All published articles of this journal are available on ScienceDirect.
Importance of Preoperative Imaging in Acetabular Revision Surgery - A Case Report
Abstract
Acetabular defects, particularly as a result of protrusion of acetabular components into the hemipelvis, may cause serious complications during revision procedures as a result of iatrogenic injury to surrounding anatomical structures. In these challenging cases, we advocate the utilisation of preoperative three dimensional imaging. MRI and CT- imaging offer superior understanding of the three-dimensional quality of bony defects and the relationship of implants to important anatomical structures. Appropriate preoperative planning may also prevent major complications during the removal of the pre-existing hardware, prior to re-implantation of implants. Potential complications include injury of nerves, blood vessels and other intrapelvic structures.
In our case, a major bony defect of the acetabulum was a result of the protrusion of an implanted reinforcement ring. A preoperative, contrast-enhanced CT scan showed that the urethra was in close proximity to the hook of the reinforcement ring.
The preoperative imaging aided in identifying and understanding the potential complications that could occur intraoperatively. Additionally, it delineated the intact anatomic structures prior to surgery, which could have medico-legal implications.
The importance of preoperative imaging and the existing literature is discussed within this case description.
INTRODUCTION
Preoperative imaging and adequate planning should be the standard in primary hip and knee arthroplasty procedures. Modern imaging technologies can give the operating surgeon an improved preoperative understanding of the anatomical findings [1-3].
Planning of the procedure should then be easier and appropriate reconstructive implants and augments can be ordered. This may be more imperative in the evaluation of complex three-dimensional anatomic areas, like the acetabulum, where plain radiography does not clearly depict the complexity of osseous destruction.
In cases where the acetabular defect causes a protrusion of the cup into the hemipelvis, serious complications may arise during the revision procedure. Some intrapelvic complications have been described. These may occur primarily during the time of removal of migrated components or by placing cage screws [4-6].
The most commonly described complications are sciatic, femoral and obturator nerve palsies and haematomas secondary to serious arterial injuries [1, 4, 7, 8].
In this manuscript we underline the importance of preoperative imaging and we will provide information gained from three-dimensional preoperative imaging in cases were components were medial to Köhler’s line (teardrop line).. Moreover, this report points out that in addition to blood vessels and nerves, other structures, in this case, the urethra (ureter), may cause serious complications in hip revision surgery.
CASE REPORT
A sixty-nine-year-old woman underwent a primary total hip arthroplasty of the left hip for primary degenerative osteoarthritis at another institution. Subsequently, she developed isolated loosening of the cup and associated bone loss 8 years after the index procedure was performed. She underwent revision surgery, which entailed the implantation of a reinforcement acetabular reconstruction cage (Ganz ring). Postoperatively, the patient remained symptomatic complaining of residual pain after the revision procedure. She was referred to our institution 6 years after the revision procedure with increasing pain particularly with weight bearing and with a reduced range of movement. Mobility was only possible with the aid of two-forearm-crutches with an inability to weight bear on the left side.
On examination, there was a leg length discrepancy of 2 cm with the left leg shorter than the right, with an inability to perform a single leg stance. Preoperative range of motion of the left hip was limited to -0-100º of flexion, abduction/adduction was limited to 20-0-10º, and internal/external rotation was 20-0-15º. Clinically, there was localised tenderness noted on axial compression in the groin.
Plain radiographs demonstrated the protrusion of the reinforcement ring into the pelvis and complete migration of the anchoring hook into the pelvis with close proximity to the anatomic structures and other major soft tissue structures. There was no evidence of stem loosening or migration noted (Figs. 1, 2). Based on these findings and particularly the position of the anchoring hook and close proximity to intrapelvic structures, a CT scan was performed (Fig. 3).

Pelvis AP identifying the migration of the reinforcement hook into the pelvis.

Lateral view preoperative.
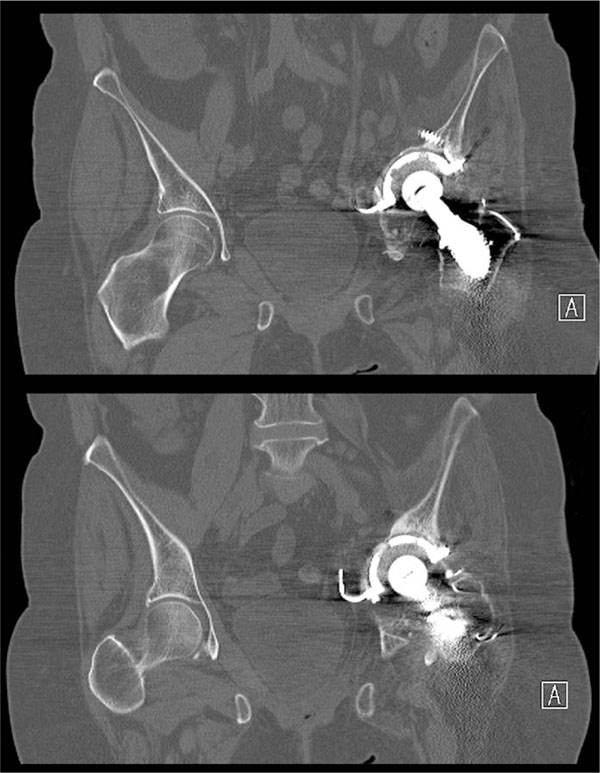
Conventional CT scan preoperatively without contrast agent.
The initial conventional CT-scan revealed the close proximity of the anchoring hook to the urethra, consequently a continuative contrast agent based CT scan was performed. which demonstrated the urethra looped around the hook of the reinforcement ring. No other relevant soft tissue encroachment was noted and an appropriate pre-operative plan was performed accordingly (Figs. 4, 5).
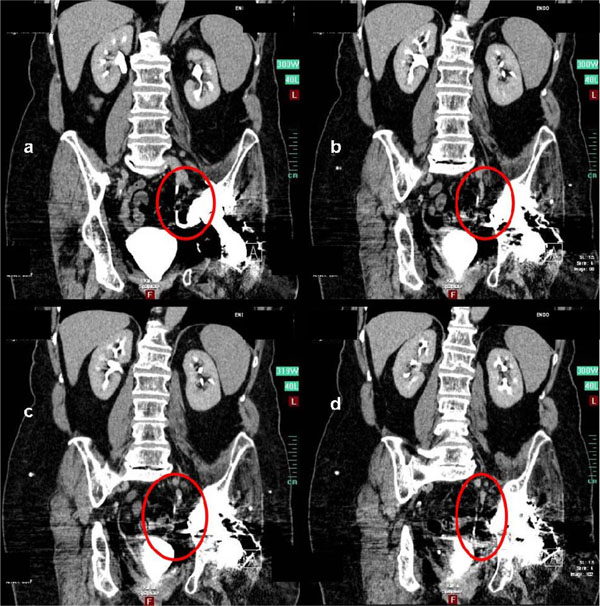
(a-d) CT with contrast agent which clearly identifies the anatomic relation between the hook and the urether within the contrast flow.

