All published articles of this journal are available on ScienceDirect.
A Complication During Femoral Broaching in Total Hip Arthroplasty: A Case Report
Abstract
Press-fit component fixation is one of the primary goals in uncemented total hip arthroplasty. When aiming at proximal load transfer, the stem size has to be selected with regard to the shape of the proximal femoral canal. This can be challenging in patients with ‘champagne flute’ femurs with a relatively narrow diaphysis, especially when a long stem femoral component is used. The present case report describes a complication during femoral broaching for a primary uncemented femoral component. Because of the narrow diaphysis, the distal portion of the broach got caught in the narrow canal and it became impossible to remove the broach with conventional techniques. Via a second distal incision, the femur was split from the distal tip of the broach to approximately 5 cm distal of the femoral neck cut along the posterior aspects of the femur. This loosened the broach enough to allow for an uncomplicated removal. The longitudinal split was secured with cables before a similar size primary implant was press fitted into the femoral canal.
INTRODUCTION
The goal of femoral component positioning in uncemented total hip arthroplasty (THA) is the accurate restoration of joint biomechanics and a close fit between the implant and the endosteal surface of the proximal femur [1, 2]. Primary mechanical stability is achieved by press-fit implantation [3] which allows for bony ingrowth onto the prosthesis [4, 5] and for proximal load transfer [1, 6]. A close proximal fit is furthermore essential to minimize micromotion at the bone-implant interface [1, 6], and to reduce the risk of stress-shielding [7] and aseptic loosening [8].
Careful stepwise preparation of the proximal femur is crucial to achieve primary component stability. Surgical broaches, gradually increasing in size, are used to prepare a predefined space for the implant. In this case report, we describe a rare complication of broaching and how it can be managed intraoperatively.
CASE REPORT
A 60 year old male was scheduled for THA for left primary end-stage hip osteoarthritis (OA). (Fig. 1) In the operating room, a spinal-epidural anesthesia was administered. After positioning for posterior-approach THA, an 8 cm incision was placed over the left hip. The short external rotators were indentified, released and tagged with stitches. Elevation of the gluteus minimus exposed the capsule which was subsequently incised and tagged. The hip was dislocated, the neck cut and the femoral head removed. The acetabulum was prepared in the usual fashion and a size #58 no-hole shell (R3, smith&nephew, Memphis, TN) was press-fitted.

Left: Anteroposterior radiograph of the left hip showing primary OA and a ‘champagne flute’ femoral canal. Right: Lateral radiograph of the left hip demonstrating a thick anterior cortex (white arrows).
To start the preparation of the proximal femoral canal, a box osteotome was used to open the canal. After reaming for a size #14 stem (Synergy, smith&nephew, Memphis, TN), the femur was broached for a size #14 stem. Trial reduction with a standard offset neck and a plus eight head showed restoration of the lesser trochanter-to-center distance (LTC) and the femoral offset.
After trial reduction, an attempt to remove the broach failed, and despite using a heavy mallet and ultimately a removal slap hammer it was not possible to remove the broach. After trying to remove the broach for 30 minutes, flexible osteotoms were utilized to carefully loosen up the proximal part. After one and half hours of repeated extraction attempts, we decided to stop.
Considering the configuration of the proximal femoral canal, it was assumed that the broach got hung up distally. Therefore, the decision for a second incision was made to release the broach distally. The exact length of a #14 broach was measured and an 8 cm skin incision was placed proximal to the distal tip of the implant. After dissection of the vastus lateralis, a drill was placed on the posterior aspect of the femur distal to the broach tip which was confirmed by an intraoperative radiograph (Fig. 2).
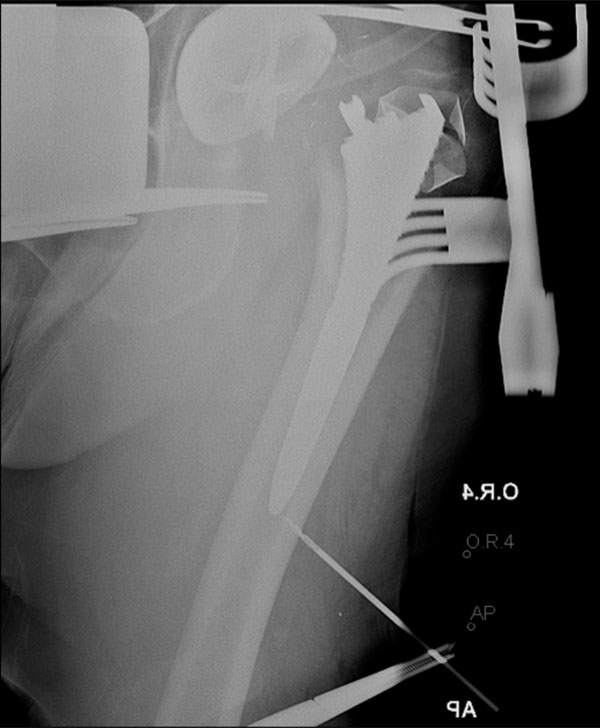
Anteroposterior radiograph of the left hip taken intraoperatively showing the size #14 broach stuck in the femoral canal. The distal drill confirmed the accurate position of the second incision.
