All published articles of this journal are available on ScienceDirect.
Does Choice of Head Size and Neck Geometry Affect Stem Migration in Modular Large-Diameter Metal-on-Metal Total Hip Arthroplasty? A Preliminary Analysis
Abstract
Due to their theoretical advantages, hip systems combining modular necks and large diameter femoral heads have gradually gained popularity. However, among others, concerns regarding changes in the load transfer patterns were raised. Recent stress analyses have indeed shown that the use of modular necks and big femoral heads causes significant changes in the strain distribution along the femur. Our original hypothesis was that these changes may affect early distal migration of a modular stem. We examined the effect of head diameter and neck geometry on migration at two years of follow-up in a case series of 116 patients (125 hips), who have undergone primary Metal-on-Metal total hip arthroplasty with the modular grit-blasted Profemur®E stem combined with large-diameter heads (>36 mm). We found that choice of neck geometry and head diameter has no effect on stem migration. A multivariate regression analysis including the potential confounding variables of the body mass index, bone quality, canal fill and stem positioning revealed only a negative correlation between subsidence and canal fill in midstem area. Statistical analysis, despite its limitations, did not confirm our hypothesis that choice of neck geometry and/or head diameter affects early distal migration of a modular stem. However, the importance of correct stem sizing was revealed.
INTRODUCTION
Modern total hip arthroplasty (THA) designs incorporating modular necks and second-generation large-diameter Metal-on-Metal (MoM) articulations have been widely implanted worldwide. Due to the increased joint stability and the low-wear characteristics of the well-functioning arthroplasties, an extended long-term survivorship rate was anticipated. Thus, they were reserved for the younger and more active patients [1]. However, in predicting longevity, periprosthetic bone remodeling after prosthesis insertion is the most important factor. We know that adaptive bone remodeling is proportional to the magnitude of stress [2]. It is logical to presume that a deviated femoral head, at the coronal or sagittal plane, under an axial load may have different load transfer patterns than when a straight neck is used [3]. Similarly the use of large-diameter heads may impose alterations in strain distribution when compared to 28 mm heads.
Only a few papers in recent literature have dealt with the effects of neck modularity and head size on the biomechanics of the hip [3-6]. According to these stress analyses, the use of modular necks and big femoral heads alters significantly the strains developed along profile lines across the femur and particularly around the stem tip. For the retroverted necks particularly, it seems that the implantation in the anteriorly bowed femur creates increased bending stress and therefore a not so benign scenario for the biomechanical environment [3, 4, 7]. Furthermore, a finite element analysis (FEA) has shown that for a lateral profile line, along linea aspera and for the stem tip area increasing the head diameter results in strain rise [5]. Although it remains uncertain whether these changes in strain distribution patterns are clinically relevant, they raise concerns regarding adaptive hypertrophy and possible mechanical failure due to increased stress [3]. Mechanical failure and loosening of a femoral stem can be predicted accurately by early measurement of distal migration at two years follow-up [8]. The RSA migration pattern of some cemented stem designs has indeed already been found to be affected by the version of the femoral component [7, 9]. Questions are raised over the effect of neck modularity on subsidence of uncemented stems.
On this basis, we examined early stem migration in a case series of 116 patients (125 hips), who have undergone primary cementless MoM THA with modular necks and large-diameter heads and asked whether: a) the choice of a particular neck orientation resulted in increased migration and b) increasing head size led to an increase in subsidence.
MATERIALS AND METHODS
Between January 2006 and January 2008, a consecutive series of 138 primary cementless MoM THA in 129 patients was performed in our institution. The selection criteria were an absence of severe deformity of the femoral canal and adequate bone stock for cementless fixation [10]. Exclusion criteria were renal insufficiency and female gender in reproductive age [11]. All patients gave informed consent to participate in the study, and the study was approved by our university institutional review board.
A collarless, streamlined, tapered modular stem (Profemur® E stem, Wright Medical Technology Inc., Arlington, TN) made of Ti6Al4V alloy was used in all patients. The stems have a grit-blasted surface (Ra = 6 micron) and a rectangular cross-section for enhanced rotational stability [12]. They are available in 10 different sizes (Fig. 1). The Profemur® E stems utilize a patented modular neck technology. Eleven options of neck orientation are available from five different designs (Fig. 2). These five neck versions include a neutral neck, an 8° angled neck for varus or valgus, an 8° angled neck for anteversion or retroversion, a 15° angled neck for anteversion or retroversion, and a neck with a combination of 4° for varus and 6° for anteversion. The latter double-angled neck can provide varus-anteversion, valgus-retroversion, varus-retroversion and valgus-anteversion orientation, depending on the side implanted (Fig. 3). Each of them can be in short or long configurations, so the available options are 22. The Conserve® (Wright Medical Technology Inc., Arlington, TN) CoCr cup, without metal liners and holes or screws, was used as acetabular component in all cases.

