RESEARCH ARTICLE
Secondary Patellar Resurfacing after Primary Bicondylar Knee Arthroplasty did Not Meet Patients’ Expectations
João Correia, Marc Sieder, Daniel Kendoff, Mustafa Citak, Thorsten Gehrke, Wolfgang Klauser, Carl Haasper*
Article Information
Identifiers and Pagination:
Year: 2012Volume: 6
First Page: 414
Last Page: 418
Publisher ID: TOORTHJ-6-414
DOI: 10.2174/1874325001206010414
Article History:
Received Date: 26/6/2012Revision Received Date: 25/7/2012
Acceptance Date: 3/8/2012
Electronic publication date: 7/9/2012
Collection year: 2012

open-access license: This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
Abstract
Secondary patella resurfacing is a controversial procedure which is applied in patients with anterior knee pain after a bicondylar knee arthroplasty (with unresurfaced patella). A group of 46 patients were submitted to this procedure and their satisfaction, range of motion and pain improvement was evaluated. 52.2% of the patients were satisfied with the procedure, with an improvement in pain (Visual Analogue Scale) of 65% and an improvement in range of motion in 56,5%, with roundabout half of the patients having no resolution to their complaints. Whilst an improvement was not achieved in all patients, as it was initially hypothesised, this procedure should be considered when a revision knee arthroplasty is performed with an unresurfaced patella.
INTRODUCTION
The first record of resurfacing of the patella performed in combination with a condylar resurfacing arthroplasty was performed by Groeneveld in 1970 [1, 2], with most knee replacement systems having an option for patella resurfacing since the beginning of the 1980s [2, 3].
In the literature, opinions vary when comparing the surgical practice applied, with the Swedish registry revealing resurfacing in 14% of the cases [4], whilst in the USA and Denmark, resurfacing is applied in 76% of the cases [4, 5].
In revision surgery of total knee prosthesis, secondary resurfacing of the patella is controversial as well. Usually performed in patients with anterior knee pain, where the patella was unresurfaced in the index procedure, improvements are expected in less than 60% of patients [3, 6-8]. The reasons for this are unproven for now, with a number of studies presenting conflicting information [9-12].
Many conditions surrounding the patellofemoral joint can give rise to anterior knee pain - patella maltracking, bony alterations (loose body impingement, osteophytes) and soft tissue conditions (complex regional pain syndrome, bursitis, peripatellar tendinopathy)[2] – thus making it difficult to treat.
An eventual screening tool could be the use of bone scans, with 95% of patients with anterior knee pain showing significant increased uptake (“hot patella”). The finding of a “hot patella” suggests that the problem is related to the patellofemoral joint [13]. Albeit, according to a recent study, there seems to be no relation between “hot patella” and subsequent improvement after secondary patella resurfacing [14, 15].
The aim of this study was to evaluate a group of patients, with bicondylar knee replacements, who were later submitted to secondary patella resurfacing, with the hypothesis that the procedure would be the resolution to their persistent anterior knee pain.
MATERIAL AND METHODS
During the period of November 2005 to October 2007, 48 patients with bicondylar knee replacements were submitted to secondary patella resurfacing. The follow-up ranged from 14 to 38 months, with 2 patients lost to follow-up.
The main indication for the procedure was persistent anterior pain knee (36 patients), with a secondary indication being range of motion restrictions due to arthrofibrosis (13 patients).
In total there were 18 male patients and 28 female patients, grouped according to their initial implant (bicondylar implants; rotating hinge implants; hinged implants) and further into 2 groups (patients with anterior knee pain and with arthrofibrosis).
The patients were telephonically interviewed, and enquired as to their:
- level of satisfaction – simple inquiry as to the satisfaction of the patient after the secondary resurfacing;
- range of motion – data recorded pre- and postoperatively and compared to what patients specified; inquiry as to the need of assistance when climbing up/down stairs;
- pain – Visual Analogue Scale recorded pre- and postoperatively, compared to the patients information;
- pain control medication – comparison of the patient medication preoperatively and the medication referred to during the interview.
Statistical Analysis
All variables were expressed in terms of mean ± standard deviation (SD) of the mean. A Student’s t test was performed when the data had a normally Gaussian distribution; otherwise the Mann-Whitney test was employed. The Shapiro-Wilk normality test was performed to ascertain whether the data were normally distributed. For all tests, p < 0.05 was considered statistically significant. Statistical analysis was carried out by means of a statistical software package (GraphPad Prism Version 4.1, GraphPad Software Inc., La Jolla, CA).
RESULTS
Patients
The mean age was 65 years (45y-81y). The mean time since the last procedure of the affected knee was between 12 months in the bicondylar implants and 18 months in the rotating hinge implants, with previous surgeries averaging 1.56 and 2.33 for the former and latter respectively (Figs. 1,2).
