All published articles of this journal are available on ScienceDirect.
Triangle Tilt and Steel Osteotomy: Similar Approaches to Common Problems
Abstract
Background:
Each year, thousands of children worldwide suffer obstetric brachial plexus nerve injuries resulting not only in primary nerve injury, but also in development of secondary muscle and bone deformities of the shoulder. The triangle tilt surgery has been developed and shown to effectively address these deformities. The triangle tilt procedure was initially designed by the lead author (RKN) to follow the concepts of joint normalization featured in the Steel pelvic osteotomy used to correct developmental dysplasia of the hip joint, and indeed ultimately bears a striking resemblance to the Steel osteotomy. Prior to performing these bony surgical procedures, soft tissue procedures are performed to release the muscle contractures of the shoulder and hip. The purpose of this article is to compare and analyze the similarities between the indications, surgical techniques, involved anatomy, and outcomes of these operative procedures.
Methods:
A literature review was conducted using PubMed to identify articles pertaining to triangle tilt surgery and the Steel pelvic osteotomy. Functional parameters and surgical strategies were compared. Pre- and post-operative CTs were analyzed to compare anatomical results of the procedures.
Results:
Similarities were found between both procedures in terms of indications, involved anatomy, surgical techniques, and outcomes. The triangle tilt surgery is indicated to correct the developmental dysplasia of the glenohumeral joint in obstetric brachial plexus injury patients. Steel pelvic osteotomy is performed to correct the subluxation and dislocation of the hip innominate bone in patients with congenital dysplasia, cerebral palsy myelodysplasia, and poliomyelitis. The involved anatomy of both procedures is similar in that both involve limb girdles and ball-and-socket joints, namely the shoulder and hip. Both procedures are also triple osteotomies, the triangle tilt involving the acromion, clavicle and scapula while the Steel osteotomy involves the iliac spine, ischial and pubic ramus of the innominate bone. Surgical techniques also bear likenesses in that both can theoretically be done percutaneously. Post-operative CT outcomes of both surgeries showed improved anatomical positioning of the ball-and-socket joint congruency, and therefore better functional outcomes.
Discussion:
The similarities between the triangle tilt surgery and Steel pelvic osteotomy could potentially be useful as a model system in developing other procedures that involve the shoulder and hip. Future clinical applications include the development and implementation of new surgical procedures based on comparisons and adaptations from the hip to the shoulder and vice versa.
BACKGROUND
Obstetric brachial plexus injuries (OBPI) can affect any or all of C5-T1 nerve roots, although they most commonly involve the C5 and C6 nerve roots. Though patients may recover spontaneously within the first three months of life, inadequate recovery of neurological function may lead to long-term morbidity in this patient population by causing secondary muscular imbalances and bony deformities at the shoulder joint [1-4]. Muscle imbalance and weakness around the shoulder (the deltoid and external shoulder rotators) resulting from the upper plexus injury lead to glenohumeral dysplasia and joint incongruity [5, 6], which also impair the bone growth and development [7]. Significant secondary deformities that follow include medial rotation contracture (MRC) and elbow flexion. Several studies including ours have shown that soft tissue procedures such as muscles release and tendon transfers [8-15], lead to better shoulder abduction and flexion through releasing existing contractures, but does not realign the deformed glenohumeral joint (GHJ). The triangle tilt (TT) surgery has been shown to effectively address these bony deformities [16-24], which improves overall functions of the shoulder. The triangle tilt surgical technique includes osteotomies of the clavicle and the neck of the acromion, releasing the distal acromioclavicular triangle to tilt back into its neutral position and allowing the humeral head to improve congruency [16-24]. Triangle tilt is also performed as a salvage procedure in patients in whom other shoulder surgeries failed [18].
