All published articles of this journal are available on ScienceDirect.
Current Concepts of Prophylactic Antibiotics in Trauma: A Review
Abstract
Traumatic injuries cause 5.8 million deaths per year globally. Before the advent of antibiotics, sepsis was considered almost inevitable after injury. Today infection continues to be a common complication after traumatic injury and is associated with increases in morbidity and mortality and longer hospital stays. Research into the prevention of post-traumatic infection has predominantly focused on thoracic and abdominal injuries. In addition, because research on sepsis following musculoskeletal injuries has predominantly been on open fractures. There is a paucity of research into the prevention of soft tissue infections following traumatic injuries. This review analyses the evidence for the role of prophylactic antibiotics in the management of soft tissue injuries. Emphasis is placed on assessing the strength of the presented evidence according to the Oxford Level of Evidence scale.
INTRODUCTION
Traumatic injuries are a significant cause of death, with 5.8 million deaths per year globally [1]. Before the advent of antibiotics, sepsis was considered almost inevitable after injury [2]. Although no longer the case, infection continues to be a common complication after traumatic injury and is associated with an increase in morbidity and mortality, and longer hospital stays [3]. Whilst not a priority at the time of critical illness, infective complications can also result in poorer cosmetic outcomes [4].
Research into the utility of prophylactic antibiotics in traumatic injuries has focused on thoracic and abdominal injuries [5, 6]. Sanabria et al. performed a systematic review and meta-analysis of randomised control trials (RCTs) comparing the effectiveness of prophylactic antibiotics versus placebo in patients with isolated chest trauma [5]. Patients were included if they had received blunt or penetrating trauma. Patients receiving antibiotics had a significantly reduced rate of posttraumatic empyema (RR 0.19) and pneumonia (RR 0.44) than controls. These results were supported by a systematic review by Bosman et al. which found that patients who received prophylactic antibiotics had a lower risk of developing empyema (OR 0.32) [7]. In Bosman et al.’s study, 1234 patients with isolated chest trauma received either a first generation cephalosporin or placebo at the time of chest drain insertion. Patients who benefitted the most from prophylactic antibiotics were those with penetrating injuries (OR 0.28) whereas no benefit was seen in those suffering blunt thoracic trauma (OR 1.30). Together these studies provide good evidence supporting the use of prophylactic antibiotics in patients with chest trauma.
When considering the use of prophylactic antibiotics in abdominal trauma, a Cochrane review by Brand et al. suggested that there was insufficient data on which to base guidelines as there were no studies of sufficiently strong methodology found [6]. However, almost a decade ago, guidelines recommending the use of prophylactic antibiotics in penetrating trauma had been produced [8]. The difference in conclusions between the authors of these guidelines and of the systematic review suggests that the general debate is ongoing.
With regard to musculoskeletal trauma, research has concentrated on soft tissue injury in open fractures. Guidelines on the use of prophylactic antibiotics in both civilian and military populations with open fractures have been published [9, 10]. The use of prophylactic antibiotics in the treatment of open fractures in the military has provided a great deal of supporting evidence for these guidelines [7]. This focus on open fractures has resulted in a paucity of research into the prevention of infection in soft tissue injuries without associated bony injuries. This review analyses the evidence for the role of prophylactic antibiotics in the management of soft tissue injuries, both with and without associated bony injuries. Emphasis has been placed on assessing the strength of the presented evidence according to the Oxford Level of Evidence (OLE) scale (Table 1).
Oxford Level of Evidence Scale
| Level 1: Meta-analysis of randomized controlled trials (RCT) or high quality RCTs |
| Level 2: Lesser quality RCTs or prospective comparative studies |
| Level 3: Case control studies or retrospective studies |
| Level 4: Case series without the use of comparison or control groups |
| Level 5: Case reports or expert opinion |
LITERATURE SEARCH AND OUTCOME
MEDLINE and EMBASE were searched using the National Health Service evidence interface (www.evidence.nhs.uk) in August 2012 using the term:
Duplicate filtered: [(prophyla* AND trauma AND (antibiotic* OR antimicrobial*) AND injury). ti, ab Limit to: English Language and (Year Published Last 30 Years)]].