The Profemur® E stem. Note the grit-blasted surface, the proximal ribs and at the lateral view the tapered, rectangular cross-section. The latter two features provide improved initial rotational stability.

The available neck types, each coupled with the plastic blue trial. In the first row, from left to right: the straight neck, the 8° angled neck for anteversion or retroversion (Ante/Retro 8°) and the similarly 15° angled neck (Ante/Retro 15°). In the second row, the 8° varus or valgus neck is shown first. The next two are actually the same neck version, designed separately for the right (ARVV1) and the left hip (ARVV2), so as to provide the combination of 4° varus and 6° anteversion in each side.
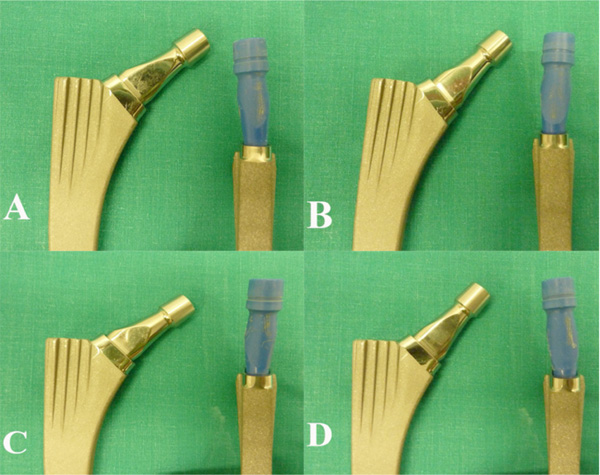
The double-angled necks can provide further orientations depending on the side implanted. For the right hip, the ARVV1 neck can provide 4° of varus and 6° of anteversion (Ante-varus) (A), but also 4° of valgus and 6° of retroversion (Retro-valgus) if implanted reversed (B). If the ARVV2 neck is used instead, the possible orientations are 4° of varus and 6° of retroversion (Retro-varus) (C) and 4° of valgus and 6° of anteversion (Ante-valgus) (D). The same applies vice versa for the left hip.
Patients who fulfilled the selection criteria underwent a complete metabolic workup before operation and a cardiologic and pneumonologic evaluation, when necessary. Preoperative control included digital radiographic examination, with low-centered pelvic radiographs and anteroposterior and lateral radiographs of the indexed hip. The procedures were performed by a single surgeon, the senior author, in a single unit and with the abovementioned specific implants and MoM articulation. A standard posterior surgical approach was used in all cases. Implant type, size, neck, and head were selected according to preoperative planning and intraoperative axial and rotational stability and impingement testing. These implants were accurately recorded. A closed suction drainage was used in all cases. Postoperatively, antibiotic prophylaxis (cephalosporin) was used for two days until the removal of the drainage. Routine prophylaxis was not provided for the prevention of heterotopic ossification. Low-molecular-weight heparin was administered for six weeks together with compression stockings. Partial weight-bearing was encouraged for six weeks and progressed to full weight-bearing as tolerated thereafter.
All patients completed at least two years of follow-up (mean 38 months, range 26-64 months). Reevaluation was performed at regular intervals (1st, 3rd, 6th month and every year thereafter) and included clinical assessment and digital radiography of the operated hips. During this follow-up period, three patients (three hips) died for reasons irrelevant to the operations, nine patients (nine hips) were lost to follow-up, and one had a stem revision because of aseptic loosening, which was attributed to failure of primary fixation of the undersized stem. These left 116 patients (125 hips) available for analysis. 43 (37%) of them were men and 73 (63%) women. Mean average age at surgery was 63.7 years (range 29 - 85 years). The preoperative diagnosis for the 125 hips was primarily osteoarthritis (93 hips; 74.4%). Other etiologies included femoral neck fracture (8 hips; 6.4%), avascular necrosis (5 hips; 4%), osteoarthritis secondary to developmental dysplasia of the hip - Crowe type I (6 hips; 4.8%) and II (3 hips; 2.4%) - or Legg-Calve-Perthes disease (6 hips; 4.8%), rheumatoid arthritis (2 hips; 1.6%) and traumatic osteoarthrosis (2 hips; 1.6%). From the neck options available every possible orientation was used, except from valgus-anteversion (Table 1). Head size, with 2 mm increments, varied from 40 mm to 52 mm (mean 44 mm) (Table 2).