The most common etiology of hip dysplasia is developmental dysplasia of the hip (DDH) [25]. Myelodysplasia, cerebral palsy and poliomyelitis are the other etiologies of hip dysplasia [26]. Spastic hip subluxation and dislocation are common problems in children with cerebral palsy [27-29]. In addition, extensive deficiency of soft-tissues particularly the hip abductors can be an important contributing cause of hip instability in patients in whom prior surgical procedures have failed [30]. There are three types of DDH, categorized by increasing severity: type I (hyperlaxity of the joint), type II (subluxable head), and type III (dislocated hip) [31]. In DDH, characteristic anatomic changes of the hip joint include hip dysplasia, subluxation or dislocation of the femoral head, and contractures of the iliopsoas and adductor muscles which must be released [32]. The Steel osteotomy has been shown to effectively correct the bony deformities of DDH [26]. The purpose of this study is to compare the triangle tilt surgery to the Steel pelvic osteotomy and determine if there are any similarities present between the indications, surgical techniques, involved anatomy, and outcomes of both of these procedures.
METHODS
A literature review was conducted using PubMed to identify articles pertaining to triangle tilt surgery and Steel pelvic osteotomy. The overall aim was defined to compare different aspects of these two procedures. The publications reviewed for this article refer to the indications, surgical techniques, involved anatomy, and outcomes of both of these procedures. Pre- and post-operative CTs were analyzed to compare anatomical results of the procedures.
Search Strategy
The Medline database was searched for literature with the following key words: “obstetric brachial plexus injury”, “obstetric brachial plexus injuries”, “obstetric brachial plexus palsy”, “triangle tilt surgery”, “developmental dysplasia of the hip”, “DDH”, “Steel osteotomy”, “pelvic osteotomy”, “triple osteotomy of the innominate bone”, “indications”, “surgical technique”, “anatomy”, “outcomes”, “CTs”, and “radiographs”. Numerous combinations of these terms were individually applied and the results compared using Medline’s search history feature. Articles were also identified by using the function “related articles” in PubMed.
RESULTS
Indications
The triangle tilt surgery is indicated to correct the medial rotation contracture (MRC) and the scapular hypoplasia, elevation and rotation (SHEAR) deformities in OBPI patients. Weak external rotation secondary to OBPI causes MRC which leads to deformation of the bones of the shoulder. SHEAR is accompanied by progressive dislocation of the humeral head. The triangle tilt procedure corrects the impingement which occurs in the SHEAR deformity and improves the position of the humeral head in the glenoid [16]. Prior studies have shown how progressive glenohumeral dysplasia occurs in OBPI patients [33, 34]. This process is comparable to one observed in the acetabulum in developmental dysplasia of the hip [35]. Bony procedures similar to the triangle tilt surgery are used to “tilt” the acetabulum and correct the position of the femoral head within the acetabulum [35, 36].
Steel pelvic osteotomy is performed to correct DDH, among other conditions. Its goal is to stabilize the hip at the level of the acetabulum in cases of hip dislocation or subluxation. The indications for this procedure can be summarized by any condition of the hip joint in a child that has resulted in a faulty femoral head-acetabular relationship and where restoration of stability to the hip is not possible by any one of the displacement osteotomies (Salter’s, Pemberton’s or Chiari’s) or by the arthroplasty of Colonna [26].
Anatomy
The anatomy of the shoulder girdle is structured around the primary bones that constitute - the scapula, humeral head, and clavicle. The superolateral surface of the scapula forms a smooth concave partial cavity called the glenoid fossa, which is also simply called the glenoid. The shoulder joint is one of the most mobile joints, and characterized by a broad range of motion when compared to the hip joint, which is relatively immobile. Although, both joints are ball-and-socket type, the shoulder joint is very unstable, and therefore it can slip off easily like a “golf ball” (humeral head) on a flat “tee” (glenoid), unlike the hip joint, which is relatively very stable. The hip joint is the true or complete “ball” (femoral head) and “socket” (acetebulum) type joint. The shoulder joint is highly dependent on the surrounding soft tissues for its stability whereas the hip joint is inherently stable because of the encircling bony anatomy. The surfaces of the glenoid fossa and humeral head are protected by articular cartilage which also serves to improve congruence of the joint. A ring of fibrous connective tissue called the labrum surrounds the glenoid and provides further cushioning. Surrounding the entire GHJ is a large, dynamic capsule, reinforced by glenohumeral (GH) ligaments and associated muscles [37].
