RESEARCH ARTICLE
Management of Extensor Tendon Injuries
M Griffin1, S Hindocha*, 2, 3, D Jordan3, M Saleh4, W Khan5
Article Information
Identifiers and Pagination:
Year: 2012Volume: 6
Issue: Suppl 1
First Page: 36
Last Page: 42
Publisher ID: TOORTHJ-6-36
DOI: 10.2174/1874325001206010036
Article History:
Received Date: 1/9/2011Revision Received Date: 22/10/2011
Acceptance Date: 27/10/2011
Electronic publication date: 23/2/2012
Collection year: 2012

open-access license: This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
Abstract
Extensor tendon injuries are very common injuries, which inappropriately treated can cause severe lasting impairment for the patient. Assessment and management of flexor tendon injuries has been widely reviewed, unlike extensor injuries. It is clear from the literature that extensor tendon repair should be undertaken immediately but the exact approach depends on the extensor zone. Zone I injuries otherwise known as mallet injuries are often closed and treated with immobilisaton and conservative management where possible. Zone II injuries are again conservatively managed with splinting. Closed Zone III or ‘boutonniere’ injuries are managed conservatively unless there is evidence of displaced avulsion fractures at the base of the middle phalanx, axial and lateral instability of the PIPJ associated with loss of active or passive extension of the joint or failed non-operative treatment. Open zone III injuries are often treated surgically unless splinting enable the tendons to come together. Zone V injuries, are human bites until proven otherwise requires primary tendon repair after irrigation. Zone VI injuries are close to the thin paratendon and thin subcutaneous tissue which strong core type sutures and then splinting should be placed in extension for 4-6 weeks. Complete lacerations to zone IV and VII involve surgical primary repair followed by 6 weeks of splinting in extension. Zone VIII require multiple figure of eight sutures to repair the muscle bellies and static immobilisation of the wrist in 45 degrees of extension. To date there is little literature documenting the quality of repairing extensor tendon injuries however loss of flexion due to extensor tendon shortening, loss of flexion and extension resulting from adhesions and weakened grip can occur after surgery. This review aims to provide a systematic examination method for assessing extensor injuries, presentation and management of all type of extensor tendon injuries as well as guidance on mobilisation pre and post surgery.
INTRODUCTION
The extensor tendons function to transmit tension from the muscle belly to the specific joint. Extensor tendons can be divided into intrinsic and extrinsic groups [1]. The instrinsic muscles are located within the hand itself, whereas the extrinsic muscles are located proximally in the forearm and insert onto the hand by long tendons [1]. The extensor muscles are all extrinsic tendons except for the interosseous-lumbrical complex [1]. The lumbrical muscles contribute to the flexion of the metacarpahlangeal joints and to the extension of the interphalangeal joints [1]. The interossei group form the lateral bands with the lumbricals and abduct and adduct the fingers [1]. All the extrinsic extensors are innervated by the radial nerve, which consist of 3 wrist extensors and a larger group of thumb and digit extensors 1. The extensor carpi radialis brevis (ERCB) is the main extensor of the wrist accompanied by extensor carp radialis longus (ECRL) and extensor carpi ulnaris (ECU) which provide radial and ulnar movement of the wrist repsectively.1The ECRB inserts at the base of the third metacarpal, the the ECRL at the base of the second metacarpal and ECU at the base of the fifth metacarpal [2]. The extensor digitorum communis, extensor indicis proprius and extensor digiti minimi extend the digits [2]. Each one of these muscles inserts at the base of the middle phalanges as central slips and to the base of the distal phalanges as lateral slips [2]. Extension of the thumb is carried out by the abductor pollicis longus, extensor pollicus longus and extensor pollicis [1]. An extensor retinaculum, a fibrous band prevents bowstringing of tendon at the wrist levels and separates the tendons into 6 compartments [1]. The extensor digitorum communis is a series of tendons to each it with a common muscle belly and with intertendinous bridges in between them [1]. The index and small finger also have extension function through the extensor indicis proprius and extensor digiti [1]. minimiThe first compartment contains the extensor pollicis brevis and the abductor pollicis longus; the second, the extensor carpi radialis longus and extensor carpi radialis brevis; the third, the extensor pollicis longus; the fourth, the four tendons of the extensor digitorum communis plus the extensor indicis proprius; the fifth, the extensor digiti quinti; and the sixth, the extensor carpi ulnaris [1].