Groups of Cases According to Neck Type and Differences in Mean Stem Migration Across them
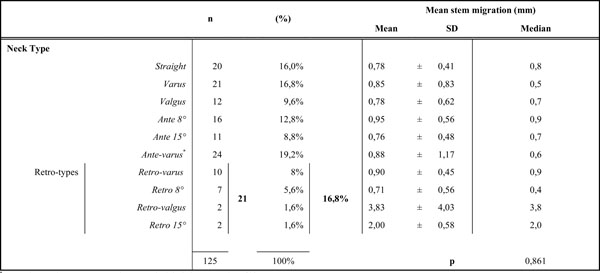 |
* Ante-valgus neck type was not used, SD: standard deviation, n: number of hips.
p refer to the p-value of Kruskal-Wallis test of differences between the first 8 groups of neck type (non-parametric equivalent test to ANOVA).
Descriptive Data for Head Size, BMI, Canal Fill Levels, Early Migration and their Association
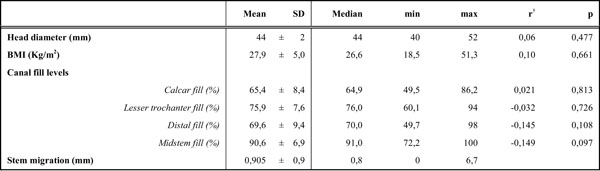 |
†Pearson correlation coefficient of the association betweeen mean stem migration and all other variables, BMI: Body Mass Index, SD: standard deviation.
According to the orientation of the implanted neck, the cases were divided into 10 groups (Table 1). The first postoperative and subsequent consecutive anteroposterior digital radiographs of each hip were examined retrospectively by two independent blinded observers (E.T, C.P.), neither involved in the clinical care of the patients. Stem subsidence at two years postoperatively was measured by the two observers, as a change in the vertical distance from the proximal tip of the greater trochanter to the shoulder of the stem [8]. A computer-assisted method was used to perform these measurements. The radiographs were originally DICOM and transformed into TIFF greyscale format without compression. These digital images were processed via Roman v1.7 software (Roman software version V1.70; Robert Jones and Agnes Hunt Orthopaedic Hospital, Oswestry, UK; http://www.cookedbits.co.uk/roman/). Roman is a radiological measurement program designed for orthopaedic applications in general. Its accuracy has already been demonstrated for the measurement of polyethylene wear, where the determination of bone and prosthesis landmarks is automated by the computer using an edge detection algorithm [13]. Roman has also been successfully used in stem migration analyses [14].
Cortical Index (CI), stem alignment and canal fill were also assessed, with the use of Roman v1.7. CI was calculated at a level 100 mm below the middle of the lesser trochanter and Dorr’s bone quality for each patient was assigned [15]. Varus or valgus malalignment of the stem was defined as deviation from the longitudinal femoral axis of > 3° on the first postoperative radiograph [16]. On the same radiograph, canal fill at four different levels (calcar, lesser trochanter, midstem, distal fill) was measured [17]. Firstly, lesser trochanter level was defined from a line drawn on the anteroposterior radiograph through the midpoint of the lesser throchanter. Three lines parallel to this were then drawn through the diaphysis. One through the medial margin of the neck osteotomy (calcar level), another through the middle of the stem (midstem level) and the last 100 mm distally, at the stem tip area (distal level). Canal fill was calculated as a percentage of the stem diameter to the endosteal diameter at each level [17]. We defined a stem as undersized when midstem fill was ≤80% [18].
Statistical Analysis
As the determination of bone and prosthesis landmarks were assessed by hand, before proceeding to further analysis an investigation of the intra- and interobserver variability was performed to confirm the reliability of the results. Intraobserver variability was determined by estimating the correlation coefficient of two measurements obtained by one observer in 1-week intervals. Interobserver variability was determined by simultaneously estimating the correlation coefficient (r) and the F-test of equality of variances of the two measurements obtained by the two different observers. Interobserver reliability was assessed by using the intraclass correlation coefficient (ICC). We set 2.4 mm as the threshold of distal migration at 24 months follow-up [8].