The complete ball-and-socket type of synovial hip joint is formed by the rounded head of the femur articulating with the cup-like acetabulum of the pelvis. Both joint surfaces are covered with a strong, lubricated layer of articular cartilage. The cuplike acetabulum is actually formed by the union of three pelvic bones: the ilium, ischium, and pubis [38]. The triradiate cartilage, a “Y”-shaped growth plate that separates these three bones, is fused definitively at ages 14-16 [39]. Almost half of the roughly spherical femoral head is contained within the acetabulum. This grip is further augmented by a ring-shaped fibrocartilaginous lip, the acetabular labrum [38]. These soft tissues provide stability and support the ball-and-socket joint congruence. The range-of-motion of both the shoulder and hip joints is very broad, allowing for internal and external rotation, extension and flexion, abduction, and adduction.
Surgical Techniques
In many OBPI patients, prior to triangle tilt being performed, the modified Quad surgery is performed [15] to release the muscle contractures near the shoulder and improve shoulder range of motion, especially abduction. This is then followed by the triangle tilt, the surgical strategy of which entails releasing the distal acromioclavicular triangle (“ACT”, the sides of which are defined by the clavicular shaft and the acromion process and the base by an imaginary line connecting their medial ends) from the medial spine of the scapula and the medial clavicle by osteotomies of the clavicle and neck of the acromion. Essentially, this levels the “triangle” by allowing the distal triangle to “tilt” back into its neutral position; hence, the name given to the procedure, the “triangle tilt” [37]. The impingement of the ACT on the humeral head is relieved by releasing and tilting the ACT back to neutral. This allows the humeral head to be repositioned passively into a neutral position in the glenoid fossa as well [16-24].
The triangle tilt procedure consists of:
- osteotomy of the clavicle at the junction of the middle and outer thirds
- osteotomy of the acromion at its junction with the spine of the scapula
- ostectomy of the superomedial angle of the scapula
- splinting of the limb in adduction, 5° of external rotation and full forearm supination.
Splinting is maintained for six weeks, after which the splint may be worn only at night for an additional three to six months. Other elements of the operation include bone grafting of the site of the acromial osteotomy and fixation of the clavicular osteotomy to prevent nonunion. Posterior glenohumeral capsulorraphy can be performed in patients with posterior instability of the shoulder diagnosed by preoperative CT or positional MRI [16], and still present intraoperatively after the initial elements of the triangle tilt surgery are performed.
Similar to the use of modified quad surgery prior to the triangle tilt, the Steel pelvic osteotomy is often preceded by a surgical release of the hip muscles to bring the femoral head down to the level of the acetabulum.
The Steel procedure (Fig. 1A,1B) consists of:
- osteotomy from the anterior inferior iliac spine (ASIS) to the sciatic notch
- osteotomy of the ischial ramus
- osteotomy of the superior pubic ramus
- stabilization of acetabular fragment with bone graft removed from superior wing of ilium and fixed with two extra-articular pins penetrating to inner table of ilium.
- the spica cast applied with the hip in 20 degrees abduction, 5 degrees flexion and neutral rotation [26, 40].