Articles included were those relating to the management of musculoskeletal soft tissue trauma using prophylactic antibiotic therapy, and all articles regardless of the severity of disease and age range of population studied were included. Articles were included if they were systematic reviews or randomised control trails (RCTs) (either OLE 1 and 2) or if they were case control studies or retrospective studies providing a comparison (OLE 3). Articles were excluded if they related soft tissue trauma associated other systems such as the alimentary system or within the context of polytrauma (Table 2).
Articles Included from Literature Search
| Article | OLE, Study Type | Population | Comparison | Outcome Measures and Findings |
|---|---|---|---|---|
| Harley et al., 2002 [11] | 3: retrospective comparison study | 227 patients, 241 long bone fractures | Time to definitive treatment divided into 3 groups: <5, 5-10, or >10 hours | Incidence of infection and non union associated with fracture grade (p<0.05), not time to treatment (p>0.05) |
| Hauser et al., 2006 [12] | 2: Systematic review | 16 OLE 1 and 2 articles (no meta-analysis: total number of patients not given) | Prophylactic Antibiotics in open fractures vs placebo vs no medication in the treatment of open fractures | 24h 1st generation cephalosporins reduce incidence of wound infection; no significant effect in open hand trauma |
| Patzakis et al., 1974 [13] | 2: placebo controlled RCT | 310 patients with open fractures; randomised | Placebo vs 10 day course of penicillin + streptomycin vs 10 days of cefalothin | Reduced incidence of wound infection with cefalothin only compared to placebo (13% vs 2.3%, p<0.05) no difference with use of penicillin + streptomycin (13% vs 9.7%, p<0.45) |
| Dellinger et al., 1988 [14] | 2: double blinded RCT | 248 patients with open fractures; randomised | 1 day course of cefonicid vs 5 days of cefonicid vs 5 days of cefamandole | No reduction in infection rates with longer prophylactic course (13% vs 12% vs 13%; p>0.5) |
| Braun et al., 1987 [15] | 2: double blinded placebo controlled RCT | 100 patients with open fractures; randomised | 10 day course of cloxacillin vs placebo | Reduction in infection rate with use of cloxacillin (4% vs 24%, p<0.05) |
| Hansraj et al., 1995 [16] | 2: prospective comparative study | 100 patients with gun shot wounds of the hand; alternating treatment given | 2 day course of ceftriaxone vs 2 days of cefazolin | No difference in infection rate (p>0.05) |
| Suprock et al., 1995 [17] | 2: prospective comparative study | 91 open finger fractures; alternating treatment given | 3 day course of 1st generation cephalosporin, dicloxacillin or erythromycin vs no treatment | No significant difference in infection rates (9% vs 9%, p>0.05) |
| Stevenson et al., 2003 [18] | 2: double blinded placebo controlled RCT | 193 open distal phalanx fractures; randomised | 5 day course of flucloxacillin vs placebo | No significant difference in superficial or deep wound infection rates (3% vs 4%, p>0.05) |
| Altergott et al., 2008 [4] | 2: RCT | 135 distal fingertip injuries in children; randomised | No prophylaxis vs 7 day course of cefalexin | No significant difference in wound infection rates (1.45% vs 1.52%, p>1) |
| Whittaker et al., 2005[19] | 2; placebo controlled RCT | 170 adults with clean hand lacerations including tendon + nerve damage; randomised | Oral placebo vs Intravenous (IV) flucloxacillin single dose at induction vs IV flucloxacillin at induction+ 5 day course of oral flucloxacillin | No significant difference in wound infection rates (15% vs 13% vs 4%, p>0.05) |
| Gerhardt et al., 2009 [20] | 3: retrospective cohort study from field medical records | 53 US troops suffering soft tissue injury in battlefield | None IV 3rd generation cephalosporin + wound irrigation | Wound infection 48 hours post injury increased in those not using prophylactic antibiotics (7% vs 40% p<0.05); increased wound infection in those not undergoing wound irrigation (4.5% vs 40%, p<0.05) |
This search produced 173 abstracts that were reviewed for relevance. Removing duplicate articles reduced the number of abstracts to 120. After applying exclusion criteria, 32 potentially relevant papers were then reviewed including their references by two authors (Fig. 1). Two articles were unavailable, and six were conference abstracts and 13 were of insufficient quality or relevance. Of the remaining full text articles, 11 studies were included in the critical analysis. All included studies were assigned a level of evidence using the Oxford scale. Guidelines were advanced and also assigned a grade using a published scale (Table 3) [21].
