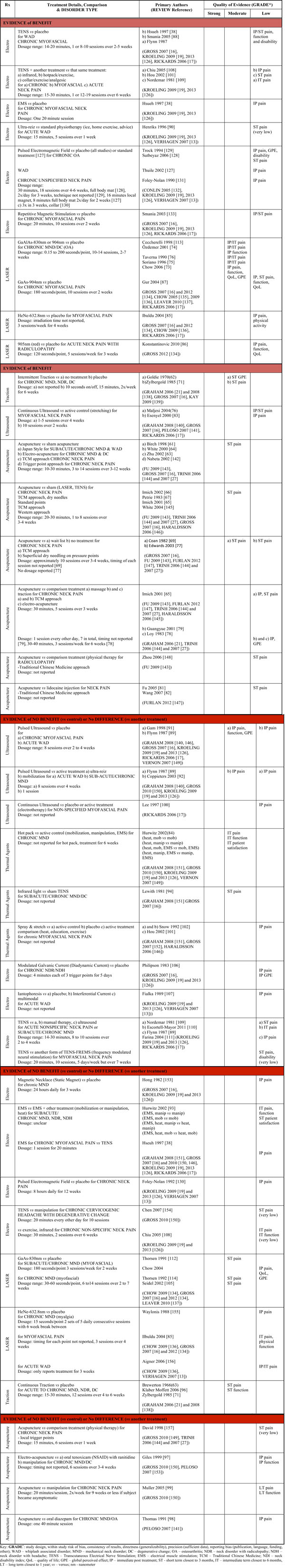 |
Evidence-Based Recommendations
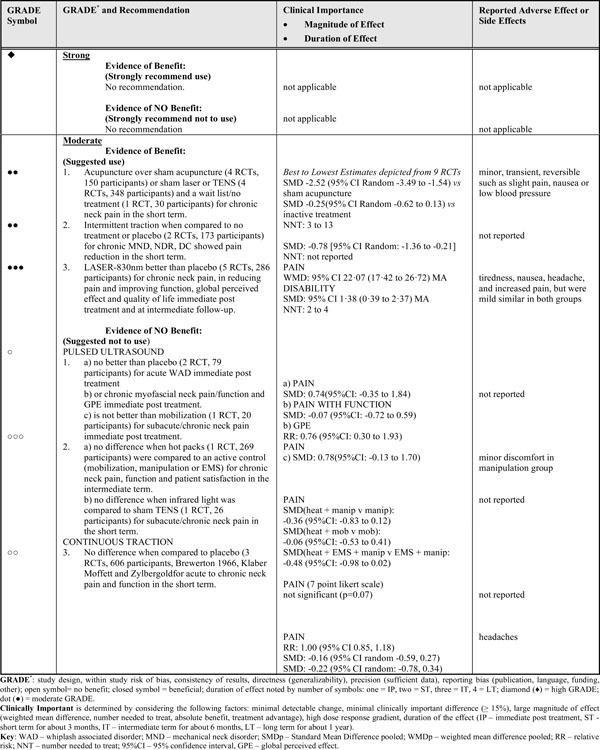 |
RESULTS
From 117 reviews that were identified for the entire ICON treatment category, 103 were screened for eligibility. From these, a total of 48 reviews evaluated the physical modalities of interest, with 20 reviews included (Fig. 1 – PRISMA diagram). Eighty-three reviews were excluded, detailed reasons can be found in APPENDIX 1.