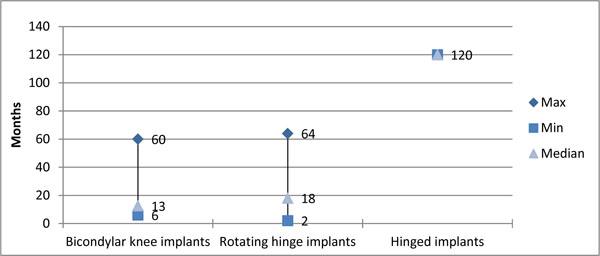 |
Fig. (1). Time passed since last surgery. |
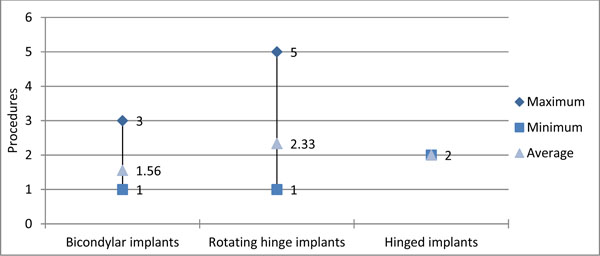 |
Fig. (2). Previous surgeries. |
The average body mass index (BMI) was 28.1 (primary implants) and 26.9 (rotating hinge implants).
Patient Satisfaction
Overall, 52.2% of the patients were satisfied with the secondary procedure (Fig. 3). When stratifying to specific implants and indications, the results were as shown (Table1).
Stratified Patient Satisfaction and Post-Operative Results
| Bicondylar Implants | Rotating Hinge Implants | Hinged Implants | Total | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Indication | AKP | AF | AKP | AF | AKP | AF | AKP | AF | ||||||||||||||||
| I | W | U | I | W | U | I | W | U | I | W | U | I | W | U | I | W | U | I | W | U | I | W | U | |
| Patient satisfaction | 10 | - | 5 | - | - | 3 | 8 | - | 9 | 5 | - | 5 | 1 | - | - | - | - | - | 19 | - | 13 | 5 | - | 8 |
| PO VAS | 12 | 1 | 2 | 1 | 1 | 1 | 9 | 2 | 6 | 7 | 1 | 2 | 1 | - | - | - | - | - | 22* | 3 | 8 | 8* | 2 | 3 |
| PO ROM | 9 | 4 | 2 | 1 | 2 | - | 9 | 5 | 3 | 6 | 3 | 1 | 1 | - | - | - | - | - | 19** | 9 | 5 | 7** | 5 | 1 |
PO – post-operative; AKP – anterior knee pain; AF – arthrofibrosis; I – improved; W – worsened; U – unchanged
* p < 0,05
** p > 0,05.
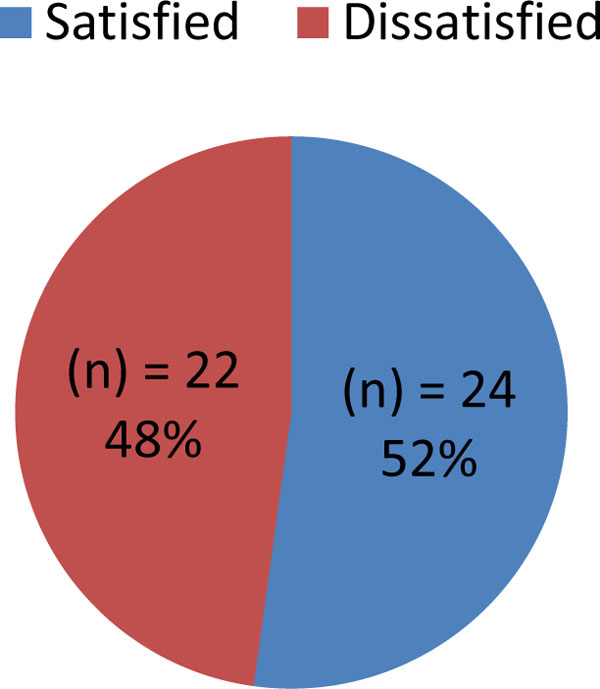 |
Fig. (3). General patient satisfaction. |
When correlating for age, half of the patients below the age of 70 benefitted from the procedure, while those above this age revealed no improvements.
Range of Motion
The postoperative range of motion was improved in 26 cases (Fig. 4) with no statistical significance, with varying results according to initial indications (Table1).