EXTENSOR TENDON INJURIES
Extensor tendon injuries are more frequent than flexor tendon injuries [3]. and are very common (61%)[4] as they are not protected as well as the flexor tendons due to their superficial location and lack of overlying subcutaneous tissue. Extensor tendon injuries can cause serious functional impairment but have not received the attention in the literature as flexor tendon injuries [5]. To repair extensor tendons the surgeon needs the same skills as flexor tendon repair and is not a simple challenge, which is common misconception [6-8]. Lacerations of the extensor tendon system can occur at any site. Extensors are particularly difficult for surgeons because of their reduced size compared with the flexors and their lack of collagen-bundle linkage, which reduces the grip strength available for the suture material [9]. Also the flat tendon profile in zone I to IV increases the surface area between the repaired tendon and the adjacent tissue, particularly bone which makes it susceptible to adhesion formation. In addition, the cross section of the extensors changes from semicircular to bioconcave disk in zones I to IV making durable repair difficult because of thin but broad characteristics of the tendon [10].
PRESENTATION AND EXAMINATION OF EXTENSOR TENDON INJURIES
Taking a detailed history is important and knowing the mechanism of injury, position the finger was in during the injury, age, occupation and handiness as in other hand injury to plan treatment and management of extensor tendon injuries. The mechanism of injury is important for several reasons. Most lacerations of the dorsal aspect of the hand and fingers can be considered ‘clean’ but any contamination would need debridement, which needs to be discovered during the history. It is unusual for patients to always admit to being in fights, however knowing whether it is a human bit is necessary. Whether the patient thinks there may be a foreign body is also necessary as these foreign bodies may then be missed.
Physical examination needs to include systemic and in depth examination of both hands. The site of the laceration and the inability to extend a joint distal to it indicates that the extensor tendon may have been at least partially divided. If the extensor tendon is completely severed the finger may be resting in flexion. When testing function of the extensor muscle of the hand, extension must be against resistance as you will not pick up a partial laceration. Extension of the hand digits is performed by several muscles with their bodies in the forearm that continue to the dorsal aspect of the wrist and insert onto the digits. Extensor digiti minimi is responsible for extension of the fifth digit. It can be tested by asking the patient to lie their hand flat on a surface and hyperextend the fifth digit. The extensor digitorum tendons extend digits two through five. The hand can be laid flat again on a surface and the tendon of each finger tested by having the patient hyperextend the digits against resistance. Extension of the second finger is also performed by extensor indicis, which can be tested in a similar fashion to extensor digiti minimi. Extension of the first digit is controlled by two muscles, extensor pollicis longus and brevis. The path of these two tendons defines the “anatomical snuffbox” which contains the radial artery and the scaphoid bone of the wrist. Extension of the thumb at the interphalangeal joint and the metacarpophalangeal joint can be tested separately against resistance.
Sensation using two-point discrimination or the surgeon’s choice should be carried out to determine the radial nerve injury particularly if extensor tendon injury is suspected. However median and ulnar nerve should be tested also. Radiographs are needed to assess any associated fracture as they will need to fixed before tendon and nerve injuries during surgery. A human bit can cause metacarpal fractures. Glass and other foreign objects can also be picked up on x-ray.
Full extension of the digits at the individual small joint of the hand can be possible even after laceration. The extrinsic and intrinsic components of the extensor system can act solely independently. The distal IP joint finger extension can still be possible with complete severance of the main extrinsic extensor tendon at or proximal to the metacarphalageal joints. Furthermore oblique retinacular ligaments can results in weak distal extension through the tenodesis effect but this can fatigue and the extension lad can become obvious.