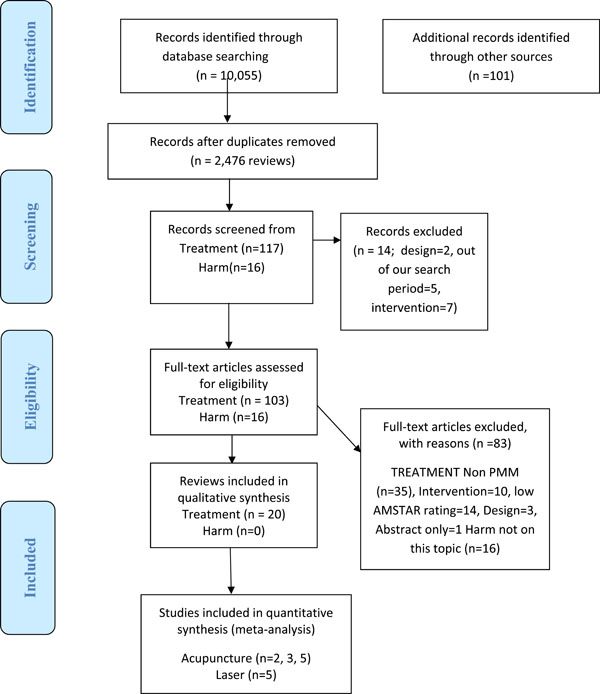
PRISMA diagram showing the flow of reviews for Physical Medicine Methods (PMM).
Those systematic reviews that scored less than six on the AMSTAR assessment were not included. The AMSTAR assessment disclosed that the most common methodological limitations included incomplete reporting on: publication bias; conflict of interest; and complete reporting of excluded studies [57]. The primary reviews included in our analyses evaluated the evidence on the following physical modalities: thermal, electrotherapy, ultrasound, mechanical traction, laser and acupuncture. Treatment parameters varied across interventions and some were not reported at all. Treatment dosages have been reported when available.
EVIDENCE OF BENEFIT
Strong Evidence
There was no strong evidence to support or discount the use of any of the modalities in this overview.
Moderate Evidence
Acupuncture
We found acupuncture to be more beneficial relative to sham acupuncture (4 RCTs, 150 participants) [61-64] or sham laser or TENS (4 RCTs, 348 participants [65-68]) and a wait list or no treatment (1 RCT, 30 participants) [69] for pain reduction in the short term in patients with chronic mechanical neck disorder.
Low or Very Low Evidence
Acupuncture
Acupuncture was shown to be better than no treatment (1 RCT, 40 participants) [77] for chronic myofascial neck pain in the short term.
We found acupuncture to be more beneficial for chronic neck pain than massage (1 RCT, 177 participants) [65] immediate post treatment and in the short term and better than traction (2 RCTs, 589 participants) [78, 79] for global perceived effect immediately following treatment.
We found acupuncture to be more beneficial than multimodal physical therapy (details not reported) (1 RCT, number of participants not reported) [80] for radicular pain in the short term. We found acupuncture to be more beneficial than the injection of lidocaine (2 RCT, number of participants not reported) [81, 82] for non-specific neck pain in the short term.
Ultrasound
Continuous ultrasound was better than a control immediately post treatment and in the short term (2 RCTs, 150 participants) [83, 84] for myofascial pain. High-powered pain threshold with the probe placed over the trigger point and held motionless was more beneficial than conventional ultrasound (1 RCT, 60 participants) [84] for myofascial pain immediately post treatment.
LASER
HeNe-632.8nm with exercise (1 RCT, 60 participants) [85] was shown to be better than placebo for chronic myofascial pain immediately post treatment but not at intermediate follow-up of six months. GaAlAs-830nm or 904nm (4 RCTs, 196 participants) [72, 74, 75] was better than placebo for subacute/chronic neck pain with associated osteoarthritis. 905nm-red (1 RCT, 60 participants) [86] was shown to be better than placebo for improving disability in acute neck pain with radiculopathy immediately following treatment. GaAs-904nm was better than placebo (1 RCT, 60 participants) [87] for reducing myofascial neck pain, improving function and quality of life immediately post treatment and in the short term.
Electrotherapy
TENS
TENS (3 RCTs, 88 participants) [38, 88, 89] was more beneficial for pain reduction when compared to placebo for myofascial pain or WAD of unspecified duration immediately following treatment. Ultra-Reiz, a form of TENS (1 RCT, 16 participants) [90] was more beneficial for reducing acute WAD pain when compared to standard physiotherapy including ice, home exercise and advice in the short term. TENS was beneficial for reducing chronic myofascial neck pain (1 RCT, 60 participants) [38] when compared to electric muscle stimulation immediately post treatment.
