All published articles of this journal are available on ScienceDirect.
Treating Stiffness After Total Knee Arthroplasty: A Technical Note and Preliminary Results
Abstract
Total Knee Replacement is used to treat pain, stiffness and reduced range of movement. It has been estimated that a minimum of 90 degrees of range of motion in the knee is required for normal activities of daily living. In this article we demonstrate a technical note with a small patient series about the methods of treating knee stiffness after Total Knee Replacement.
INTRODUCTION
Total knee arthroplasty is performed to provide pain relief, joint stability and a satisfactory range of motion. It has been estimated that a minimum of 90° of range of motion in the knee is required for activities of daily living. 65° of knee flexion is required in the swing phase of normal gait and 106° of flexion is needed to arise from a chair easily or tie shoe laces [1].
Disabling stiffness after total knee arthroplasty (TKA) is rare, but can be devastating for the patient. Most patients complain of pain and diminished function associated with the stiffness. The true prevalence is unclear due to the lack of an established definition [2]. Several studies have attempted to define factors that have significant effect on range of motion (ROM) after TKA and most have shown that preoperative ROM is the principal predictive factor of postoperative ROM [3, 4]. Other factors include removal of posterior osteophytes and release of the deep medial collateral ligament in patients with large preoperative varus alignment [3].
Extrinsic sources of knee stiffness must be excluded (e.g. osteoarthritis of the ipsilateral knee, neurological injury leading to muscle rigidity or heterotopic ossification). When such problems exist, revision surgery is unlikely to be successful until they have been addressed.
With the exclusion of extrinsic aetiologies, the objective is to identify specific intrinsic causes that are amenable to surgery (see Table 1) [5]. Of these, arthrofibrosis is one of the most unresponsive causes. Arthrofibrosis is an abnormal proliferation of fibrous tissue in and around a joint that can lead to loss of motion. It is thought to result from pathological tissue hyperplasia following injury or surgery to the knee [6]. The knee is particularly vulnerable and widespread fibrous tissue can lead to altered knee biomechanics. Care needs to be taken when patients are on warfarin after TKA as the relative risk of developing stiffness due to arthrofibrosis postoperatively is 3.7 times greater than in unwarfarinised patients [7].
Intrinsic Causes of Knee Stiffness
|
PATIENTS AND METHODS
Patients
Between 1996 and 2005 the senior author has performed 568 total knee arthroplasties (TKAs). Of these, 3 patients developed stiffness following surgery that was debilitating. All patients had pain and restricted flexion to less than 60 degrees with full extension. The main symptoms were knee pain located laterally on mobilisation that was affecting daily activities.
Surgical Technique
As all the patients had a vertical incision, the old scar was incised. This was deepened down to the level of the subcutaneous tissue and with a combination of blunt and sharp dissection the medial flap was raised to expose the medial parapatella retinaculum, the vastus medialis obliqus (VMO) and the quadriceps tendon. The lateral flap was elevated to expose the patella as well as the attachment of the vastus lateralis (VL) to the quadriceps tendon. A medial para-patellar incision was used (Fig. 1) and this was deepened down to the level of the knee joint to evert the patella. The original eversion of the patella was not easy in all the patients and a quadricepsplasty (Modified Coonse-Adams flap) [8] was used to evert the patella (see Fig. 2). Further careful eversion of the patella was done with the help of a combination of blunt and sharp dissection at the level of the attachment of the patella tendon to the tibia. The knee was then carefully flexed with much of the eversion taking place at the quadriceps back snip.
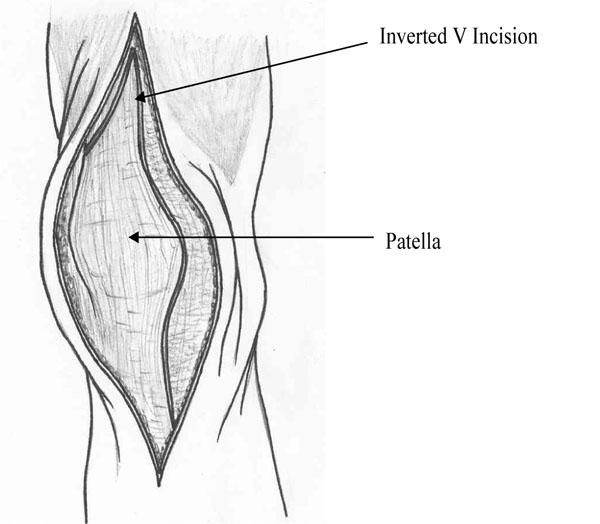
Initial incision into the joint consists of routine median para-patellar approach.