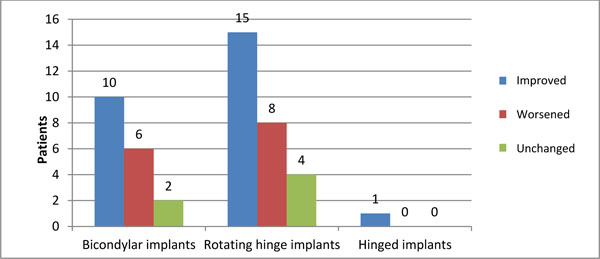 |
Fig. (4). Postoperative range of motion. |
Pain and Pain Management
The pain (VAS) improved significantly in 30 cases (Fig.5) in both the anterior knee pain and arthrofibrosis groups, with a decrease in postoperative painkiller use in 12 cases (6 increased, 28 unchanged).
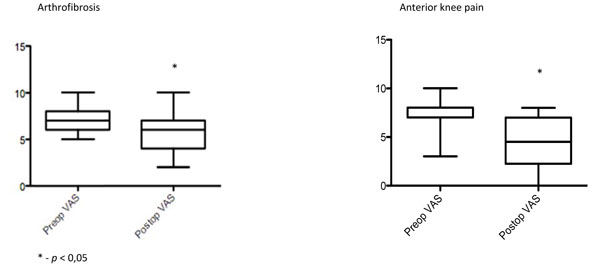 |
Fig. (5). – Postoperative pain evaluation (VAS). |
Other Procedures
During the secondary resurfacing, patients were submitted to soft-tissue procedures (Table 2).
Soft-Tissue Procedures
| Bicondylar Implants | Rotating Hinge Implants | Hinged Implants | Total | |||||
|---|---|---|---|---|---|---|---|---|
| Indication | AKP | AF | AKP | AF | AKP | AF | AKP | AF |
| Patella lateralization | 4 | 0 | 13 | 3 | 0 | 0 | 17 | 3 |
| Lateral release | 10 | 3 | 24 | 7 | 1 | 0 | 35 | 10 |
| Medial imbrication | 5 | 2 | 13 | 10 | 1 | 0 | 19 | 12 |
AKP – anterior knee pain; AF – arthrofibrosis.
Four patients were submitted to further procedures during the study period, as the secondary resurfacing had led to no improvement in symptoms (2 revision arthroplasties; 1 passive knee mobilization under anesthesia; 1 arthroscopic arthrolysis).
Complications
There were 2 surgery-related complications: a wound healing complication, with the need for debridement on 3 separate occasions (due to early removal of sutures) and a periprosthetic fracture of the patella, after a fall.
DISCUSSION
Over half of the patients submitted to secondary resurfacing of the patella benefitted from the procedure, with 65.2% revealing an improvement in pain symptoms. Although our hypothesis was rejected, this procedure may be an adjuvant solution to anterior knee pain and should be considered in the preoperative planning of revision surgery.
The results reflect current literature, which reports improvements in close to 50% of cases, with secondary resurfacing of the patella [3, 6-8], but our knowledge of indicators that would reliably identify those patients who may develop AKP and how best to treat them to avoid dissatisfaction remains deficient [2]. A recent study revealed improvements in knee scores in a similar percentage of cases, with a specific cause for anterior knee pain being unknown [16].
When considering subgroups, the under-70 year old patients with anterior knee pain after bicondylar knee replacement responded well to this form of treatment. Postoperative improvement in range of motion (60%) and improvement in pain (80%) led to patient satisfaction of 75% in this subgroup, providing a justified indication for this procedure.
Similarly, this indication may be applied to patients with arthrofibrosis, as a 53,8% improvement in range of motion and 62% improvement in pain symptoms was achieved in these patients. When reviewing current literature, a number of other procedures are mentioned, such as manipulation under anesthesia and aggressive physiotherapy, arthroscopic and open arthrolysis and revision arthroplasty [17, 18], with no apparent mention of secondary patella resurfacing.
In this study, secondary resurfacing of the patella revealed a low complication rate (2.2%) and a low rate of further procedures (10.9%).
Whether these patients improved from the secondary resurfacing itself, or from the associated soft-tissue procedures or both, remains to be seen, with further studies necessary to differentiate between the various techniques.
A sine qua non condition for the success of a secondary resurfacing is an accurate and well-fixed primary prosthesis, with correct ligament balance.
CONCLUSION
Although secondary resurfacing did not resolve the anterior knee pain in all patients, it is definitely an important procedure to keep in mind when revising a bicondylar arthroplasty. Further studies need to be done in order to provide improved screening for the origin of anterior knee pain and to evaluate the soft-tissue procedures in these cases.
ACKNOWLEDGEMENT
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article. No funds were received in support of this study.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflicts of interest.