Pearson correlation coefficients were used to assess the association of mean stem migration with head diameter, Body Mass Index (BMI) and canal fill levels, while mean differences of the early migration across the rest variables of interest were assessed using the Kruskal-Wallis non-parametric test (equivalent test to ANOVA) and the test of equality of medians.
A multivariate regression analysis was performed to examine whether neck type and head diameter independently affected early migration. In the model, only those variables were included, that in the separate univariate regression models were found to have a p-value of association with early migration lower than 0.150. Among the variables examined were BMI (continuously), Dorr’s bone quality (categorically), stem positioning (neutral, varus, valgus; categorically), canal fill in the four levels (continuously). Midstem fill was also introduced categorically (≤80% vs >80%).
All statistical analyses were performed using the Stata statistical package (Stata Corporation: Stata/SE 11.0 for Windows, Lakeway Drive, College Station, Texas, USA, 2010).
RESULTS
Intraobserver variability was negligible and the measurements of the two observers were highly correlated (Pearson r=0.970) with equal variances (p=0.641). The ICC was equal to 0.969 indicating very good agreement between the two observers, thus the mean migration value for each patient was used for further analysis. Mean distal migration at two years postoperatively was 0.905±0.9 mm (median 0.8 mm, range 0-6.7 mm). Four patients exhibited stem subsidence more than the 2.4 mm threshold. Distribution of migration in the groups is shown in Fig. (4a), where the retroverted necks are considered as one group (including retro 8° and 15°, retro-varus and retro-valgus). Boxplots of early subsidence in relation to the rest categorical variables are shown in Fig. (4b-d).
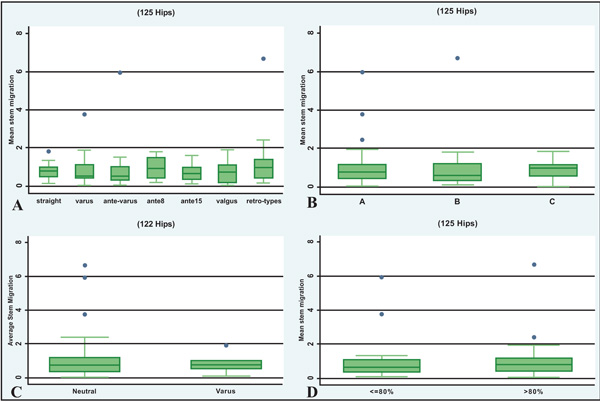
Boxplots showing the relationship between migration and the categorical variables of interest, i.e. neck type (A), bone quality (Dorr’s A, B, C bone quality) (B), stem positioning (neutral vs varus) (C) and midstem fill (<80% vs >80%) (D).
Table 2 presents the Pearson correlation coefficient of the association of mean early migration with head size, BMI and canal fill levels. Head size and BMI doesn’t seem to correlate with subsidence. There appeared to be a negative association of mean migration with midstem and distal levels, although marginally non-significant (Table 2).
Mean differences in early migration across categories of neck type and several variables under study are presented in Tables 1 and 3. There was no evidence of difference in early migration across choices of neck geometry. However, one patient with a retroverted 15° neck had a mean distal migration of 2.4 mm and another patient with a retro-valgus neck had a migration of 6.7 mm. Retroverted 15° and retro-valgus neck have only been used each twice (Table 1). Furthermore, when comparing the retroverted versus the straight necks, there was a suggestion of difference (mean migration=1.22 for retroverted necks versus 0.78 for straight neck type), although not statistically significant at the 5% significance level (p=0.176, t-test, data not shown).