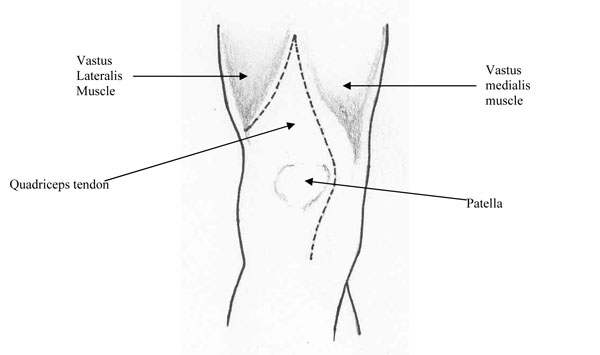
Lateral limb of incision into quadriceps tendon is carried distally and laterally, detaching vastus lateralis muscle.
The surgical scar around the knee replacement was released and the adhesions that had formed in the medial para-patellar gutter and the lateral part of the para-patellar gutter was released with a knife or diathermy to restore the normal anatomy. Dense scar tissue was commonly found around the patella button and carefully preserving the patella button, the dense scar tissue was removed.
A common consistent feature was the presence of adhesions along the lower pole of the patella to the attachment of the patella tendon. Careful dissection of the patella tendon and the fat pad was done from this band of scar tissue. Very often this scar tissue extended from the anterior aspect of the knees to the lateral aspect of the knee joint.
The scar tissue was carefully excised whilst preserving the normal anatomy. Once this central part of the scar tissue was removed, further scar tissue extending on the lateral side which was often the cause of tethering on the lateral side was also carefully excised. This was done with the help of diathermy as well as sharp dissection. Very often the denser scar tissue was found immediately lateral to the patellar tendon and extending to the prosthesis on the lateral side. Once this tissue was freed the extensor mechanism felt much more mobile. In view of the tightness in flexion the Posterior Cruciate Ligament (PCL) was excised in all patients as a part of the procedure and the intercondylar notch was cleared of fibrous tissue.
The attachment of the medial para-patellar retinaculum to the tibia was also carefully elevated to free the anteromedial aspect of the tibia. This was down to the level of the original medial collateral ligament. In one of the patients, the polyethylene was exchanged, but in the other two patients there was no exchange of the component.
If there was any inadvertent damage to the polyethylene we performed exchange of the polyethylene component. Once the major anterior soft tissues had been excised flexion was quite easily possible to 110°-120°. This was the same amount of flexion that was achievable prior to closure of the wound when the original surgery was done. Once the anterior, medial and lateral soft tissues had been excised and released, the scar tissue adjacent to the prosthesis was excised.
At this point, the tourniquet was released and haemostasis was achieved. The wound was then closed with the knee held in 110-120° of flexion. Once it was established that this degree of knee flexion was possible with the knee in this position, a vicryl suture was then applied to the apex of the V, which was then sutured to the VMO attachment to the quadriceps tendon. Further sutures were then carefully applied to convert the V into a Y to give the overall lengthening of the extensor mechanism between 1-1.5cm (Fig. 3). The rest of the wound was then closed using interrupted vicryl sutures for the medial para-patellar incision and then a continuous vicryl suture was applied to produce a complete closure of the para-patellar incision and the quadriceps tendon. No drains were inserted and with the knee held in 100-110° of flexion, the sub-cutaneous tissue was then closed and finally the skin using staples.