Grades of Recommendation are Assigned According to the Level of the Evidence and its Applicability to a Target Population [21]
| Grade A: level 1 evidence that is directly applicable to the target population |
| Grade B: Extrapolated level 1 evidence, or directly applicable level 2 evidence |
| Grade C: Extrapolated level 2 evidence or directly applicable level 3 or 4 evidence |
| Grade D: All other evidence from case reports and expert opinion |
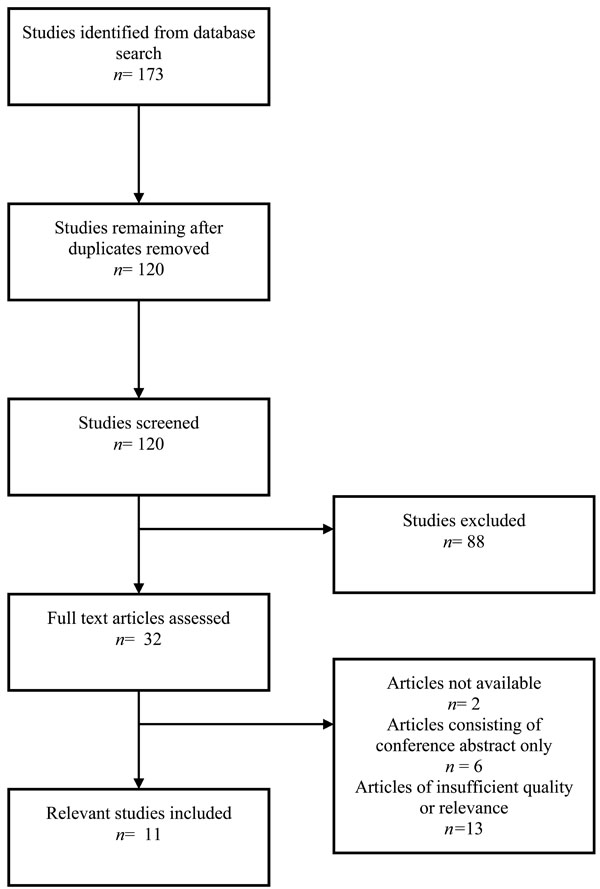
Flow chart for included studies from literature search.
SOFT TISSUE INJURIES ASSOCIATED WITH BONY INJURY (OPEN FRACTURES)
Whilst infection has been found to be a significant adverse outcome in all open fractures [3], it is first necessary to examine the subpopulations found in the literature to be more prone to this complication. Harley et al. retrospectively reviewed the records of 227 patients who had presented with 241 open long bone fractures to a single trauma center over a two year period [11]. They found that time to definitive treatment did not significantly affect infection rate or rate of non union whereas the presence of infection was significantly increased in more severe fractures, as graded according to Gustillo and Anderson’s scale (Fig. 1) (Gustillo grade 3 OR 5.95, p< 0.05) [22]. The rate of infection also significantly increased the incidence of non-union (OR 35.97, p<0.05). This study refutes traditional teaching that open fractures must receive definitive treatment within six to eight hours [23] however the researchers comment that 92% of patients received treatment within 13 hours and therefore limits their results to this timeframe. In addition to the retrospective nature of the study, the researchers also commented that whilst ‘standard treatment’ was given to all patients over the three year period, treatment was not uniformly provided following a protocol, potentially causing outcomes to differ depending upon the attending surgeon (Table 4).
Gustillo Classification of Open Fractures [22]
| Grade (Type) I: Open fracture with a skin wound less than 1 cm |
| Grade (Type) II: Open fracture with a laceration more than 1 cm without extensive soft tissue damage |
| Grade (Type) III: Open segmental fracture, open fracture with extensive soft tissue damage, or a traumatic amputation. |
Modern protocols of the management of open fractures are still based on research accumulated decades ago [24]. The problem with relying on this early evidence is that it usually is not of a level high enough to be considered the basis of modern guidelines. For example, Hauser et al.’s systematic review of civilian literature found that there was a lack of modern evidence for the most appropriate choice of antimicrobial agent whilst old evidence has significant methodological flaws [12]. They found that the majority of studies were of OLE level 3 or below, with only 16 studies containing any prospectively collected data or randomization. After analysing the OLE level 1 and 2 studies they found, Hauser et al. recommended that patients with open fractures should receive a short course prophylactic first generation cephalosporins (approximately 24 hours) of soon after injury. However, conclusions from this systematic review may be limited because no meta-analysis was conducted, perhaps due to the procedural heterogeneity of the studies. An RCT undertaken by Patzakis et al. in 1974 remains at the core of the evidence supporting the use of antibiotic prophylaxis [13]. The study included 310 patients who were randomized into three groups to receive either a prophylactic ten day course of penicillin and streptomycin, cefalothin or placebo, and four cultures from the wound site were taken, one prior to intervention and three following. A statistically significant difference in wound infection rate between those receiving cefalothin and those receiving placebo (2.3% vs 13.9%, p< 0.05) was found, but no significant difference between those patients receiving penicillin and streptomycin or placebo (9.7% vs 13.9%, p< 0.45). Limitations of the study however are that the majority of fractures were lower limb, especially tibial fractures, and that the researchers did not classify the severity of the fractures. Further research is therefore needed to ensure that these results also apply to upper limb fractures, and to all grades of open fracture.