Differences in Mean Stem Migration Across Categories of Important Variables Under Study
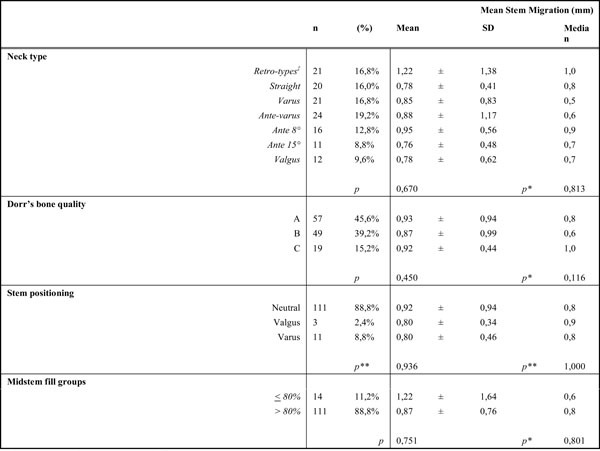 |
p refer to the p-value of Kruskal-Wallis test of differences between all groups (non-parametric equivalent test to ANOVA).
p* denote the p-value of equality of medians.
p** denote the p-values for Kruskal-Wallis and medians’ test respectively for comparing groups Neutral and Varus only (due to insufficient number of valgus stems for analysis).
‡Retro types include retro 8° and 15°, retro-varus and retro-valgus, SD: standard deviation.
Table 4 shows the mutually adjusted linear regression-derived coefficients of the association of stem migration with neck type and head diameter. Their interaction was not statistically significant (p=0.208). The only potential confounders that appeared to affect migration (untransformed) in the univariate models were midstem (β=-1.43, p=0.097) and distal fill (β=-1.90, p=0.108) and were therefore included in this model. Head size does not seem to play a role in stem’s early subsidence (β=0.02, p=0.459). Migration tended to be higher when retroverted neck types were used, compared to other neck types, although the association was statistically non-significant (β=0.38, p=0.077). In contrast with canal fill in stem tip area, midstem fill was found to be negatively associated with stem migration, with the difference found marginally significant (β=-0.36, p=0.046). However, no statistical significant difference is evident, when comparing undersized with the rest stems (Table 3).
Mutually Adjusted Linear Regression-Derived Coefficients for the Regression of Stem Migration on Neck Type and Head Diameter Controlling for Potentially Confounding Variables in an Analysis of 125 Hips
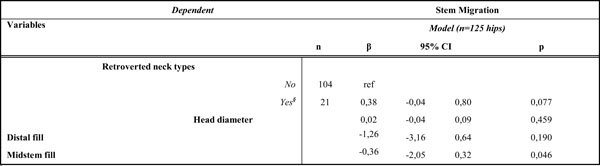 |
§Retro types include retroverted 8° and 15°, varus and valgus, 95% CI: 95% Confidence Interval, β: regression coefficient.
DISCUSSION
Although the risk and benefits of systems combining modular necks and large-diameter femoral heads are constantly reevaluated [19, 20], interestingly enough, biomechanics of these novel systems have not been equally investigated. Increased femoral anteversion alters significantly loading patterns in monoblock implants, while variations of offset seem to cause only minor changes [21]. For the modular-neck stems and their complex configurations, however, there are only a few reports in the literature [3, 4, 6]. In a study by Umeda et al. [3] strain gauge measurements of a modular cementless stem implanted in a synthetic femur were performed. Changing the neck from straight to anteverted or retroverted caused a large increase in strains on both, anterior and posterior, femoral surfaces, particularly at the distal part of the stem, and that increase was highly correlated with the extent of neck version. On the aspect toward which the prosthetic neck was oriented increased compressive strains were developed, while on the opposite side increased tensile strains. Due to the anteriorly bowed femur more bending stress was produced, especially at the stem tip area, when retroverted necks were used, as the femoral head deviates more in the sagittal plane than when an anteverted neck is used. The highest value of strain increase, compared with the strain developed with the straight neck, was 1195% and it was recorded with the extensively retro-angled 22.5° neck at the anterior aspect of the femur and at the level of the stem tip. It is worth noticing that, for both neck types, strain magnitudes on the anterior and posterior surfaces exceeded those developed on an intact femur [3]. Strains on the medial and lateral aspects of the femur were also increased, but at a lesser magnitude of maximum 22% [3]. Although it is difficult to directly compare results between experimental studies, this increase in the tensile strain on the anterior femoral surface with the retroverted necks was confirmed in another strain gauge study on cadaveric femurs [4]. In the same study, varus neck angulation was found to have a relatively small influence on strain distribution in the proximal femur [4]. In contrast with these studies, a FEA reported no significant alterations in the strain distribution of a cemented stem coupled to a modular neck, positioned in anteversion, retroversion and with two different offsets [6]. However, this study focused only on the medial and lateral femoral aspects. None of these papers examines the changes in strain pattern caused by simultaneous alteration of neck-shaft angle, neck length and version. On the other hand, only one study addresses the effect of increasing head size in proximal femur loading [5]. Although one anticipates that head diameter would not affect the strain pattern of the implant [4], this FEA revealed notable changes [5]. With respect to the reference model of a 28 mm femoral head, changing head diameter in 10 mm increments invoked proportional increases of about 15 to 18% in the maximum strains developed around the stem tip, and along linea aspera and a lateral profile line [5].
