All published articles of this journal are available on ScienceDirect.
‘Not Always a Baker’s Cyst’ – An Unusual Presentation of a Central Voluminous Postero-Medial Meniscal Cyst
Abstract
Meniscal cysts are rare and often are a result of extrusion of synovial fluid through a tear of the meniscus, resulting in a one-way valve effect of the tear. Arthroscopic partial meniscectomy of the meniscus with intra-articular cyst drainage has become the standard of care. We report a case of an unusually large symptomatic medial meniscal cyst, situated postero-medially and pressing on the posterior cruciate ligament, which was initially clinically misdiagnosed as a Baker’s cyst. The patient had difficulty and pain on squatting. He was successfully treated with arthroscopic debridement and needle decompression; a rarity in literature for such a voluminous perilabral cyst tenting the posterior cruciate ligament. This procedure has the advantage of being able to obtain the cystic fluid for histological and cytological analysis before debridement. This case also highlights the importance of the use of Magnetic Resonance Imaging (MRI) to accurately diagnose a central, posterior knee swelling.
INTRODUCTION
Meniscal cysts are relatively uncommon affecting about 4-8% of the population [1]. Most meniscal cysts are associated with horizontal tears of the meniscus, with communication of synovial fluid into the meniscocapsular complex. Meniscal cysts have been reported to be 3 to 10 times more commonly associated with the lateral meniscus rather than the medial meniscus [2]. The size of the cyst depends on the amount of synovial fluid extruded during motion of the knee joint [3]. Patients may present with a palpable mass over the joint line or complain of pain over the joint line [4]. Treatment of symptomatic meniscal cysts would depend on the presence of a tear and can range from arthroscopic partial meniscectomy and cyst decompression to open cyst decompression and meniscal repair [5-7].
We present an unusual case of a large postero-medial meniscal cyst which was initially misdiagnosed as a Baker’s cyst. AMagnetic Resonance Imaging (MRI) scan confirmed the diagnosis. The cyst was decompressed with a needle and a syringe under direct visualization and was subsequently debrided arthroscopically. Twenty-four months post-surgery, there was no sign of recurrence and the patient was pain-free and leading an active lifestyle.
CASE REPORT
A 47-year old male presented to the specialist outpatient clinic at a tertiary university hospital after being referred from a general practitioner, with an initial diagnosis of a Baker’s cyst of his right knee. The patient presented with a one-year history of localized pain over theposterior aspect of his right knee. The pain had been recurrent over the last year and was particularly exacerbated with squatting. There were recurrent episodes of swelling noted over the last 8 months associated with intermittent locking of the knee joint. The patient had no previous trauma to the knee and did not engage in sports regularly. On examination, there was a discrete 4cm diameter hemispherical cystic mass at the popliteal region of the patient’s right knee. The mass was fluctuant, firm and cystic on palpation. It was tender and immobile and was also more apparent on extension of the knee. No joint effusion was noted but medial joint line tenderness, particularly over the posterior horn of the medial meniscus, was elicited. Range of motion was 0 to 120 degrees passively, but terminal flexion was uncomfortable. There was no ligamentous instability. McMurray’s test was negative. Radiographic images of both knees did not reveal any abnormalities.
MRI scans of the right knee demonstrated a complex multidirectional tear involving the posterior horn and posterior junction of the medial meniscus, with an oblique component extending to the superior and inferior articular surfaces. A horizontal tear through the posterior horn extending postero-medially was also identified (Figs. 1, 2). The MRI also showed a complex multilobulated, multiseptated intra-articular cystic lesion abutting the posterior margin of the posterior horn of the medial meniscus. The cyst also extended to the intercondylar region, abutting the posterior margin of the posterior cruciate ligament. The cyst was found to communicate with a defect along the posterior margin of the posterior horn of the meniscal tear. The cyst measured to be 3.8 X 2.5 (axial dimension) X 3.0 cm (craniocaudal dimension). Another smaller, elongated, septated cystic complex was identified extending supero-medially adjacent to the medial femoral condyle, posterior to the medial collateral ligament. Thissmaller component measured 1.5 X 0.4 (axial dimension) X 1.7 cm (craniocaudal dimension). The lateral meniscus was intact and normal in configuration. No significant articular cartilage defect or bone contusion was seen and no ligamentous abnormalities were noted (Fig. 3).

MRI (sagittal view) demonstrating a horizontal meniscal tear extending through the posterior horn.
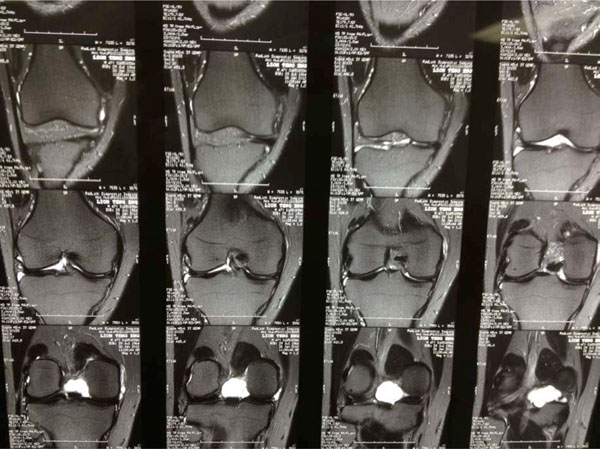
MRI (coronal view) demonstrating a horizontal meniscal tear extending through the posterior horn, and the meniscal cyst.