EVIDENCE OF NO BENEFIT (VS CONTROL) OR NO DIFFERENCE (VS ANOTHER TREATMENT)
Moderate Evidence
Ultrasound
Pulsed ultrasound was no better than placebo (2 RCT, 79 participants) [89, 91] at changing function or global perceived effect immediately post treatment in patients with either acute WAD or chronic myofascial neck pain. Also, ultrasound was inferior to mobilization (1 RCT, 20 participants) [92] for subacute/chronic neck pain immediately post treatment.
Thermal Agents
There was no difference between hot packs (1 RCT, 269 participants) [93] and an active control (mobilization, manipulation or EMS) at improving pain, function and patient satisfaction in the intermediate term for patients with chronic mechanical neck disorder. There was no difference when infrared light was compared to sham TENS (1 RCT, 26 participants) [94] for subacute/chronic neck pain in the short term.
Low or Very Low Evidence
Acupuncture
There was no difference found when electro (1 RCT, 62 participants) [97] or non-stimulated acupuncture (1 RCT, 132 participants) [98] for chronic mechanical neck disorder with degenerative changes was compared to manipulation or medication-tenoxicam (NSAID) with ranitidine or diazepam respectively for improving pain or function immediately following treatment. Additionally, no difference was found between acupuncture and manipulation for chronic neck pain (1 RCT, 69 participants) [99] at long term follow-up.
Ultrasound
Pulsed ultrasound was inferior to ultra-reiz (1 RCT, 21 participants) [89] for acute WAD immediately post treatment. Continuous ultrasound was not beneficial when compared to placebo and inferior to an active treatment (electrotherapy, type not specified) (1 RCT, 26 participants) [100] for reducing myofascial neck pain immediately post treatment.
Thermal Agents
No difference was found when spray/stretch was compared to an active control, placebo or active treatment (heat, education, exercise) (2 RCTs, 72 participants) [101, 102] for reducing chronic myofascial neck pain immediately post treatment.
LASER
For Helium Neon 632.8nm (1 RCT, 55 participants) [103] there was no benefit for pain relief when compared to placebo immediately following treatment for chronic myofascial pain syndrome. For pain reduction, GaAs 830nm was inferior to manipulation (1 RCT, 38 participants) [104] for cervicogenic headache or acupuncture (1 RCT, 12 participants) [105] for chronic tendomyositis both in the short term.
Electrotherapy
Modulated Galvanic Current
There was no benefit for improving chronic neck pain and global perceived effect (1 RCT, 40 participants) [106] compared to placebo immediately post treatment.
Iontophoresis
There was no benefit when iontophoresis was compared to no treatment, interferential current and was inferior to a multimodal approach of traction, exercise and massage (1 RCT-3 arms) [107] for improving pain in patients with acute WAD with cervicogenic headache immediate post treatment.
TENS
There was no benefit when TENS was compared to placebo (1 RCTs, 53 participants) [88] for reducing pain in patients with chronic mechanical neck disorder immediately post treatment.
There was no benefit adding TENS to other treatments (infrared, hotpack/exercise, collar/exercise/analgesic, and standard physiotherapy of ice/home exercise/advice) [90, 101, 108, 109] for various disorder types and various follow-up periods in very small trials. There was no difference when TENS was compared to manual therapy (2 RCTs, 107 participants) [109, 110] or ultrasound (1 RCT, 14 participants) [89] for reducing subacute/chronic neck pain immediately post treatment. Also, when different parameters of TENS were compared to each other the results were similar for pain at short term follow-up (1 RCT, 40 participants) [111].