Whether these changes in loading patterns are associated with clinical problems remains uncertain. We know that bone remodeling after implantation is proportional to the magnitude of stress applied [2]. The increased strain induced by the increased offset and altered neck angles could theoretically act beneficially in preservation of proximal bone stock in vivo, minimizing proximal femur stress-shielding. However, as the postarthroplasty neck version becomes excessive, the anterior and posterior femoral regions are exposed to noticeably great stresses, with strain values exceeding several times, not only those developed with straight necks, but also those of unoperated femurs [3]. Although none of the existing papers [3 - 6] examines the scenario, we assume that a neck with reduced neck-shaft angle and increased length, implanted in retroversion and coupled with a big femoral head, would lead to even greater strain concentration. There is a concern that subsequent changes in bone quality, due to adaptive remodeling, may have undesirable long-term effects on the stability of the implant and, thus, may limit the life-span of THA [4]. Furthermore, these extended stresses at the implant-bone interface seem likely to raise the risk of implant loosening [21]. A latest report from the Australian Joint Registry has shown indeed a significant higher revision rate for modular-neck stems, with aseptic loosening identified as the predominant reason [22]. Similarly, higher revision rates due to loosening/lysis were recorded for large-diameter MoM THAs (>32 mm), compared to those with smaller bearings [22].
Loosening of a femoral stem, though, can be predicted by measurement of distal migration at two years follow-up [8]. Distal stem migration might be, therefore, affected by the parameters of head size, neck version and femoral offset. In a previous RSA study of cemented THA, it was already found that, for some stem designs, anteversion is negatively associated with subsidence [9]. In light of these, we measured early migration in a series of 125 uncemented modular-neck MoM THAs, focusing on the behavior of retroverted necks. A multivariate analysis, including several potential confounding variables, however, has shown that no specific neck geometry resulted in increased migration. Retroverted necks, in particular, have not presented significant differences in subsidence, when compared with straight necks. Similarly, increasing head diameter did not also seem to affect stem subsidence and this agrees with recent EBRA studies [20]. The results revealed only a negative association between migration and midstem fill, independent of the other covariates. This finding goes along with the intention of stem’s design for metaphyseal press-fit.
Our study has several limitations. First of all, the number of patients receiving a retroverted neck was limited. This was due to two reasons. Firstly, as these systems were reserved for the younger and more active patients, the overall number of patients enrolled was relative small for the neck options available. Secondly, it was inapplicable to randomise patients to the neck type, because this would have endangered joint stability. As posterior approach was used in all cases, it was fairly uncommon to use a retroverted neck to adjust femoral component version. Certain neck options (retroversion-valgus and retroversion 15°) were only used twice, thus safe conclusions could not be made from a separate analysis. For this reason we performed an initial univariate analysis excluding these cases (Table 1) and then grouped patients with a retroverted neck into a single group and proceeded to further steps. The most incriminated combination of strain rise, retroversion-varus, was examined in the univariate analysis. Limited number of patients was the reason for another premise. To avoid further subdividing of the sample, we intentionally ignored the variable of neck length; femoral offset was determined only by changes of the neck-shaft angle. Consequently, our preliminary results should be interpreted with caution; negative results may be related to the limitation of the series. Despite, however, the small sample size, the strength of this study lies in that it is a single-institution, single-surgeon study and that the same implants were used in all patients. Thus, migration could not be influenced by design or surgeon related factors.
In conclusion, in order to investigate the effect of neck modularity and head size on the outcome of cementless THA, we measured early distal stem migration in a case series with these implants combined. Although literature is unfavorable with retroverted necks, statistical analysis of our series, despite its limitations, failed to reveal an association of migration with retroverted or any other neck type whatsoever. Similarly, head diameter could not be related to subsidence in our series. The higher incidence of reported aseptic loosening of modular-neck stems and large-diameter MoM bearings is not confirmed in the preliminary analysis of our short-term follow-up series.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