Further evidence for the use of short courses of antibiotic prophylaxis was found by Dellinger et al. who investigated the difference in fracture site infection rates depending upon type of antibiotic and duration of treatment used [14]. No significant difference in infection rates were seen in patients randomized to one of three groups: one day or five days of cefonicid or five days of cefamandole a second-generation cephalosporin (13% vs 12% vs 13%, p>0.5). These recommendations are supported by Braun et al. who investigated the effect of single agent antibiotic prophylaxis versus placebo and found that patients with open fractures who received cloxacillin had a significantly lower infection rate than those who received a placebo (4% vs 24%, p<0.05) [15]. In contrast, studies of the effect of prophylactic antibiotics versus placebo in open hand fractures after low velocity gunshot wounds [16], open finger fractures [17], and open distal phalanx fractures [18] found no significant differences in the outcomes in intervention and control groups. However, soft tissue injuries of the hand tend to have less soft tissue involvement. For example, patients included in the study Hansraj et al. had soft tissue involvement mostly less than 1 cm at its greatest diameter [16]. Perhaps the need for prophylactic antibiotics is dependent on the scale of soft tissue involvement and damage to supplying vasculature, since Suprock et al. specifically excluded those with digital arterial damage in their RCT [18].
Although military research has increased the evidence base on the role of prophylactic antibiotics for soft tissue injuries, generalisation of such studies to civilian populations must be done with care. Recent military guidelines such as those produced by the Eastern Association for the Surgery of Trauma (EAST) highly recommend the use of prophylactic antibiotics in soft tissue trauma and open fractures [25]. Using evidence found by a systematic review undertaken in 1997, evidence from the 313 papers included was reviewed by an expert panel including orthopaedic and general surgeons. Hauser et al. however have also assessed evidence given for these guidelines in civilian literature, with different interpretations found [13]. Conflicting interpretations surround the use of aminoglycosides for Grade 3 Gustillo fractures. The use of an additional antibiotic as gram-negative prophylaxis was initially suggested by Patzakis et al. due to the increased incidence of wound infections in severe open fractures found in their seminal paper [13]. The EAST group therefore proposes additional gram-negative cover for grade 3 Gustillo fractures. This conclusion had been considered to be extrapolation in civilian literature since Paztakis et al. used antibiotics that predominantly only cover gram-positive organisms in the RCT itself, and their suggestion for the inclusion of gram-negative cover was only a discussion point due to wound culture results. This inconsistency of opinion emphasizes that insufficient evidence has yet been seen for the addition of gram-negative prophylactic cover for those patients suffering grade 3 fractures, and that debate is ongoing.
The EAST guidelines concur with civilian findings that level 2 evidence supports the use of gram-positive cover for all open fractures [25]. However, they suggest the use of antibiotic regimes of high dose intravenous 3rd generation cephalosporins rather than oral 1st generation drugs seen in civilian patients. This adaptation is proposed as it combines primary evidence with the logistics of in-the-field administration and concerns regarding incorrect dosage in this young, muscular and predominantly male population [9]. With the guidelines also commenting that the majority of open fractures studied in the military population are Grade III, this may be another reason why results from research in military personnel may not be appropriate for extrapolation to the civilian cohort. However, as the use of aminoglycosides is now routine in the military, further primary data may be produced to add to the debate surrounding their use [26].