CONFLICTING EVIDENCE
Laser
830nm or 904nm for myofascial pain had varied evidence (5 RCTs, Ceccherelli 1989, Gur 2004, Seidel 2002, Thorsen 1991, Thorsen 1992) [87, 105, 112-114] with meta-regression (2 RCTs, 81 participants, Ceccherelli 1989 and Gur 2004) [87, 113] suggesting drive technology (super-pulse) may be most successful in treating this subgroup albeit an independent clinical trial is needed to demonstrate this. We have also recorded trials with conflicting/unclear evidence in Table 3.
ADVERSE EVENTS
We found minor, transient, and reversible side effects consisting of increased pain, headache, tiredness or nausea to be occasionally present when reported for physical modalities. Most trials did not report adverse events at all or if so, collection of data was not described adequately.
DISCUSSION
Although the evidence continues to improve with respect to the use or not of physical modalities as a treatment choice for management of neck pain, there is still a lack of strong evidence to base recommendations that address meaningful outcomes in a standardized way. The core recommendations based on moderate evidence may be strengthened or refuted by results from larger trials with sound methodological quality. These recommendations supporting the use of acupuncture, laser and intermittent traction but not pulsed ultrasound, hot packs and continuous traction are summarized in Table 5.
Some modalities especially acupuncture and laser, utilize a broad spectrum of doses that may be beneficial while others appear to be of no benefit for pain management. Specific dosage trials are essential. Data on function/disability and quality of life is limited or completely absent. Many studies focus on pain as the primary outcome and to a lesser extent function typically using differing outcomes. Unless there is consistent use of the same pain and disability outcomes in these clinical trials it will be difficult to undertake meta-analyses and provide clinicians with a summary estimate of the expected benefit when considering these two outcomes. Further, since physical agents can be used for a variety of adjunctive benefits such as enhancing tissue extensibility to improve motion gains during mobilizations or exercise; or general healing effects then short term pain measures may not capture their benefit.
A number of reporting and design issues are consistent across neck clinical trials and have been detailed in Goldsmith et al. 2011 [115]. However, there are design options and clear criteria that can be used to improve the feasibility and quality of future clinical trials in this area of neck pain but also in rehabilitation generally. In particular, future research should ensure adherence to reporting standards of CONSORT [116, 117] and PRISMA guidelines, and should look beyond the basic two group design commonly used in clinical trials as well as consistent use of similar impairment and disability outcomes. Since rehabilitation often includes multiple interventions, it is recommended that researchers use factorial design methods to not only evaluate the effectiveness of independent treatments but also the impact on various combinations within the same trial. A core set of patient reported outcomes and key participation indicators (such as return to work) are needed and the community at large should consider setting initiatives, similar to the International Classification of Functioning (ICF) core measures [118]. Additionally, most studies in this overview assessed the outcome immediately following treatment up to six months. There is a need for more long-term follow-up.
There is general agreement between reviews. Some of the primary studies in one review may differ from another due to inclusion/exclusion criteria or search strategies.
Consistent reporting of side effects and how this information was collected is poor in the majority of trials. Accurate prospective collection of adverse event data is fundamental to these trials; there has been work done to define categories of severity and types of events considered adverse within the musculoskeletal area [119-121]. A move toward more active methods of capturing harms (rather than spontaneous reporting) would be necessary. Although our search did not retrieve any reviews of harms for physical modalities specific to neck pain, we can look to reviews pertaining to other musculoskeletal conditions or the general use of some physical modalities such as acupuncture. A review on the safety of acupuncture was reported by Wheway et al. [122] after analyzing the National Reporting and Learning Database of the National Patient Safety Agency in the United Kingdom. The authors reported the following adverse events related to 325 patient incidents: retained needles (31%), dizziness (30%), loss of consciousness/unresponsive (19%), falls (4%), bruising or soreness at needle site (2%), Pneumothorax (1%) and other adverse reactions (12%). More than 95% of the incidents were categorized as low or no harm. Other reviews have reported more serious adverse events related to acupuncture [123] however these findings should be questioned due to the use of unclear and unsystematic review methods that may have produced biased results. As it is well known that acupuncture treatment can be similar in technique regardless of the condition treated, it is conceivable that the aforementioned adverse events could manifest in patients with neck pain.
