All published articles of this journal are available on ScienceDirect.
Occult Acetabular Fracture in Elderly Patients
Abstract
Acetabular fractures in the elderly are increasingly common; however, an antecedent of trauma may not be known, and the diagnosis easily missed. Early identification and prompt management are needed in order to minimise morbidity rates, but little has been published on occult acetabular fracture.
In this paper we present three cases of occult acetabular fracture in patients older than 75 years. All three are females and had previously been operated on the ipsilateral hip with an implant (two proximal femur fractures treated with a proximal intramedullary femoral nail, and one case of total joint replacement); these acetabular fractures could be related to the existence of a stress shielding mechanism.
We believe that whenever an elderly patient feels groin pain, and anteroposterior pelvis X-rays are normal, oblique Judet projections (obturator and iliac) should be obtained. In any case, displacement will make any fracture evident within a few weeks.
INTRODUCTION
Acetabular fractures in elderly patients are rare, but their incidence has increased [1-4] during the last 30 years [5] probably due to longer survival rates and higher activity levels [6]. As a result of osteoporosis, particularly in females, low energy trauma is the main cause of acetabular fractures in the elderly [7-9]. Furthermore, in some cases an antecedent of trauma is not known [10], making diagnosis easily missed [11]. Although early diagnosis is very important, since delayed management and early failures with subsequent salvage surgery can cause higher morbidity [4, 12], very few papers have been published on occult acetabular fractures [9-1, 13-15]. In this paper we present three cases of non-traumatic occult acetabular fractures in patients older than 75 years. Informed consent was obtained from all these patients, and the study was approved by our Hospital’s ethics committee.
CLINICAL CASES
Case 1.
A seventy-five-year-old female patient, operated on three years previously for a left hip fracture using a proximal femoral nail (PFN, Synthes), started to feel left groin pain with no traumatic antecedent; she was otherwise healthy. She was not using any drug interfering with bone metabolism. Clinical examination revealed that the pain was exacerbated by internal and external rotation of her hip. X-ray examination of the left hip revealed a consolidated hip fracture with lateral migration of the screw. There were no signs of acetabular fracture on this AP projection (Fig. 1).

A left hip anteroposterior x-ray in a 75-year-old female patient with groin pain. No acetabular abnormalities visible. Lateral migration of the hip screw nails.
Since the pain continued, two months later further x-rays were obtained, revealing a transverse acetabular fracture according to Letournel’s classification [16] with the femoral head medially protruding onto the anterior acetabular wall; probably because of this, the femoral head had an anteriorsuperior notch, and was collapsed (Fig. 2).

X-ray of the same patient two months later. The medially-migrated femoral head, with an acetabular transverse fracture, is evident.
A cemented total hip replacement was performed, with no osteosynthesis or bone graft of the acetabular fracture (Fig. 3); bone and soft tissue samples obtained intraopera-tively were negative for bacteriological cultures. The pathology biopsy presented no noteworthy findings, apart from acute inflammation cellularity. A chest X-ray revealed no sign of a former pulmonary tuberculosis. The patient improved clinically after the operation. Six year follow-up X-rays showed proximal migration and medialization of the acetabular component (Figs. 4, 5).

X-ray of the same patient at one year follow-up. Cemented hip replacement with proximal acetabular cup migration.

Five year follow-up.

Six year follow-up.
The pain eased and the patient continued to be clinically well at the 7 year follow-up. Although she walked with a slight limp and needed the help of a crutch, daily activities such as short-distance walking and climbing stairs were well tolerated. Painkillers were needed occasionally.
Case 2.
An eighty-year-old female patient presented with pain in her left hip. She had a clinical history of ipsilateral hip fracture treated with a proximal femoral nail (PFN, Synthes) 2 years previously, and had no other related medical condition. No antecedent of any further traumatic event was known, and she was not on any treatment for bone disease. Clinical examination of hip mobility increased the pain, which was particularly painful in internal and external rotations. No abnormalities were seen in the AP pelvis X-ray (Fig. 6).

Anteroposterior pelvis x-ray of an 80-year-old female patient. Normal osteosynthesis of a left perthrocanteric fracture at 2-year follow-up with a screw-nail device can be seen.
The patient was sent home with pain medication. At the one-month evaluation she still had groin and thigh pain, and a left transverse acetabular fracture with mild medial protrusion of the femoral head was observed radiologically (Fig. 7 – arrow-).
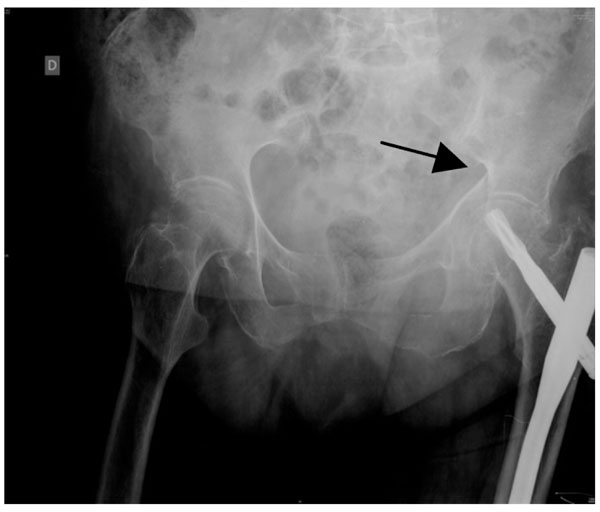
Anteroposterior pelvis X-ray of the same patient, one month later. A left acetabular transverse fracture is evident, with mild medial displacement of the femoral head.
Careful examination of the initial X-rays revealed that the ilio-ischial line was interrupted at the greater sciatic notch (Fig. 6). Bed rest without traction for one month was prescribed, followed by sitting and walking without weight bearing for a further month. A subsequent x-ray, 2 months later, showed that the fracture had probably healed (Fig. 8). This conclusion was consistent with the fact that the patient had much less pain under passive and active hip motion. She could walk with a slight limp and the help of a walker.