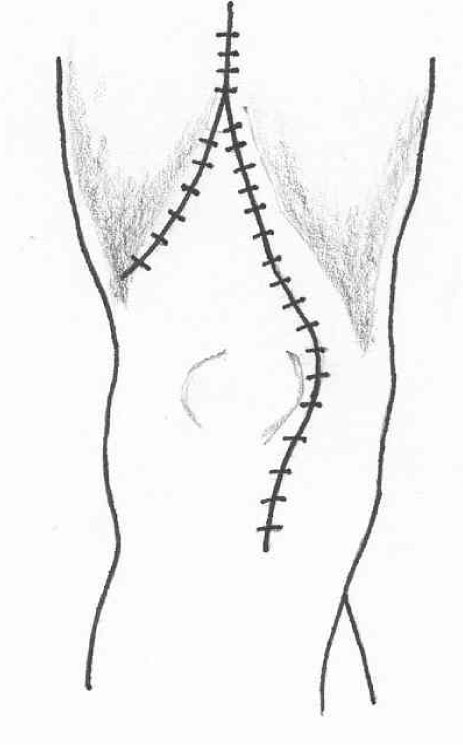
Conversion of V into Y Quadricepsplasty.
Salient points of the surgical technique were: -
- VY-plasty of the quadriceps tendon;
- Excision of surgical scar in the patellar tendon area and lateral to the prosthesis;
- Complete opening of medial and lateral para-patellar gutters to restore the normal anatomy;
- Excision of dense scar tissue around the patellar button with its extension into the patellar tendon area as well as freeing of the entire lateral side of the para-patella gutter and associated scar tissue next to the prosthesis, especially on the lateral side;
- Excision of the PCL despite the prosthesis being a cruciate-retaining prosthesis in all the three patients mentioned in this paper.
Post – Operative Management
The knee was rehabilitated as a primary TKA with no restraints on weight bearing or quadriceps activity. Continuous passive motion (CPM) was not used post surgery. All patients had out-patient physiotherapy after discharge for six weeks.
RESULTS
There were 2 females (aged 62 and 84) and one male (age 59). The mean interval between the primary and secondary surgery was 17.7 months (range 14 to 20). A summary of the procedure and range of motion for each patient is summarised in Table 2. The mean increase in flexion after revision surgery was 60 degrees (55, 60, and 65) with all patients reporting an improvement in pain, mobility, and activities of daily living.
Individual Patient History
| Age/Gender | Mean Interval to 2°Surgery (Months) | Procedure | Length of Follow Up (Months) | Pre-Op Flexion | Post-Op Flexion | Knee Pain |
|---|---|---|---|---|---|---|
| 62/F | 19 | V-Y plasty, excision PCL, change of insert | 13 | 45° | 110° | Improved |
| 59/M | 14 | V-Y plasty, excision PCL | 9 | 40° | 100° | Improved |
| 84/F | 20 | V-Y plasty, lateral release, excision PCL | 11 | 55° | 110° | Greatly improved |
DISCUSSION
Though there is no consensus about timing, manipulation under anaesthesia is usually the first step in the management of stiff TKA [1, 2, 6, 7]. This procedure is usually undertaken within 2 months of primary surgery. If ROM does not improve or even regress and all other intrinsic causes of stiffness have been excluded, then several operative options are available but there is no established operation for an arthrofibrotic stiff knee following TKA. Yercan et al. [2]. performed secondary surgery on 10 patients (3 arthroscopic debridements, 5 open arthrolysis and 2 component revisions). In the arthrotomy group, the ROM improved from a mean of 66 degrees preoperatively to 107 degrees (an improvement of 41 degrees) postoperatively. This group also included 2 patients that had patellar “clunk syndrome”. If these were excluded from this group then simple arthrolysis resulting in improved ROM resulted in only one of three patients. These results are supported in another study in which seven knees with stiffness post TKA were treated with arthrolysis and conversion to a thinner tibial polyethylene insert [9]. Two knees required revision for aseptic loosening and infection. All five of the remaining knees were painful and stiff (four severely painful) at the time of final follow up. Our results compare favourably with these two studies. All three of our patients reported a marked improvement in pain whilst also maintaining a mean increase in flexion of 60 degrees. We believe that lengthening the extensor mechanism by performing the V to Y quadricepsplasty is the main reason for the difference in results.
In Papagelopoulos’s series of 42 stiff knees following TKA, quadricepsplasty combined with arthrolysis was performed in 6 cases of severe joint ankylosis. In 3 cases the Judet quadricepsplasty technique was performed and in 2 the modified Coonse and Adams quadricepsplasty [1]. Though no further operative treatment was performed, the average range of motion at last follow up was only 55° (range 20°-80°). Furthermore, in this series intra-articular arthrolysis was performed in a separate cohort of 18 knees. In all cases although there was an initial increase in ROM, this was not consistently maintained. This paper highlights the point that simple arthrolysis does not result in good functional outcome in the long term. The mean range of motion in our series improved from 46.7° to 106.7°. This is a substantial difference compared to Papagelopoulos’s series and this could be due to the fact that all 3 patients in our study had excision of the PCL and in one patient the polyethylene insert was changed to a thinner component. This patient had the greatest increase in flexion and ROM.