In a systematic review of conservative treatments for lumbar disc herniation, traction was related to 16 adverse events ranging from increased pain, anxiety, and fainting to lower limb weakness [124]. As there are many differences in the application of traction to the neck and low back, these specific results may not be directly relevant. While these adverse events appear to be minor and transient, they are perhaps an indication of the susceptibility of the spine when forces are applied in less specific and less controlled ways i.e. external machines, than with the sensitivity afforded by manual techniques. A physical modality such as hot packs for example, lacks strong evidence of benefit but harm is minimal and may still be considered since they are cost effective, easy to apply in a self-management program and may provide an element of comfort to the patient. Even though supportive evidence is lacking, it is only one component of evidence-based practice to be considered in the development of an individual treatment plan but decision making also requires the therapist’s clinical experience and the patient’s wishes [125].
We had several strengths regarding our approach to summarizing this literature. We used a comprehensive, librarian-assisted search and multiple databases. Two independent reviewers determined article relevance, assessed the AMSTAR methodological and verified data extraction. Consensus was used both by the internal data abstraction team and an interdisciplinary external panel consensus to validate the GRADE of evidence and recommendations.
CONCLUSION
Final Evidence-Based Recommendations (Table 4)
For chronic mechanical neck disorders, the recommendation from moderate evidence suggests using acupuncture or intermittent traction for short term pain reduction. In addition, this evidence suggests using LASER 830nm and 904nm for pain reduction, improving function/quality of life and to maximize global perceived effect up to the intermediate term (approximately six months). For both acute WAD and subacute/chronic neck disorders (including myofascial pain), the evidence suggests there is no benefit using pulsed ultrasound for reducing pain, improving function or global perceived effect immediately following treatment. Thermal agents (hot pack and infrared light) for chronic neck pain immediately following treatment or in the short term are also not suggested. Lastly, the evidence suggests there is no benefit in continuous traction for acute to chronic neck disorders for short term pain relief and improved function. Some electrotherapies (magnetic necklace, galvanic current) may not be beneficial for chronic neck pain. Dosage, design and long term follow-up continue to be the recommendations and essential elements when designing future trials.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
This work was supported by Canadian Institutes of Health Research (CIHR) grant(s) FRN: KRS-102084 and Centric Health LifeMark Industry Partner Grant.
APPENDIX 1
Excluded Studies Categorized by Reason for Exclusion
Design
Tsakitzidis G, Remmen R, Peremans L, Van Royen P, Duchesnes C, Paulus D, et al. Non-specific neck pain: diagnosis and treatment. Good Clinical Practice (GCP). Brussels: Belgian Health Care Knowledge Centre (KCE) 2009; Report No.: KCE Reports 119C.
Low AMSTAR rating
Brønfort G, Haas M, Evans R, Leininger B, Triano J. Effectiveness of manual therapies: The UK evidence report. Chiropractic and Osteopathy 2010; 18: 3.
Hurwitz EL, Carragee EJ, van der Velde G, Carroll LJ, Nordin M, Guzman J etal. Treatment of neck pain; noninvasive interventions: results of the Bone and Joint Decade 2000-2010 task force on neck pain and its assoiciated disorders. Spine 2008; 33(4 Suppl); S123-S152.
Fernandez-de-Las PC, Alonso-Blanco C, Cuadrado ML, Pareja JA. Spinal Manipulative Therapy in the Management of Cervicogenic Headache. Headache 2005; 45: 1260-70.
Teasell RW, McClure JA, Walton D, Pretty J, Salter K, etal. A research synthesis of therapeutic interventions for whiplash-associated disorders (WAD): Part 2-Interventions for WAD. Pain Res Manage 2010; 15(5): 295-304.
Vernon H, Schneider M. Chiropractic management of myofascial trigger points and myofascial pain syndrome: A systematic review of the literature [review] J Manipulative Physiol Ther 2009; 32(1): 14-24.