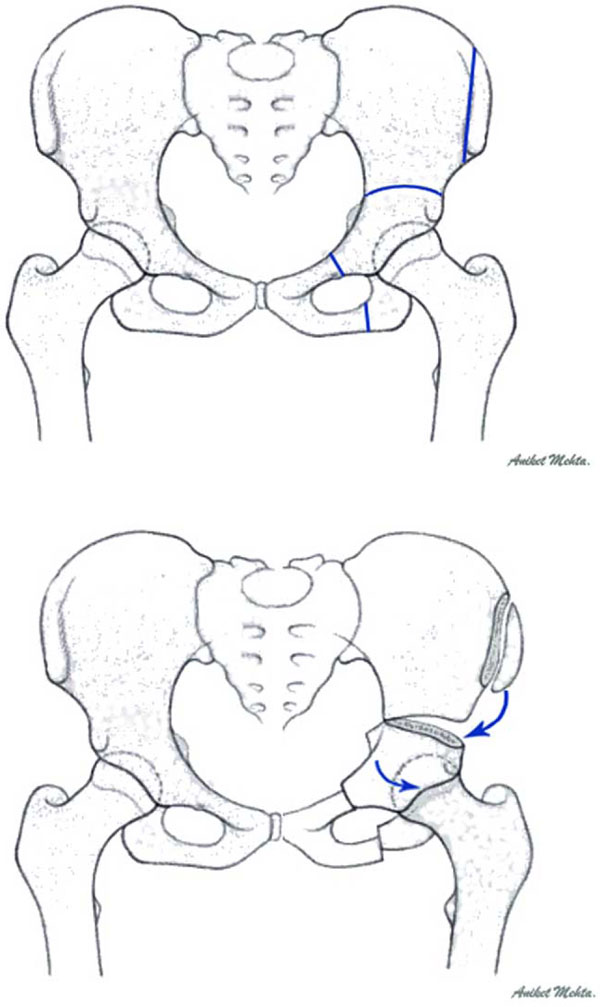
(A) Depicts location of osteotomies for Steel procedure: 1) On the ilium superior to the acetabulum. 2) Inferior aspect of the ischium. 3) On the superior and inferior pubic rami. (B) Depicts transposition of iliac crest bone graft and correction of acetabular position. The position of the acetabulum is corrected by rotating the fragment created by these osteotomies.
Fig. (2) is a post-Steel anterior view 3D-CT. The osteotomies of the superior pubic and ischial rami and from the ASIS to the sciatic notch are depicted. The bone graft has been removed from the superior wing of the ilium and repositioned to stabilize the acetabular fragment.
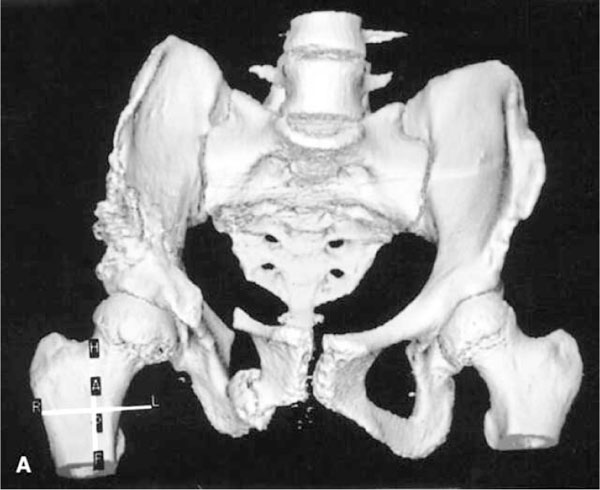
A post-Steel osteotomy anterior view 3D-CT. The osteotomies of the superior pubic and ischial rami and from the ASIS to the sciatic notch are depicted. The bone graft has been removed from the superior wing of the ilium and repositioned to stabilize the acetabular fragment. Reproduced with permission from Frick S, Kim S, Wenger D; “Pre- and Postoperative Three-Dimensional Computed Tomography Analysis of Triple Innominate Osteotomy for Hip Dysplasia”, Journal of Pediatric Orthopaedics, Vol. 20, Issue 1, pp.116-23.
Outcomes
In a retrospective study conducted by Nath et al. 2007 [16]., 44 children underwent the triangle tilt surgery between February and August 2005 to correct the medial rotation contracture and SHEAR deformities caused by their initial obstetric brachial plexus injuries. The outcomes of this surgery were improved shoulder function and corrected glenohumeral axes in these patients. In the 40 children who were followed up for more than one year, the posture of the arm at rest was improved and active external rotation increased by a mean of 53° (0° to 115°). Furthermore, there was a mean improvement of 4.9 points (1.7 to 8.3) of the Mallet shoulder function score after surgical correction of the bony deformity. The angle of the hand-to-mouth movement (bugler’s sign) improved significantly by decreasing from a mean of 110° (60° to 160°) preoperatively to 36° (0° to 100°; t-test p < 0.000) postoperatively. Additionally, supination of the forearm increased from a pre-operative mean of -12° (-80° to +50°) to a postoperative mean of 36° (-45° to +90°; t-test, p < 0.000). Post-operative CT scans showed the head of the humerus relocated within the glenoid fossa [16].