The use of quadricepsplasty to increase knee flexion is not a new concept. Nicoll [8] and Thompson [10] described a technique (which leaves most of the quadriceps mechanism detached from the patella) and reported satisfactory results following femoral shaft fractures. Judet’s treatment for quadriceps contracture involved detaching the vastus lateralis and medialis from the entire length of the femur [11]. A more recent study has confirmed the effectiveness of this procedure in native stiff knees following trauma [12]. These techniques are not easily applicable to patients with total knee replacements, where the primary surgical site is at the knee, and where an intact extensor mechanism with a sealed joint is desirable. However, a modified V-Y quadricepsplasty procedure has been described to facilitate greater exposure during total knee replacement in the ankylosed knee [11]. In Scott et al.’s series of 7 patients using the same technique, the average improvement in flexion was 49 degrees [11]. Our mean increase in flexion was 60 degrees and though a different cohort of patients, compares favourably with their study.
In Garvin’s case series of 16 patients, the quadriceps snip was used to assist in the surgical exposure of the knee [13]. This technique is essentially a modification of Coonse and Adams operative approach to the stiff, ankylosed or revised knee joint. Eight patients had previous knee prostheses and were undergoing revision surgery for aseptic loosening. The range of motion was increased by 30 degrees on average, though there was significant weakness in extension of the knee when compared with the contralateral side. Our results are more promising with respect to improving knee flexion whilst maintaining extension.
Rodriguez Blanco et al. reported an endoscopic quadricepsplasty technique in 26 patients suffering from knee stiffness from a variety of causes (4 of which were post operative) [14]. Their intra- and extra-articular techniques resulted in 65% of patients gaining at least 70 degrees of flexion at 3 months follow up. This is similar to our findings in which the mean improvement in flexion (at a minimum follow up of 3 months) was 60 degrees.
To our knowledge, the detailed technique we present here has not been reported previously with regards to improving knee stiffness post total knee replacement.
The value of the procedure described in relieving stiffness is that revision surgery (a major procedure with serious complications) is not required. This is the only known soft tissue procedure described for stiffness after total knee replacement. Previously simple arthrolysis with or without change of tibial insert has met with limited success [2, 9].
When a posterior cruciate ligament – preserving knee design is utilised, limited flexion may result if the PCL is too tight. Williams et al. reported an average increase in flexion of 40.1 degrees after arthroscopic release of the PCL in such patients [15]. Although all 9 patients reported subjective improvements in pain and stiffness, two eventually required revision arthroplasty. This highlights the importance of performing other soft tissue procedures as well as a PCL release. In all our patients the PCL was excised to further increase flexion and we recommend this as part of the soft tissue procedure, particularly if a PCL retaining prosthesis was used initially. It is necessary to ensure that the soft tissue balance of the TKA is correct otherwise sacrificing the PCL (which leads to an increase in flexion gap) may lead to subluxation or even dislocation of a posterior-stabilised prosthesis [16].
Although all three patients clearly stated a subjective improvement in pain and function as well improvement in knee flexion following this procedure we were unable to demonstrate this objectively as none of the patients had pre-operative functional knee scores.
In conclusion we describe an operation in which a V-Y quadricepsplasty was combined with a defined soft tissue procedure in order to relieve stiffness following total knee arthroplasty. The main indications are pain, functional limitation and stiffness. Additionally, extrinsic sources of knee stiffness should be excluded before performing this procedure and if the aetiology is solely arthrofibrosis then a more favourable outcome is likely to occur (Fig. 4).
ACKNOWLEDGEMENTS
We would like to thank Dr. R. Jaiswal (rsehda@doctors. org.uk) for the illustrations and schematic drawings.
CONFLICTS OF INTEREST
The authors did not receive grants or outside funding in support of their research or preparation of this manuscript. They did not receive payments or any other benefits from a commercial entity. There are no conflicts of interest.