Excluded for Acupuncture
Intervention
Conlin A, Bhogal S, Sequeira A, Teasell R. Treatment of whiplash-associated disorders-Part 1: Non-invasive interventions. Pain Res Manage 2005; 10(1): 21-32.
Haines T, Gross A, Burnie SJ, Goldsmith CH, Perry L. Patient education for neck pain with or without radiculopathy. [Review] [123 refs][Update of Cochrane Database Syst Rev 2008; (4): CD005106; PMID: 18843681]. Cochrane Database Syst Rev 2009; (1): CD005106.
Miller J, Gross A, D’Sylva J, Burnie SJ, et al. Manual therapy and exercise for neck pain: A systematic review Man Ther 2010; 15: 334-54.
Wang M-Y, Tsai P-S, Lee P-H, Chang W-Y, Yang C-M. Systematic review and meta-analysis of the efficacy of tuina for cervical spondylosis. J Clin Nurs 2008; 17: 2531-8.
Low AMSTAR Rating
Baxter GD, Bleakley C, McDonough S. Clinical effectiveness of laser acupuncture: A systematic review. JAMS J Acupunct Meridian Stud 2008; 1(2): 65-82.
Brønfort G, Haas M, Evans R, Leininger B, Triano J. Effectiveness of manual therapies: The UK evidence report. Chiropr Osteopat 2010; 18: 3.
Hurwitz EL, Carragee EJ, van der Velde G, et al. Treatment of neck pain; noninvasive interventions: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Assoiciated Disorders. Spine 2008; 33(4 Suppl); S123-S152.
Lee MS, Choi T-Y, Kim J-I, Choi S-M. Using Guasha to treat musculoskeletal pain: A systematic review of controlled clinical trials. Chinese Med 2010; 5: 5.
Lin H-L, Song H-M, Zhong W-H, Chen S-Q, Wang S-Z. Effects of different acupuncture and moxibustion treatments on cervical spondylotic radiculopathy: A systematic evaluation. [Chinese]. J Clin Rehab Tissue Eng Res 2009; 13(46): 9017-21.
Reid SA, Rivett DA. Manual therapy treatment of cervicogenic dizziness: A systematic review. Manual Ther 2005: 4-13.
Vernon H, Humphreys BK. Manual therapy for neck pain: an overview of randomized clinical trials and systematic reviews. [Review] [141 refs]. Europa Medicophysica 2007; 43(1): 91-118.
Vernon H, Schneider M. Chiropractic management of myofascial trigger points and myofascial pain syndrome: A systematic review of the literature [Review] J Manipulative Physiol Ther 2009; 32(1): 14-24.
Design
Ernst E, Lee MS, Choi TY. Acupuncture: does it alleviate pain and are there serious risks? A review of reviews. Pain 2011; 152(4): 755-64.
Itoh K, Kitakoji H. Acupuncture for chronic pain in Japan: A review. Evidence-based Complementary and Alternative Medicine 2007; 4(4): 431-8. [neck studies included were non-RCTs]
Tsakitzidis G, Remmen R, Peremans L, Van Royen P, Duchesnes C, Paulus D, et al. Non-specific neck pain: diagnosis and treatment. Good Clinical Practice (GCP). Brussels: Belgian Health Care Knowledge Centre (KCE) 2009; Report No.: KCE Reports 119C.
Wang YW, Fu WB, Ou, AH, Fan L, Huang YF. A systematic review of randomized controlled clinical trials of abdominal acupuncture treatment of cervical spondylosis [Chinese] 2011; 36: 137-44. [abstract only]
Exclude for Thermal
Intervention (Multimodal, Thermal Agent Part of Cluster Treatment – Dosage and/or Contribution of Each Unclear)
Brønfort G, Nilsson N, Haas M, Evans RL, Goldsmith CH, Assendelft WJJ, Bouter LM. Non-invasive physical treatments for chronic/recurrent headache. Cochrane Database Syst Rev 2004; 3: CD001878.
