All published articles of this journal are available on ScienceDirect.
Minimally Invasive Helical Plating for Shaft of Humerus Fractures: Technique and Outcome
Abstract
Introduction:
The humerus is subjected to substantial amount of torsional stress. Conventional plating may not address this sufficiently and may lead to fixation failure or non-union. A helical plate may offer the solution. We present the surgical technique and functional outcome of 5 cases of humeral shaft fractures treated with this technique in a minimally invasive way.
Materials and Methods:
The operations were performed between 2004 and 2010, by three surgeons. All the patients had closed humeral shaft fractures, either simple transverse or with mild comminution. Two small incisions were made. The proximal incision was placed along the deltopectoral groove over the shaft, and the distal incision was placed as in an antero-lateral approach. The radial nerve was identified and protected. A pre-selected plate was contoured and introduced in the submuscular plane. The plate was placed in a proximal-lateral and distal-anterior position. Screws were inserted through stab incisions. The patients were followed for an average of 6 months. Functional recovery of the shoulder and elbow was assessed using the Constant and Mayo elbow performance score systems.
Results:
All incisions healed by first intention without complications and all the fractures went on to unite. All patients achieved good to excellent shoulder and elbow function.
Conclusion:
The helical plate technique is a safe and effective method of treating humeral shaft fractures and has good functional outcome.
INTRODUCTION
Shaft of the humerus fractures are common in an orthopaedic practice. Most of them can be treated effectively by conservative means [1, 2]. When surgery is required, intramedullary nails or plates may be used, depending on the fracture pattern. Open plating allows anatomical reduction of fractures without affecting elbow and shoulder function [3, 4] but involves extensive soft tissue stripping, which increases the risk of non-union and radial nerve palsies [5-7]. Minimally invasive plate osteosynthesis (MIPO) techniques have been used to minimize soft tissue dissection and injury to the radial nerve. It has been reported that humeral shaft fractures can be successfully treated with MIPO technique, while having lower complication rates than conventional open plating [8, 15-18].
The position of the plate varies with different minimally invasive techniques. Lau et al. had treated proximal humerus or proximal humeral shaft fractures with lateral plating [9]. Anterior plating has also been used with success in the treatment of middle and distal humeral shaft fractures [8].
Lateral plating requires the development of a submuscular plane underneath the deltoid muscles, which violates the deltoid fibers inserting into the lateral part of the humeral shaft. The distal incision is also limited by the radial nerve, which winds around the lateral border of the humerus. Anterior plating may not be suitable for the fixation of proximal shaft fractures as plate position is hindered by the bicipital groove and biceps tendon.
Helical plating addresses these problems as the proximal part of the plate sits on the lateral part of the humerus. The distal part of the plate lies on the anterior surface of the humeral shaft, thus avoiding the deltoid insertion. This technique is suitable for the fixation of fractures involving various parts of the humeral shaft. This is a retrospective study to evaluate the technique and outcomes of patients with shaft of humerus fractures treated with minimally invasive helical plate technique.
MATERIALS AND METHODS
We included all adult patients that had displaced shaft of humerus fractures treated using the MIPO helical plate technique from December 2004 to January 2010. Open fractures, pathological fractures and fractures extending beyond the shaft were excluded. Patients who underwent non-helical plating and those with pre-existing nerve injury were excluded as well. The surgeries were performed by 3 surgeons and the choice of plate was based on the surgeon’s decision. These patients were followed up regularly in the clinic with X-rays and clinical examination. The range of motion of the shoulder and elbow of each patient were recorded by the attending surgeon.
Surgical Technique
The patients were in supine position with the operated arm on a radiolucent table. All patients underwent general anaesthesia. 2 small incisions were made. The proximal incision was made along the deltopectoral groove over the shaft. Care was taken to avoid injury to the axillary nerve, which winds around the humeral shaft about 5cm from the lateral edge of the acromion. The distal incision was made in the groove between the biceps and the brachioradialis muscle, at about 8cm proximal to the lateral epicondyle, placing it over the radial nerve near the lateral border of the humerus. Intermuscular dissection was similar to that of the antero-lateral approach to the humerus. Careful dissection was performed to identify and protect the radial nerve.