MRI (sagittal view) demonstrating no significant articular cartilage defect or bone contusion or ligamentous abnormalities. A large meniscal cyst abutting the posterior cruciate ligament can also be seen.
The patient was diagnosed to have a complex degenerative tear of the posterior horn of the medial meniscus associated with a large multiloculated, parameniscal cyst. He was then scheduled for arthroscopic surgery.
Diagnostic arthroscopic examination of the knee was performed using standard anterolateral and anteromedial portals. Arthroscopy revealed a small tear of the posterior horn of the medial meniscus and a large perilabral cyst (Fig. 4). The cyst was punctured and aspirated using a long 10G needle under direct visualization at arthroscopy (Figs. 5, 6). The cystic material was subsequently sent for cytology as well as histology. Following this, the remaining sac was debrided with a motorized shaver. Histological analysis of the gelatinous fluid revealed blood clots, macrophages and fibrinous material, with no malignancy identified. Post-operative recovery was very satisfactory and remarkable.
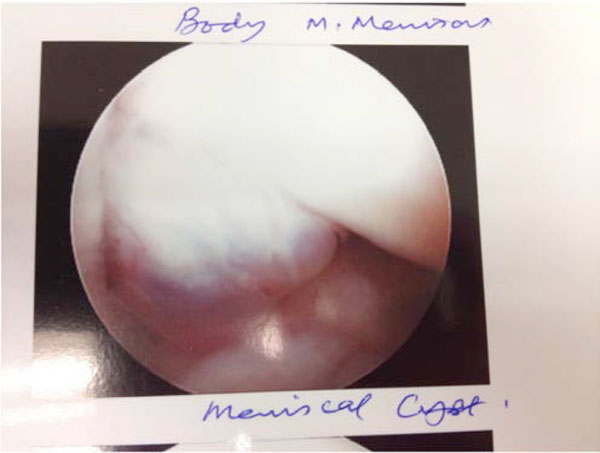
arthroscopic view demonstrating view of medial meniscal cyst.

Arthroscopic view of needle decompression of the meniscal cyst.
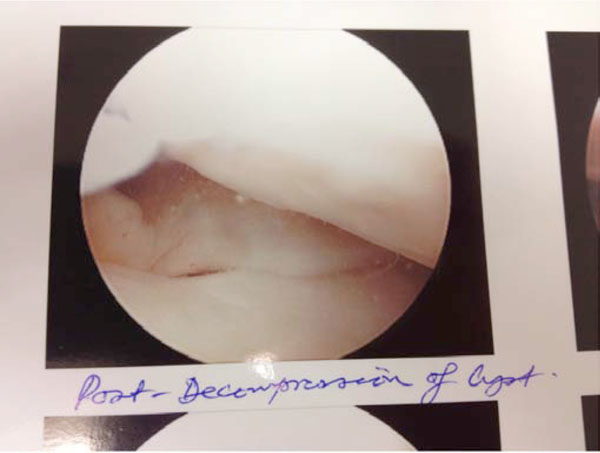
Arthroscopic view of the post-decompression of the meniscal cyst.
The patient was reviewed 24 months post-surgery. There were no signs of recurrence and the patient did not experience any pain, instability or locking of the knee. He was able to lead an active lifestyle.
DISCUSSION
Medial parameniscal cysts of the knee are typically 0.3 to 9mm in diameter [8]. Previous studies have described usually small parameniscal cysts but we are only aware of 3 previous case reports of a medial parameniscal cyst larger than 2 cm in diameterin English literature [9-11]. Furthermore, in all 3 cases, the meniscal cystswere openly excised. Open excisions of meniscal cysts pose greater risks of infection, inadvertent damage to the meniscus and surrounding structures during surgery, and longer time to recovery and return to mobility for the patient. This case highlights the management of a large posterior medial meniscal cyst that was managed arthroscopically with good post-operative recovery.
While small parameniscal cysts are rarely symptomatic, larger cysts located posteriorly may present with pain and persistent swelling due to pressure on surrounding structures [10-14]. Our patient experienced pain, recurrent swelling and locking over a period of 12 months.
A voluminous posterior medial meniscal cyst could present in the popliteal fossa, and coupled with its size, may be misdiagnosed as a Baker’s cyst. Distinguishing a meniscal cyst from a Baker’s cyst is important as Baker’s cysts are usually associated with osteoarthritis of the knee. They mayoften resolve spontaneously and hence be treated conservatively [15]. However, arthroscopic repair or debridement of a meniscal tear with the aim of preventing recurrence is the usual treatment for a meniscal cyst [3]. MRI and arthroscopy are useful in distinguishing a perimeniscal cyst from a Baker’s cyst in such a scenario. Most meniscal cysts (91%) occur immediately adjacent to the meniscal tear (98% horizontal cleavage tears, 49% anterolateral), with the tear communicating directly with the cysts, and produce a homogenous signal on MRI [16, 17]. Furthermore, demonstration of a Baker’s cyst origin between the muscles of the medial gastrocnemius and semimembranosus allows for differentiation from a meniscal cyst.
CONCLUSION
We present a 47-year old male patient, with an unusually large posterior medial meniscal cyst that was initially misdiagnosed clinically as a Baker’s cyst, due to its size and position. Careful clinical examination along with imaging studies, particularly MRI, will help in such diagnoses. This case report highlights that a large posterior medial meniscal cyst can be treated successfully with arthroscopic needle decompression and meniscal debridement without open excision. Good postoperative function and symptom relief are obtained, which suggest that arthroscopic management can be considered a viable alternative to open excision of large meniscal cysts.
ACKNOWLEDGEMENT
The figures have the written permission of the owner (National University Hospital (S) Pte Ltd).
CONFLICT OF INTEREST
The authors confirm that this article content has no conflicts of interest.