Haraldsson BG, Gross AR, Myers CD, Ezzo JM, Morien A, Goldsmith C, et al. Massage for mechanical neck disorders. [Review] [114 refs]. Cochrane Database Syst Rev 2006; 3: CD004871.
Kay TM, Gross A, Goldsmith CH, Hoving JL, Bronfort G. Exercises for mechanical neck disorders. Cochrane Database Syst Rev 2009; (4).
Miller J, Gross A, D’Sylva J, Burnie SJ, et al. Manual therapy and exercise for neck pain: A systematic review Man Ther 2010; 15: 334-54.
Verhagen AP, Scholten-Peeters GGGM, van Wijngaarden S, de Bie R, Bierma-Zeinstra SMA. Conservative treatments for whiplash. Cochrane Database of Systematic Reviews 2007; 2: CD003338.
Vernon H, Humphreys K, Hagino C. Chronic mechanical neck pain in adults treated by manual therapy: a systematic review of change scores in randomized controlled trials. J Manipulative Physiol Ther 2007; 30: 215-27.
Comparison (Thermal Agent was Active Control or Co-Intervention)
Conlin A, Bhogal S, Sequeira A, Teasell R. Treatment of whiplash-associated disorders-Part 1: Non-invasive interventions. Pain Res Manage 2005; 10(1): 21-32.
Haines T, Gross A, Burnie SJ, Goldsmith CH, Perry L. Patient education for neck pain with or without radiculopathy. [Review] [Update of Cochrane Database Syst Rev 2008; (4): CD005106; PMID: 18843681]. Cochrane Database Syst Rev 2009; (1): CD005106.
Trinh K, Graham N, Gross A, et al. Acupuncture for neck disorders. Spine 2007; 32(2): 236-43.
Design
Tsakitzidis G, Remmen R, Peremans L, et al. Non-specific neck pain: diagnosis and treatment. Good Clinical Practice (GCP). Brussels: Belgian Health Care Knowledge Centre (KCE); 2009. Report No.: KCE Reports 119C.
Whiffen P. Evidence-based pain management and palliative care in Issue 3 for 2006 of the Cochrane Library. J Pain Palliat Care Pharmacother 2007; 21(1): 53-6.
Low AMSTAR Rating
Hurwitz EL, Carragee EJ, van der Velde G, et al. Treatment of neck pain; noninvasive interventions: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Assoiciated Disorders. Spine 2008; 33(4 Suppl); S123-S152.
Peake N, Harte A. The effectiveness of cervical traction. Phys Ther Rev 2005; 10: 217-29.
Teasell RW, McClure JA, Walton D, Pretty J, Salter K, etaL A research synthesis of therapeutic interventions for whiplash-associated disorders (WAD): Part 3-Interventions for WAD. Pain Res Manage 2010; 15(5): 305-12.
Vernon HT, Humphreys BK, Hagino CA. A systematic review of conservative treatments for acute neck pain not due to whiplash. J Manipulative Physiol Ther 2005; 28(6): 443-8.
Vernon H, Humphreys BK, Hagino C. The outcome of control groups in clinical trials of conservative treatments for chronic mechanical neck pain: A systematic review. BMC Musculoskeletal Disorders 2006; 7: 58.
Vernon H, Schneider M. Chiropractic management of myofascial trigger points and myofascial pain syndrome: A systematic review of the literature [Review] J Manipulative Physiol Ther 2009; 32(1): 14-24.
Exclude for Traction
Intervention (Manual Traction)
Gross A, Miller J, D'Sylva J, Burnie SJ, et al. Manipulation or mobilisation for neck pain. [Review] [173 refs][Update of Cochrane Database Syst Rev 2004; (1): CD004249; PMID: 14974063]. Cochrane Database Syst Rev 2010; (1): CD004249.
Kay TM, Gross A, Goldsmith CH, Hoving JL, Bronfort G. Exercises for mechanical neck disorders. Cochrane Database Syst Rev 2009; (4).