After the generation of the EAST guidelines, a retrospective observational study was undertaken by Barton et al. to examine the effect of compliance with these guidelines for the use of antibiotic prophylaxis with the incidence of infection [26]. Patients admitted over a four year period were included in this audit and divided into two groups depending on their adherence to the EAST guidelines. There were 214 patients included, and although there was no significant difference in incidence of infection between the groups (17.0% vs 11.5%, p< 0.313), patients who received antibiotic regimens that were non-compliant with guidelines had a significantly prolonged hospital stay (6 vs 3 days, p< 0.0001). The main reason for non-compliance with guidelines was exceeding the recommended number of days of recommended antibiotic prophylaxis (either three days from injury or until 24 hours after wound closure). It could be considered therefore that these results may have been confounded by clinically unwell patients receiving further antibiotics due to clinical condition, rather than non-compliance causing a longer hospital stay.
Recommendation:
Civilian populations presenting with open fractures benefit from a short course of 1st generation cephalosporins given as soon as possible after the injury. Hand fractures do not require routine prophylaxis, and this may extend to other open fractures with minimal soft tissue loss in future with further research. It is still unclear whether additional gram-negative prophylaxis provides net benefit to patients presenting with Gustillo III fractures. Caution should be employed when extrapolating evidence from military populations due to the difference in patient demographic, aetiology of injuries, severity, environmental exposure to pathogens and logistical constraints.
Level of evidence: 1 and 2.
Grade of recommendation: B.
SOFT TISSUE- PENETRATING TRAUMA
In comparison to what is now known regarding the prevention of infections following open fractures, less is known regarding the prevention of infection after soft tissue injury alone.
Two RCTs regarding the use of antibiotics in hand trauma were found in the literature search. Altergott et al. investigated the effect of prophylactic antibiotics in 135 children presenting with distal fingertip injuries [4]. Study participants were randomised to receive either no antibiotics or cefalexin after washout in the emergency department. All children were reviewed at 48 hours and patients’ relatives received a telephone enquiry at one week to ask regarding clinical signs of infection, after which children were reviewed if it there was a clinical suspicion of wound infection. The primary outcome measure was the presence of infection at seven days post-initial consultation. There was no statistically significant difference found in the incidence of post-traumatic infection between the intervention and control groups (1.52% vs 1.45%, p< 1.00). There are a few limitations to this study. Whilst the method of randomization is well documented, there is no mention of blinding, especially considering no placebo was given to the control group which could have affected the response of clinicians who reviewed children at one week. The lack of placebo may also have affected the perception of wound appearance reported by the parent, since they may have had pre-existing opinions regarding the need for antibiotic prophylaxis that skewed their opinion.
Results concordant with this study have been reported in adults. Whittaker et al. investigated the role of prophylactic antibiotics in 170 patients presenting with clean hand injuries of the skin, including tendon and nerve injury [19]. Patients were randomized prior to surgical management into one of three groups: intravenous (IV) flucloxacillin at induction of anaesthesia followed by a 5 day course of oral placebo, IV flucloxacillin followed by a 5 day course of oral flucloxacillin or oral placebo only. The primary outcome measure was the incidence of wound infection. Infection was seen in 13% of those who received one IV dose at induction, 4% in those receiving both IV and oral antibiotics, and 15% of those in the control group. However, there was no statistical significance in the rate of post-operative infection between the groups, suggesting that soft tissue injuries without gross contamination may not require antibiotic prophylaxis if receiving definitive surgical management.
Gerhardt et al. performed a retrospective analysis of 53 troops presenting with penetrating soft tissue injuries in Iraq [20]. They compared the incidence of wound infection at 48 hours post injury in troops divided into four groups; those who took antibiotic prophylaxis and underwent early irrigation of the wound as is recommended in military guidelines, those who did not receive recommended antibiotics, those who did not receive early irrigation of the wound and those who received neither antibiotics nor irrigation. Seven percent of those who took antibiotic prophylaxis developed wound infections compared to 40% of those who did not (OR 0.11). The incidence of infection was also markedly lower in the group that received irrigation as part of initial first aid (4.5% versus 40%, OR 0.04). Those who combined the use of prophylactic antibiotics and early wound irrigation showed a statistically smaller difference in infection rate when compared to either intervention alone (p<0.0005). The authors therefore suggested a combined approach using both irrigation and systemic antibiotic to produce the most significant reduction in post traumatic infection. However, it must be remembered that as a retrospective study of a small cohort in a hostile environment, care should be taken when interpreting these results, especially due to the large difference in size between intervention and control groups.