The extensor mechanism characteristically fails at the insertion of the central slip and the terminal tendon producing characteristic deformities including boutonniere and mallet. It must be remembers that mallet deformity does not always happen acutely making injuries to the central slip more difficult to identify. In addition mallet fingers can be complicated by extensor lag at the distal IPJ (DIPJ) but also the development of a ‘swan neck’ deformity as excess tension builds at the central slip insertion into the base of the middle phalanx.
REPAIR OF EXTENSOR INJURIES
Kleinert and Verdan wrote a classification system for extensor tendon lacerations according to the eight zones of the hand, wrist and forearm which as been widely accepted [11]. Verdan defined eight zones- four odd numbered zones overlying each of the joints and four even numbered zones overlying the intervening tendon segments, increasing from distal to proximal. The type of injury, surgical approach, potential deformity varies according to the zone [11]. Zone I refers to the area from the DIP joint to the fingertip; zone II encompasses the middle phalanx; zone III refers to the PIP joint; zone IV is over the proximal phalanx; zone V refers to the MP joint; zone VI encompasses the metacarpal and zone VII is over the wrist (see Fig. 1) [11]. Rockwell et al., [12]. Explained that treatment of tendon injuries is dependent on the location and type of injury. Repair should take place very soon after the injury especially within the first 2 weeks.
 |
Fig. (1). Zones of the extensor tendon muscles. |
Extensor tendon repair techniques are not as complicated in design and have much less tensile strength than flexor tendon repairs (Fig. 2). This is due to the extensor tendon being smaller with a relatively flat cross section. Its collagen is longitudinally orientated with little or no cross-linking. Due to the size differential and surrounding paratendon (except in zone VII) extensor tendons are not as capable of withstanding multiple-stranded, strong repair approaches especially in the distal zones.
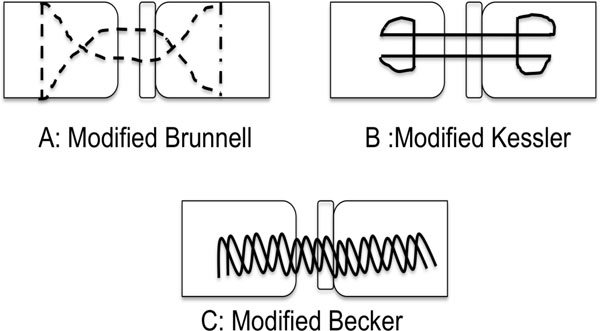 |
Fig. (2). Common extensor tendon repairs. |
Unfortunately only few studies have investigated the strength of extensor repairs. In a study by Howard et al., the four-strand repair by Howard et al., has been shown to be the strongest but not biomechanical features including shortening, loss of motion were not evaluated in this study and the strength was not evaluated as in other studies [13]. Compared with MGH or the traditional modified bunnel repair, two-strand locked bunnell repair has shown to be immediate in strength and evlauted further by Newport et al., [14]. In these studies locked bunnell improved quality of strength (suture rupture rather than pullout) over the traditional bunnell (17% versis 58% pullout) but less than the MGH repair (0% pullout), the four strand bunnell or Kracjkow-Thomas (0% pullout), described by Howard et al., [9]. But the strength and the quality of the repair compared to the traditional two-stranded technique differed in the smaller, thinner tendons of zone IV compared to repair in zone VI [9, 15].
The forces needed for extensor repair has not been studied in depth. Ketchum et al., investigated tension strength via a force transducer on the proximal phalanx finding that normal subjects could generate a force of 2.99kg for the index, which decreased ulnarly to 1.97kg for the small finger [16]. Animal models have illustrated that tendon shortening can affect how the extensor repair works by causing loss of composite flexion and increasing force required to obtain full flexion. Newport illustrated that the modified bunnell technique can produce an average of at least 7mm of shortening resulting in 35 degrees or more loss of composite flexion when the wrist is held in neutral position [9]. Minamikawa et al., [17]. Also showed there was a loss of 6.4 mm tendon over the metacarpal when the wrist was extended 45 degrees or more and recommend this could be amended if the wrist was appropriately extended. However, these are only animal studies and so further research is still needed as animal models cannot take into account muscle tone, friction of edema, adhesion formation, skin closure or bulk of repair.