The plate was selected, contoured into a helix and inserted in a proximal to distal direction under the guidance of the image intensifier. 4.5mm reconstruction plate (Synthes, West Chester, USA), 4.5mm Limited Contact Dynamic Compression Plate (Synthes, West Chester, USA) and the Philos 3.5mm proximal humerus locking plate (Synthes, Oberdorf, Switzerland) were used. Screws were inserted either through the incisions already made or through additional stab incisions. Final alignment of the fracture and the implant were checked under the image intensifier. A drain was optional. Interrupted skin closure was performed with non-absorbable sutures. The patients were allowed to begin gentle passive range of motion exercises of the shoulder and elbow the day after the operation. They were discharged mostly within 5 days after the operation with out-patient physiotherapy.
RESULTS
From December 2004 to January 2010, we treated 5 patients with shaft of humerus fractures using the MIPO helical plate technique. All patients were male. The ages ranged from 20 to 69 years of age. The average age was 35. One patient had his arm caught in a roller machine, and another fell from standing height (Fig. 1). Three patients were motorcyclists involved in road traffic accidents, of which one had his arm pinned under the motorcycle (Fig. 2).
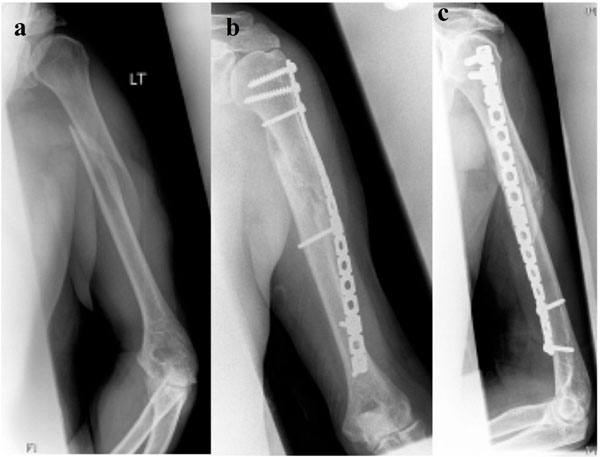
A 69 year-old man who fell and landed on his left arm. a Pre-operative radiograph shows a proximal third humeral shaft fracture (12-A1). b, c Radiograph results at six months after surgery.
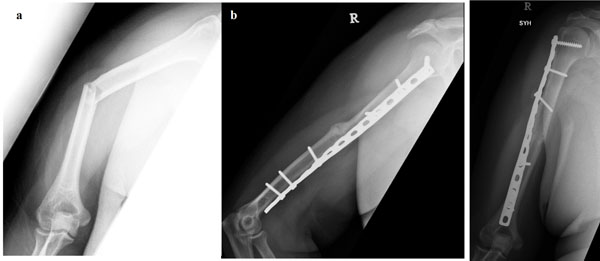
a A middle third fracture of the right humerus shaft (12-A3) of a 41 year-old male, whose right arm was pinned under a motorcycle. b, c The fracture had healed 4.5 months after surgery.
According to the AO classification, 3 fractures were categorized under type A and 2 fractures were categorized under type B (Table 1).
Patient Profile and Results
| Age/Sex | 69/Male | 20/Male | 21/Male | 41/Male | 25/Male |
|---|---|---|---|---|---|
| Injury | Fall | aRTA | Arm caught in machine | aRTA | aRTA |
| AO classification | 12-A1 | 12-B1 | 12-B2 | 12-A3 | 12-A3 |
| Part of humerus shaft | Proximal | Distal | Middle | Middle | Proximal |
| Plate | 4.5mm reconstruction | 4.5mm reconstruction | 4.5mm LCDCP | 4.5mm LCDCP | bProximal humerus locking |
| Length of stay (days) | 4 | 5 | 5 | 5 | c21 |
| Union (months) | 6 | 9 | 6 | 4.5 | 4 |
| Complications | Nil | Delayed union | Nil | Nil | Nil |
| Return to work (months) | Unemployed | 3 | 4.5 | 2 | 8 |
| Constant score | 18 (Good) | 9 (Excellent) | 10 (Excellent) | 15 (Good) | 16 (Good) |
| Mayo elbow performance score | 76 (Good) | 92 (Excellent) | 93 (Excellent) | 80 (Good) | 83 (Good) |
a Road traffic accident.
b Synthes Philos.
c Polytrauma patient.