Midway between the neck cut and the distal tip, a second posterior drill hole was placed, leaving 5-6 cm of bone proximally. Using an oscillating saw, the two drill holes were connected. After completing the posterior femoral split, the broach could now easily be extract.
Hereafter, a total of 6 Dall-Miles cables (Stryker, Mahwah, NJ) were applied: one just proximal and distal to the lesser trochanter (LT); two along the osteotomy line; and one at the tip of the implant and one distal. The cable wires were tightened and after over reaming the distal canal the same broach was re-inserted. Trial reduction showed restoration of the lesser trochanter to center distance and the femoral offset.
At this time, the broach could be smoothly removed and a size #14 stem was impacted achieving excellent press-fit. A +8, #36 head (Oxinium, smith&nephew, Memphis, TN) was added and the hip was reduced.
The patient was instructed partial weight bearing 20% for 4 weeks, before weight bearing as tolerated was initiated.
At the 6-week and 12-week routine follow-up appointments, the femoral implant was found to be stable with no focal lucencies (Fig. 3).

Anteroposterior radiograph of the pelvis at 12 weeks postoperatively, showing left uncemented total hip arthroplasty with Dall-Miles cables. The implant is stable and there are no radiolucencies.
DISCUSSION
The medullary canal shape of the proximal femur is highly variable [9-11]. Dorr et al identified three patterns of shape: type A present with a thick cortex and a narrow diaphyseal canal which is commonly present in younger males (champagne flute [12]); type B is most common and shows normal thickness of the cortex; and type C has a wide intramedullary canal with a thin cortex which is associated with older women (stove pipe [12, 13]).
The proximal femur of our patient can be classified as Dorr type A with thick cortices on the anteroposterior (AP) radiograph. As originally described by Dorr, one can clearly appreciate the medial and lateral cortices on the AP radiograph that begin just at the distal end of the LT and quickly increase in thickness (Fig. 1).
A tight anatomic fit between the stem and the endosteal surface is a key success factor in uncemented THA. When aiming at proximal load transfer with an uncemented femoral component, the stem size has to be selected with regard to the shape of the proximal femoral canal [1, 6]. In the authors’ experience, this can be challenging to achieve, especially in patients with ‘champagne flute’ femors, and when straight and relatively long stem systems are used. Consequently, proximal loading is not always entirely achievable with these designs, and fixation is more likely to occur in the meta-diaphyseal region [14].
Straight uncemented stems have been successfully introduced more than two decades ago with excellent survivorships [15]. However, the authors are not aware of any report in literature describing the management of a complication during canal broaching for long straight stems. Hirschmann et al reported on a case of an uncemented rectangular-shaped trail stem that engaged with the canal and it became impossible to remove it. The trial stem was ultimately left in situ for 17 years and underwent revision surgery because of aseptic loosening. The authors highlight the importance of initial press-fit femoral implantation and suggest that the chemistry and structure of the stem surface might be of minor importance [16].
The current case report describes a strategy to loosen the broach when the distal part engages with the narrow canal and it becomes impossible to remove it with conventional techniques. If such a complication occurs, a split incision along the components’ distal part disengages the distal press-fit. It appears that such a split incision reduces the press fit between the bone and round distal portion of the broach. The technique of split incisions has also previously been described as an option for the removal of well-fixed femoral components in revision surgery [17]. Due to posterior-approach THA in the present case report, the split incision was performed on the posterior femur. Because of the round distal design of the utilized stem, the location of the split incision is probably secondary and can be adjusted according to the surgical approach. Only if a split incision is unsuccessful, we would proceed placing a tapered window on the femur. The reported management of such an unfortunate complication is safe for the patient and seems not to impair the outcome.
The present case highlights the importance of pre-operative templating and the necessity of considering individual anatomic variations when selecting the proper femoral prosthesis. Overreaming should be considered in Dorr type A femors to avoid distal fixation.
CONFLICT OF INTEREST
Each author certifies that he has no conflict of interest in connection with the submitted article.
ACKNOWLEDGEMENTS
Declared none.