ZONE I INJURIES
Zone I injury often referred to as mallet finger is when there is disruption to the extensor tendon over the distal interphalangeal joint causing a flexion deformity of the distal interphalangeal joint (see Fig. 3) [17]. It is often open but is more likely to be closed [17]. Forceful flexion of the distal interphalangeal joint in an extended digit is the most likely cause, which results in rupture of the extensor tendon or avulsion from its insertion at the distal phalanx. When left untreated hyperextension of the proximal interphalangeal joint may develop due to the retraction of the central band causing a swan neck deformity [18]. Mallet fingers are classified into 4 types:
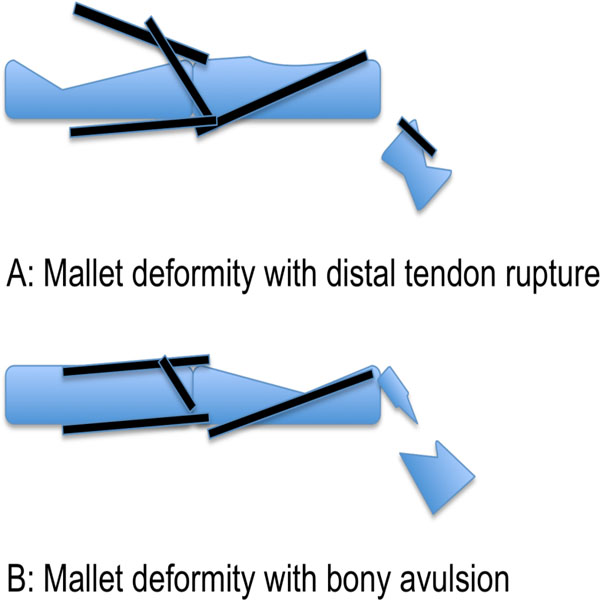 |
Fig. (3). Schematic diagram of mallet injuries. |
Type 1: Closed with or without avulsion fracture
Type 2: Laceration at or proximal to the distal interphalangeal joint with loss of tendon continuity
Type 3: Deep abrasion with loss of skin, subcutaneous cover, and tendon substance
Type 4: Transepiphyseal plate fracture in children; (B) hyperflexion injury with fracture of the articular surface of 20 to 50 percent; and (C) hyperextension injury with fracture of the articular surface usually greater than 50 percent and with early or late palmar subluxation of the distal phalanx.
Closed mallet fingers, which is type I fractures should be treated with an immobilisation splint in extension or slight hyperextension for 8 weeks, which included 2 weeks night splinting. The patient should understand the importance of keeping the finger extended for the entire 8 weeks. Exercises start by blocking exercises of the profundus involving the proximal interphalangeal joint active motion only. A Cochrane review documented that patient compliance was the most important factor in splint success [19]. A further Cochrane review found no evidence for difference in outcomes between splints [20]. After 8 weeks the fingers should be examined again and if active extension is present splinting can be reduced to high-risk times such as sleeping, manual work or athletic performance. Splinting can be successful even after 3 months of injury [21, 22]. Type II-IV fractures should be treated surgically. Type II required simple suture through the tendon alone or a roll type suture incorporating the tendon and skin in the same suture and then splinting for 6-8 weeks [23]. Type III fractures include loss of tendon substance which requires immediate soft tissue coverage and primary grafting or reconstruction with a free tendon graft [23]. Type IVA are best treated with closed reduction followed by splinting and are thee most likely fracture in children [23]. Type IV-B is usually treated by splinting for 6 weeks with 2 weeks of night splinting yields good results. Type IV-C with palmar subluxation of the distal phalanx is surgically managed with open reduction and internal fixation using a Kirschner wire and sometimes a pull-out wire or suture (Fig. 3). A splint for 6 weeks is then used after which the Kirschner wire is removed and motion started. The fracture fragment’s location is extremely important as proximally displaced fragment not in continuity with the distal phalanx may also require open reduction and internal fixation.