Recommendation:
The evidence suggests that the rate of post-traumatic infection is not statistically reduced by antibiotic prophylaxis at the time of definitive management of finger tip injuries and clean hand lacerations involving deep structures. Evidence is based on lesser quality small RCTs and the subject would benefit from further structured investigation. Wound irrigation and antibiotic prophylaxis appear to have an additive effect in the management of penetrating soft tissue injuries in military populations, although higher level evidence is needed to confirm this.
Level of Evidence 2:
For hand injuries and lacerations, level 3 for importance of antibiotics in military soft tissue injuries.
Grade of recommendation:
B for hand injuries and lacerations, C for importance of antibiotics in military soft tissue injuries.
DISCUSSION
The literature search identified 11 articles that met the inclusion criteria, the majority of which were OLE 2 quality. Most of the research into the prevention of soft tissue infections following trauma and the use of antibiotic prophylaxis, has concentrated on open fractures. As well as primary military and civilian literature, guidelines were also found and the evidence used in formulating them was analysed.
Some guidelines for the use of prophylactic antibiotics in musculoskeletal trauma use evidence extrapolated from elective surgery or from military studies to produce the guidelines we use for the civilian cohort [27]. However, because military personnel represent a different demographic suffering severe musculoskeletal trauma in hostile environments alien to civilian life, and the mechanism of combat and the logistical constraints on medical and surgical management dictate that care must be taken when transferring this evidence for use within the civilian setting.
Limitations of the search were the difficulty of defining an appropriate search term to contain all potential studies, partly due to the vast number of injuries that can be included under the term ‘soft tissue’. Limitations of the review also lie in the quality of the literature available since no level 1 studies were found, and it could be argued that research into the management of soft tissue injuries lags behind study into abdominal and thoracic trauma. The studies found that focused solely on soft tissue injury also concentrated on upper limb trauma, which may reflect the higher incidence of these minor injuries. This research may be transferrable to lower limb injuries with only small areas of soft tissue loss, although care should be taken considering higher rates of infection in lower limb injuries have previously been reported [13].
As specialist trauma centres emerge, the opportunity for the production of a higher level of evidence into soft tissue traumatic injuries may grow. Studies emerging from critically unwell surgical patients currently represent a heterogeneous group due elective and trauma patients being cared for together in surgical intensive care units. With the advent of specialist trauma centres the critically ill trauma cohort may be separated from their elective surgical and medical counterparts. This may improve the quality of research that can be undertaken, and produce improved guidance for those suffering civilian polytrauma.
In addition to the use of prophylactic antibiotics, the role of surgical debridement and transfer to a definitive specialist trauma centre are emerging as important in reducing the incidence of infective complications after trauma to the extremities. A recent retrospective review of practice in level 1 trauma centres found no significant difference in outcome with delayed surgical debridement as traditionally taught, but that transfer time from injury to trauma centre was an independent factor of adverse outcome [28]. As a formal trauma network was recently put in place in the United Kingdom, comparison of survival statistics before and after this change was initiated will show whether similar results are seen in the UK. The role of topical antibiotics has begun to be explored within the prophylaxis of burns injuries, and therefore future work may also be rewarding in the development of evidence for their use in similar depth soft tissue injuries [29].
Care must be taken however that the use of antibiotics does not lead to complications. There is already evidence from the study of critically ill surgical patients that prophylactic antibiotics of long duration involving multiple agents can lead to the development of resistant infections [30]. Prophylactic antibiotics have also been shown to be a risk factor for the development of Clostridium difficile infection in a young cohort of trauma patients requiring intensive care management [31]. It is complications such as these that emphasise the importance of research into further defining the groups who benefit from antibiotic therapy. Whilst this review discusses the prevention of infection from bacteria, further work may also begin to study the importance of other pathogens. The threat of explosions from terrorist attacks has opened the possibility of biological weapons in the form of blood borne viruses and the prophylaxis of these infectious sequelae of traumatic injuries may also warrant further investigation [32].
CONCLUSIONS
There is some level 2 evidence supporting the use of prophylactic antibiotics in the treatment of open fractures. Evidence from the study of musculoskeletal injury in both civilian and military cohorts notes the importance of short course, single agent regimens using cephalosporins in order to prevent adverse outcomes in open fractures. However, there is no conclusive evidence supporting prophylactic antimicrobial use in the management of small soft tissue upper extremity trauma and simple lacerations.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