Anteroposterior pelvis X-ray two months later. Fracture consolidation.
Case 3.
An otherwise healthy eighty-three-year-old female patient operated on by bilateral hip replacement (Spotorno, Protek) for osteoarthritis, eight years before on the right side, and seven years previously on the left, felt acute pain in her right groin after getting up from sleep. She was not taking any drugs interfering with bone metabolism, and did not recall any fall. Clinical examination of hip mobility revealed exacerbation of the pain, particularly in external and internal rotation. X-rays of the pelvis were taken and no fracture was found. Thickening of both iliopubic rami and ischia was found, as a previous stage of a stress fracture (Fig. 9). As the pain increased during the following weeks, another X-ray was taken two months later (Fig. 10).

No fracture was found, although thickening of both iliopubic rami and ischia could be seen, resembling the prior stage of a stress fracture.

Anteroposterior x-ray of an 83-year-old patient with groin pain. Non-union of the right anterior acetabular column and ischium can be seen. An apparently healed fracture in the left anterior acetabular column is also visible.
A fracture of the anterior acetabular column distal to the anterior acetabular wall was observed [16], the apparent result of an anteroposterior pelvic trauma [17, 18]. Home bed rest without traction for two weeks followed by walking with weight bearing was prescribed, and during follow-up a non-union of the fractures became evident (Fig. 11). No further treatment was applied and the pain slowly eased until the patient felt reasonably comfortable walking. Non-union was considered to be the definitive result, and the patient was able to walk with the help of a single crutch.

Anteroposterior x-ray of the same patient at one year follow-up. Non-union is not resolved.
DISCUSSION
Various studies have shown that acetabular fractures in the elderly population are marked by a high degree of variability in terms of patient and fracture characteristics [12].
The typical acetabular fracture in the elderly was previously considered to involve the anterior column and a posterior hemitransverse fracture [7], but it is now known that older patients tend to have acetabular fractures with medial displacement patterns and associated comminution, particularly of the quadrilateral surface together with displacement of the anterior column and roof impaction [5, 8]. In any case, occult acetabular fractures in elderly patients are very rare.
In none of the three cases published by Kakkar et al. [13] were the fractures evident on the initial plain radiographs. All patients had suffered a previous fall and were unable to bear weight. Cross-sectional imaging and repeated plain radiography confirmed fractures of the acetabulum. The authors concluded that an occult acetabular fracture may occur in elderly patients after a fall and present with persistent discomfort and difficulty in walking. None of our patients, however, presented an antecedent of fall in their clinical history following the initial operation. However, in all three cases previous surgery with a metal implant in the ipsilateral hip had been carried out.
In the case published by Lasanianos et al. [9], a 69-year-old patient suffered an occult acetabular fracture complicated by an ipsilateral femoral neck fracture within 2 months. The acetabular fracture remained undiagnosed at examination due to inadequate clinical and radiographic data interpretation. Mann et al. also failed to correctly diagnose their case [15], and we, too, missed the correct diagnosis in all the cases described, due to the slight degree of displacement.
All three of our patients were female; two had a transverse fracture, while the third had an anterior column fracture distal to the joint. In this latter case, a fracture of the ipsilateral ischium was accompanied by the anterior column fracture. The presence of an implant may have influenced the appearance of what was diagnosed as a stress fracture due to osteoporosis. In one patient migration of the acetabular cup was observed at the two-year follow-up. This might have been due to the absence of posterior column osteosynthesis; this osteosynthesis was not achieved as the patient was treated in accordance with Slooff’s technique for revision arthroplasty [19]; however, since the acetabular cup fitted well with cementation, and no cavitary defect was found, no bone graft was used. Probably if this acetabular defect had been considered as a grade V pelvic discontinuity, in accordance with the classification proposed by Paprosky et al. [20], osteosynthesis of the posterior column would have prevented cup migration. Nevertheless, no loosening was found at the six-year follow-up.
In the case reported by Lasanianos et al. [9], no migration of the implant was observed after the operation; however, this case corresponded to an occult traumatic acetabular fracture, and an ilio-inguinal approach for anterior column osteosynthesis was taken [9]. In the case described by Angles et al. [14], no traumatic episode was present in the clinical history.
Some authors advocate additional diagnostic studies in cases of an injury in the hip area after a previously missed diagnosis of occult acetabular fracture. Such additional studies may include Judet view radiographs, bone scanning, computed tomographic scans or magnetic resonance imaging [13, 14]. In our cases, the x-rays were repeated after the initial mis-diagnosis; no CT-scan was needed as secondary displacement occurred in all cases. No further bone studies, either by images or biochemistry, were performed before treatment as it was considered that these would not produce any change in the therapeutic decision taken.
Since acetabular fractures in the elderly may occur after mild injury [9] and in some cases there is no apparent antecedent of trauma [10], the diagnosis may be missed [11]. The decision as to when a CT-scan should be performed is unclear; it is probably indicated in any elderly patient with groin pain and normal x-rays. Nevertheless, the validity of this approach remains to be elucidated. In our experience, the fracture was easily seen in x-ray examinations during subsequent weeks.
We believe that whenever an elderly patient feels groin pain, and anteroposterior pelvis X-rays are normal, oblique (obturator and iliac) Judet projections should be obtained. In all our cases, and in those described in the literature, a homolateral proximal femur implant was present; this could be related to the acetabular fracture, by a stress shielding mechanism, but more cases need to be studied to confirm this hypothesis.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflicts of interest.
ACKNOWLEDGEMENTS
Declared none.