Chronic mallet finger is common because some patient accept the deformity and never see a surgeon for treatment. Splinting should be the first treatment for those presenting late. Even when the presentation is late and splinting is delayed several reports have shown beneficial outcomes. Surgery is then offered if conservative management has failed or patients present with recurrent chronic mallet deformities including immobilisation with transartilcular Kirschner wire fixation across the affected joint, fowler central sip release, excision of tendon scar unit and fixation in hyperextension. Amputation and distal interphalangeal joint arthrodesis are only salvage techniques [24-26].
ZONE II INJURY
Zone II injures or middle phalanx injuries are usually as a result of laceration or crush injuries rather than avulsion like zone I. If there is extensor lag on examination than exploration and repair is needed whereas if there active extension with only a degree of weakness than splinting can be used for 3-4 weeks. Injuries greater than 50% of the tendon should be repaired the tendon should be repaired with a fashion-of eight suture or similar fashion.
ZONE III INJURY
Zone III Injury otherwise known as boutonniere deformity is caused by disruption of the central slip at the proximal interphalangeal joint. Absent or weak active extension of the proximal interphalangeal joint is a positive finding [27]. Active extension is retained at first by the lateral bands but the head of the proximal phalanx eventually goes through the central slip resulting in migration of the lateral bands. This then results in loss of deformity with loss of extension at the proximal interphalangeal joint and hyperextension at the distal interphalangeal joint. The injury can be closed or open and the central slip may avulse with or without the bony fragment. The boutonniere deformity usually occurs 10-14 days after the first injury [8]. Closed deformities require splinting for 4-6 weeks of the PIPJ in extension with the DIPJ and wrist joints left free. Surgery should be implemented for closed fractures when (1) displaced avulsion fractures at the base of the middle phalanx (2) axial and lateral instability of the PIPJ associated with loss of active or passive extension of the joint and (3) failed non-operative treatment. Surgery entails passing a suture through the central tendon and securing it to the middle phalanx with or without the bony fragment. Kirschener wire fixation of the proximal interphalangeal joint is maintained for 10 to 14 days, followed by an extension splint until union. If primary repair is not possible than the lateral bands can be sutured in the dorsal midline of the finger to reconstruct the central slip and a flap can be raised from the proximal portion of the central slip to restore active extension. For open injuries, surgical repair might not be required if splinting is used as the tendon may come together. However, in a true boutonniere deformity, both central slip and lateral band injuries should be expected. In the elderly, the period of immobilization can be reduced to 2 weeks to aid the returning of full flexion.
ZONE IV INJURIES
Zone IV injuries or otherwise known as proximal phalanx injuries usually involve the broad extensor mechanism, usually partial and spare the lateral bands, being diagnosed usually by inspection [28]. Splinting the PIPJ in extension for 3-4 weeks without repair as shown to have the same outcome as repairing it with 50 nonabsorbale sutures [29]. However, if the laceration is complete surgical primary repair should be performed followed by 6 weeks of splinting in extension [30]. In the first 3 weeks volar positioning should be used with passive extension allowed. At week 4 gentle active extension is introduced but no passive flexion at this time. In the last two weeks active flexion is introduced and graded resisted exercises are implemented.
ZONE V INJURIES
Injuries in zone V are nearly always open and treated as human bites until examination proves otherwise. Primary tendon repair is needed after irrigation. The saggital bands should be repaired to prevent lateral migration of he extensor digtorum communis tendon and subsequent metacarpophalangeal extension loss [8, 29].
Splinting of the wrist in 30-45 degrees of extension and the metacarpophalangeal joint in 20-30 degrees of flexion is performed with the proximal interphalangeal joint free. If there is a human bite it should extended for inspection and debrided, irrigated and should be left open [30]. Cultures should be taken before irrigation and patients started on broad-spectrum antibiotics. The bit wound commonly heals within 5 to 10 days with secondary repair rarely being needed.
ZONE VI INJURIES
The tendons in this area are close to the thin paratendon and thin subcutaneous tissue. Injuries in this zone are situated in the dorsal hand may not always result in loss of the extension at the metacarpophalangeal joint. Surgical repair is needed with stronger core type sutures and then splinting should be placed in extension for 4-6 weeks. If the extensor digitorum communis is involved, all fingers should be splinted but if the proprius tendon is solely involved, only the affected finger need be splinted with the wrist [31]. Degloving injuries are no uncommon which require grafting or flaps. As the tendons in this area are larger stronger core suture should be used.