Most patients stayed 4 to 5 days before discharge, except the patient who was a victim of poly-trauma (21days). They were followed up for at least 6 months. Union time ranged from 4 to 9 months, at an average of 6 months. None of them developed radial nerve palsy. The time taken for the patients to return to work ranged from 2 to 8 months, averaging 4.4 months. All patients achieved good to excellent shoulder and elbow function, according to the Constant score (for shoulder) and the Mayo elbow performance score. The scores were determined at 6 months after the operation.
DISCUSSION
The merits of the MIPO technique over open plating for humeral shaft fracture fixation have been documented. Lateral and anterior MIPO plating techniques have also been described, but they seem to be more suitable for fractures involving certain parts of the shaft, and thus may have their limitations.
In the proximal humerus, the lateral aspect of the greater tuberosity is flat and ideal for screw fixation to the neck and head of the humerus. The long head of the biceps tendon and the bicipital groove prevent the application of the plate on the anterior aspect of the proximal humerus [10]. In the middle one-third of the humerus, the insertion of the deltoid muscle limits the placement of the plate on the lateral aspect. The anterior or antero-medial surface is flat and ideal for plate application at the middle and distal one-third of the humerus [11]. Therefore, partial or nearly complete detachment of the deltoid insertion is inevitable in the lateral plating technique. Encroachment of the plate on the bicipital groove is a real problem in anterior plating of proximal humeral shaft fractures. The helical plate technique avoids both problems.
Yang [12] performed helical plating in 10 cases of comminuted proximal and middle one third of humerus fractures with satisfactory to excellent outcome. Although there was preservation of the deltoid insertion, open reduction via proximal deltopectoral approach and distal antero-lateral approach to the humerus was performed. Stripping of the soft tissue envelope of the humerus was likely, especially in the distal third of the shaft. In addition, the study did not include fractures of the distal third of the shaft. Our technique is minimally invasive and our study included fractures of proximal, middle and distal parts of the humeral shaft.
Compared to a straight plate, helical plates have several biomechanical advantages. Krishna et al. [13] studied the fracture holding capability of the hemi-helical plate (HHP) versus the straight plate in femur saw bones. Finite element analysis of the HHP was also performed to elucidate the efficacy of fracture-gap movement and closure, as well as the flexibility of the fixation under compressive, bending and torsional loads. The HHP was found to be superior to the straight plate in these areas:
- Increased torsional stiffness, but decreased flexion and compression stiffness.
- Fracture gap closure was enhanced. Gap closure became more uniform with increasing contour of the helical plate.
- Less stress shielding at fracture site, allowing bone to take on both compressive and tensile stresses.
- Axis of helical plate was parallel to orientation of helical stresses. HHP absorbed tensile stresses caused by torsional loading, which is useful in spiral fracture.
- Screw holding power was stronger, which decreased the risk of screw loosening.
In this technique, there is a potential risk of injuring the radial nerve, especially where the nerve winds around the lateral border of the humerus, about 8cm from the lateral epicondyle. One cadaveric study also showed that the musculocutaneous nerve crossed anterior to the helical plate in a medial to lateral direction at 12.2 to 14.8cm from the greater tuberosity [14]. The nerve may be endangered when inserting the plate or distal percutaneous screws. In our technique, we identified and protected the radial nerve, and took care to slide the plate underneath the nerve under direct visualization. Distal screws were placed only when the screw holes were well visualized and the nerve was out of the way. We reported no radial or musculocutaneous nerve palsies.
In our series, most of the fractures united between 4 to 6 months, which is comparable with results published by other authors [8,9,16], although one fracture united at 9 months. However, we did not find any predisposing factors to delayed union.
CONCLUSION
The MIPO helical plate technique combines the advantages of the minimally invasive technique and the biomechanical stability of the helical plate. Our study showed that this technique achieved satisfactory fracture union rates and functional recovery in our patients, but was limited by small patient numbers. Larger studies, perhaps with comparison to MIPO straight plate technique will be needed to validate the efficiency of this technique conclusively.
CONFLICT OF INTEREST
Declared none.
ACKNOWLEDGEMENT
Declared none.