A further 3-D reconstruction and scrolling throughout all slices allows the surgeon to clearly rule out a complete bracing of the hook around the urether.
Through a posterior approach, the complete reinforcement ring was safely retrieved, with particular attention paid to identifying the hook and careful dissection of the surrounding soft tissues performed. Intra-operative findings confirmed that the reinforcement ring had protruded into the pelvis. A large osseous defect was noted in the acetabulum which required further fixation and stabilisation utilising a larger complete reinforcement ring and additional five screws into the ileum were placed. The osseous defect was addressed with a combination of structural allograft and impaction bone grafting. Finally, an all-polyethylene acetabular cup was cemented into place. Leg lengths and soft tissue tensioning was restored using an additional long neck and off set variation (Fig. 6).

Pelvis AP final result with a complete reinforcement ring and combined allograft impaction grafting to stabilise the all-polyethylene cup.
At 24 months follow-up, the patient was doing well, pain free and walking unaided. The patient had no further complications and the Harris Hip Scores had improved from 38 preoperatively to 80 post operatively.
DISCUSSION
Pelvic structures are prone to injury during revision hip surgery [1, 4, 6-8]. Preoperative identification of patients at risk for vascular and nerve injury during these procedures can be performed using plain radiography, angiography, CT or MRI scans.
In this case report, we demonstrate the close proximity of the acetabular metalware to relevant anatomical structures. This is especially true in complex revision procedures that include fixation screws and anchoring hooks, which can easily protrude into the pelvis. Damage to the urethra is a relatively rare but possible complication that can occur in revision procedures. In order to have a greater preoperative understanding and subsequently prevent serious injuries, a CT or MRI scan should be performed preoperatively [5].
Hollis G. at al describe a significant increase in the utilization of MR imaging in the evaluation of complications related to total hip arthroplasty. This is because of the ability to image periarticular soft tissues including muscle, tendon, and neurovascular structures, combined with the ability to limit the prosthesis-induced artefact. The absence of ionizing radiation is another advantage of MRI over CT scanning [9, 10].
Most urological injuries encountered by orthopaedic surgeons are associated with pelvic trauma. Acute injuries to the bladder, prostate, and urethra may occur in association with 13.5% to 46.6% of pelvic fractures [11].
There are no publications to date that describe a direct urethral injury caused during revision hip surgery. Components that are medial to Köhler’s line on plain radiography, require additional evaluation. A CT or MRI scan usually reveals the proximity of major structures, like the urethra, and it also provide valuable information regarding the appropriate placement of bone graft, cement, screws and finally the acetabular components [6].
Another advantage of preoperative CT-scans is the possibility to generate 3-dimensional models so that a better understanding of the acetabular anatomy is possible. With this information, the need for custom made implants or cages can also be performed [12].
A relative disadvantage of CT and MRI scans are implant related metal artefacts. Most studies show that these artefacts can be significantly reduced with proper parameter modifications and/or the use of specially designed software [13].
The same applies to modern MRI sequences; the musculoskeletal radiologist can alter the technical imaging parameters in the setting of orthopaedic implants, producing diagnostic images for the evaluation of the regional osseous and soft tissue structures [9, 14].
The two-dimensional nature of radiographs limits their ability to accurately determine component alignment, such as the true version of the acetabular component in total hip arthroplasty especially when patients are not properly positioned. CT has been proven to be more reliable than radiographic analysis for intraoperative estimation of component alignment, providing a direct three-dimensional evaluation of cup version in total hip arthroplasty [14-16, 18, 19].
In cases in which the stem has to be revised, a CT-scan offers additional information concerning the geometry of the femoral bone which aids in optimising the implant size [17].
We believe that in severe cases of component migration in hip arthroplasty, a preoperative CT or MR examination can give important information about the relationship of implants to intrapelvic structures. With modern CT technology, the radiation exposure seems justifiable. The per-patient costs are also relatively low [17].
However MR imaging has no radiation exposure but relatively high per-patient costs.
In conclusion we recommend the use of a distinct modern multiplanar imaging technique in cases of unclear protrusion of the hardware into the pelvis because CT and MRI scans are accurate and cost effective to justify regular use in preoperative planning.
CONFLICT OF INTEREST
Declared none.
ACKNOWLEDGEMENTS
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article. No funds were received in support of this study.