ZONE VII INJURIES
There is still debate whether releasing the retinaculum for visualization and repair is needed when injuries occur in this area as it may cause postoperative adhesions [32,33]. Some portion of the extensor retinaculum needs to be maintained to ensure avoid the tendon bowstringing [9]. The same routine for zone IV injuries can be used. If early dynamic splinting is used, adhesions are less likely. A four-strand suture has shown to be appropriate for zone VII injuries.
ZONE VIII INJURIES
In the dorsal forearm many tendons are likely to be lacerated, including the muscletendious junction and tendon bellies but thumb and wrist extension should be repaired first [34]. Multiple figure of eight sutures should be used to repair the muscle bellies. Static immobilisation of the wrist in 45 degrees of extension and metacarpophalangeal joints in 15-20 degrees should be maintained for 4-5 weeks [35].
THUMB INJURIES
Mallet injuries are uncommon in the thumb because the terminal extensor tendon is thicker on the thumb [36]. For open injuries most surgeons would recommend primary repair with splinting for 6 weeks. For closed injuries splinting for 6 weeks without surgical repair is a suitable alternative but surgical repair is also used [37]. The broad expansion of the metacarpophalangeal joint of the thumb makes laceration of all components in this area rare. Extensor pollicis brevis is are rare to be solely lacerated so its repair is debatable because extension of the metacarpophalangeal joint is possible with an intact extensor pollicis longus. Extensor pollicis longus injury causes extension lag in both metacarpophalangeal and interphalangeal joints and it should be repaired. Splinting is usually for 3 to 4 weeks, with the thumb metacarpophalangeal joint in full extension and wrist in 40 degrees of extension with slight radial deviation. For injuries in zone VI and VII the abductor pollicis longus retracts when divided and therefore requires to be released for successful repair [28]. Splinting is then needed for 4-5 weeks with the wrist in radial deviation and the thumb in maximal abduction [28].
REHABILITATION OF EXTENSOR INJURIES
The ultimate aim of any rehabilitation is to obtain healing with minimal gapping and prevent adhesions. Static mobilisation was the traditional method of postoperative rehabilitation but complications including tendon rupture, adhesion formation requiring tenolysis, extension lad, loss of flexion and decreased grip strength have all been documented [32,38-40].
Early mobilisation has been introduced for flexor tendon injuries because it decreases adhesions and subsequent contractures. Furthermore mobilisation has shown to enhance DNA synthesis at the repair site, improve tensile strength and increase vascularity [41-43]. It has now shown to be more useful in certain areas for extensor injuries as well [44]. Mowlavi et al., studied early controlled mobilisation versus static splinting for zone V and zone VI [45]. Functional outcomes at 4,6 and 8 weeks were improved after dynamic compared to static splinting [45]. However unfortunately the outcomes were not improved after 6 months [45]. The authors recommended that dynamic splinting should be available for those who are motivated to return early to functional capacity. Bulstrode et al., similarly found that ROM for the early mobilisation group at 6 weeks postoperatively was greater than static mobilisation but disappeared at 12 weeks [46]. Grip strength was also assessed at 12 weeks postoperatively [46]. The difference in grip strength was significantly greater in the early-mobilised group and to uninjured hand compared to the immobilised and uninjured hand [46]. Russell et al., also compared immobilisation with early controlled mobilisation but in contrast found no significant difference between the groups [47].