Kroeling P, Gross A, Goldsmith CH, Burnie SJ, Haines T, Graham N, et al. Electrotherapy for neck pain. [Review] [73 refs][Update of Cochrane Database Syst Rev 2005; (2): CD004251; PMID: 15846703]. Cochrane Database Syst Rev 2009; (4): CD004251.
Kroeling P, Gross A, Goldsmith CH, et al. Electrotherapy for neck pain. Cochrane Database Syst Rev 2012.
Miller J, Gross A, D’Sylva J, Burnie SJ, et al. Manual therapy and exercise for neck pain: A systematic review. Man Ther 2010; 15: 334-54.
Williams NH, Hendry M, Lewis R, Russell I, Westmoreland A, Wilkinson C. Psychological response in spinal manipulation (PRISM): a systematic review of psychological outcomes in randomised controlled trials. [Review] [50 refs]. Complement Ther Med 2007; 15(4): 271-83.
Low AMSTAR Rating
Hurwitz EL, Carragee EJ, van der Velde G, et al. Treatment of neck pain; noninvasive interventions: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Assoiciated Disorders. Spine 2008; 33(4 Suppl); S123-S152.
Peake N, Harte A. The effectiveness of cervical traction. Phys Ther Rev 2005; 10: 217-29.
Exclude for Electrotherapy
Intervention
Brønfort G, Nilsson N, Haas M, Evans RL, Goldsmith CH, Assendelft WJJ, Bouter LM. Non-invasive physical treatments for chronic/recurrent headache. Cochrane Database Syst Rev 2004; 3: CD001878. DOI: 10.1002/14651858.CD001878.pub2.
Haines T, Gross A, Burnie SJ, Goldsmith CH, Perry L. Patient education for neck pain with or without radiculopathy. [Review] [123 refs][Update of Cochrane Database Syst Rev 2008; (4): CD005106; PMID: 18843681]. Cochrane Database Syst Rev 2009; (1): CD005106.
Haraldsson BG, Gross AR, Myers CD, Ezzo JM, Morien A, Goldsmith C, et al. Massage for mechanical neck disorders. [Review] [114 refs]. Cochrane Database Syst Rev 2006; 3: CD004871.
Design
Tsakitzidis G, Remmen R, Peremans L, Van Royen P, Duchesnes C, Paulus D, et al. Non-specific neck pain: diagnosis and treatment. Good Clinical Practice (GCP). Brussels: Belgian Health Care Knowledge Centre (KCE) 2009; Report No.: KCE Reports 119C.
Low AMSTAR Rating
Hurwitz EL, Carragee EJ, van der Velde G, et al. Treatment of neck pain; noninvasive interventions: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Assoiciated Disorders. Spine 2008; 33(4 Suppl); S123-S152.
Lee MS, Choi T-Y, Kim J-I, Choi S-M. Using Guasha to treat musculoskeletal pain: A systematic review of controlled clinical trials. Chinese Medicine 2010; 5: 5.
Teasell RW, McClure JA, Walton D, et al. A research synthesis of therapeutic interventions for whiplash-associated disorders (WAD): Part 2-Interventions for WAD. Pain Res Manage 2010; 15(5): 295-304.
Vernon HT, Humphreys BK, Hagino CA. A systematic review of conservative treatments for acute neck pain not due to whiplash. J Manipulative Physiol Ther 2005; 28(6): 443-8.
Vernon H, Humphreys BK. Manual therapy for neck pain: an overview of randomized clinical trials and systematic reviews. [Review] [141 refs]. Europa Medicophysica 2007 Mar; 43(1): 91-118.
Vernon H, Schneider M. Chiropractic management of myofascial trigger points and myofascial pain syndrome: A systematic review of the literature [review]. J Manipulative Physiol Ther 2009; 32(1): 14-24.
Wang S-Z, Lin H-L, Song H-M, et al. Conservative in the treatment of protrusion of cervical vertebra intervertebral disc: A systematic review. [Chinese]. J Evid Based Med 2009; 9(3): 331-6.