Early mobilisation rehabilitation programmes can be in two categories (1) early active mobilisation and (2) early controlled mobilization using a dynamic splint. Early controlled motion with a dynamic extensor splint has been found to decrease adhesions and subsequent contractures. Only two randomized controlled trial studies have compared early mobilisation versus early active mobilisation. Chester et al., looked at extensor injuries from zone IV to VIII and found significantly better ROM in the patient group treated with early controlled mobilisation compared to early active mobilisation at 4 weeks [48]. However, Khandwala compared early active mobilisation with early controlled mobilisation in zone V and VI and found no difference in total active motion at 4 or 8 weeks postoperatively [49]. Therefore, it is clear that few studies have tried to evaluate the specific mobilisation regime that has the best functional outcome. Furthermore a recent review confirmed that short-term evidence shows early controlled mobilisation is superior over immobilisation for extensor tendons but no conclusive evidence is found regarding the long-term effectiveness of the different rehabilitation programmes [50]. In addition, this study highlighted that there is wide variety in duration, splinting technique and frequency and force intensity of exercises used for rehabilitation, further illustrating that further studies are needed. Evaluating the cost-effectiveness of the regimes dynamic splinting is more expensive and requires more hand therapist input and this is why some authors prefer early active mobilisation for the proximal zone injuries [51, 52]. The patient needs to be very cooperative and the hand therapist needs to monitor carefully in postoperative rehabilitations. Therefore a team approach needs to be made with rehabilitation tailored to the individual adjusting management as they go along.
COMPLICATIONS
To date there is little literature documenting the quality of repairing extensor tendon injuries. Complications can occur after extensor tendon repair including, loss of flexion due to extensor tendon shortening, loss of flexion and extension resulting from adhesions and patients can notice a weakened grip. When the extensor tendon becomes shortened or adherent, tenodesis restraint can occur. Flexion of the digit at the metacarpophalangeal joint causes extension force at the proximal interphalangeal joint when the metacarpophalangeal joint is flexed. Hand therapy should be started and focus on extrinsic excursion exercises and splinting should be started immediately. If there is no improvement following 6-month trials of conservative management then surgery may be needed. Tenolysis has shown to be appropriate when tenodesis occurs as a result of scarring with no significant loss of tendon length. Furthermore if the tendon is shortened, Littler’s technique of extensor tendon release can also be used [53]. Eggli et al., evaluated the outcomes of 23 patients after tenolysis and found that on average of follow-up of 5 years significant improvement was in 88% of the digits in extensor and flexor injuries in zone II. Extensor tenolysis was found to be a safe procedure [54].
Zone VII and VIII can be complicated by multiple tendon lacerations and decreased wrist mobility. Zone V complications can be complicated by infection from human bites. Zone I, II and III can be complicated by deformities that have occurred as discussed previously. Newport et al., [32]. Retrospectively analysed 62 patients with 101 extensor tendon injuries and found that patient without associated injuries achieved 64% good/excellent results and total active motion of 212 degrees which was statistically significant. Distal zones (I to IV) had poorer results than proximal zones (V to VIII). The percentage of fingers losing flexion was greater than those losing extension as well as the actual degree of loss. This study illustrated that the loss of flexion was more significant complication from extensor tendon injuries than originally thought. However techniques and the optimal rehabilitation methods to prevent complications as not been investigated.
Staged extension tendon repair is an option for failed primary repair and involved tendon reconstruction using a silicone implant. Small skin incisions are made over the dorsum of the finger. A silicone rod is place along the pretendious fascia to make a premade tunnel; this rod will help provide extension through elastic recoil of the rod. Soft tissue defects are managed by split thickness skin grafts or by secondary intention. Once the soft tissues are healed, the silicone rod is exchanged for a tendon graft. Adams used this technique in 6 fingers to restore proximal joint extension with severe injuries to the dorsal skin and extensor mechanism restoring active extension of all proximal interphalangeal joints and recommending it as a reliable alternative for severely injured fingers with extensor mechanism loss [55].
CONCLUSION
We have given an overview of the management of extensor tendon injuries and rehabilitation methods. It is clear that the literature has not focused on extensor tendon injuries to the extent as flexor tendon injuries. Post rehabilitation methods have been researched and it is clear that mobilisation techniques are more favoured but we can expect more research in this area. The surgical approach to each zone has not been fully researched with very few papers looking at the outcomes of different approaches. In an era of evidence based practice more research needs to work out the optimal approach to extensor tendon injuries and rate of complications after different approaches.
CONFLICT OF INTEREST
None declared.
ACKNOWLEDGEMENT
None declared.