A study by de Kleuver et al. describes the results of the triple osteotomy of the pelvis for developmental dysplasia of the hip (acetabular dysplasia). The average follow-up for the patients was ten years (8 to 15). Out of 48 hips, 39 (81%) were improved compared with before operation, with 29 (60%) scoring good or excellent. Radiographic evaluation showed improvement of the average centre-edge (CE) angle by 19°, the acetabular index by 12°, and the anterior centre-edge angle by 26°. The satisfactory long-term clinical outcomes and radiographic results provide support and encouragement to continue this treatment for symptomatic acetabular dysplasia in these patients [41].
Both surgeries measure their clinical outcomes in similar ways. OBPI patients are often assessed by a system evaluating shoulder range of motion called the Modified Mallet System, originally introduced by Mallet [42]. Specifically, the Modified Mallet System evaluates the ability to carry out five functions: external rotation, abduction, hand to mouth, hand to lower spine, and hand to back of neck. Each movement is scored on a scale of 1 to 5 (1 being no function, 5 being full function). An important point to note about using this system is that when comparing treatment modalities, the scores of individual patients should not be compared. Rather, one should compare scores before and after treatment to evaluate the improvement gained by each patient. The Nath modification of Mallet’s system (Fig.3) includes additional functions and positions such as arm postion at rest and supination [24, 37].
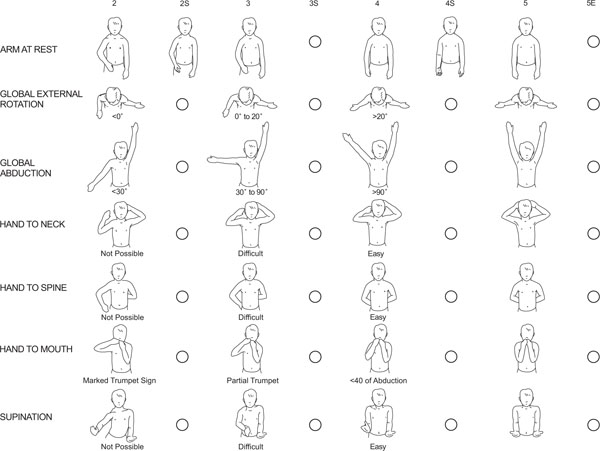
The Nath Modification of Mallet’s System [24, 37]: Clinical Scoring of Function. In addition to assessing the classical functions of the Modified Mallet system, supination and the resting position are evaluated. To further define deformity, fixed forearm supination (positions 2S, 3S, and 4S) as well as external rotation position (5E) are scored.
Clinical functioning of the hip is assessed in a similar way using the Modified Merle d'Aubign´e and Postel clinical scoring system (Table1). This system evaluates the clinical condition of a patient by three categories, each having six grades. Level of pain is gauged in conjunction with associated activity level. Walking ability is assessed by distance and form. Range of motion is measured by percentage from 0-100 [41].
| Pain | Walking | Range of Motion (%) |
|---|---|---|
| 1. Severe, prevents walking | 1. Bedridden | 1. 0 - 39 |
| 2. Severe when walking | 2. Indoors only | |
| 3. Moderate,permits walking but limits activity | 3. Limited, less than one block | 3. 40 - 59 |
| 4. Pain after walking | 4. Long distances with cane or crutch | 4. 60 - 79 |
| 5. Slight or intermittent pain | 5. Slight limp | 5. 80 - 94 |
| 6. No pain | 6. Normal | 6. 95 - 100 |
Clinical grade (total points): Excellent 18; Good 15 to 17; Fair 12 to 14; Poor 3 to 12.
Results of both surgeries are also measured anatomically and radiographically. In triangle tilt surgery, one of the parameters measured is the posterior subluxation of the humeral head (PHHA) according to Waters et al. [33], calculating as the percentage of the humeral head anterior to the scapular line (Fig.4). Glenoid version is another parameter used to assess the outcomes of triangle tilt surgery (Fig.4). This is measured according to Friedman et al. [45]. Triangle tilt also assesses its results with the SHEAR percentage (Fig.5). The SHEAR deformity (scapular hypoplasia, elevation, and rotation) is a common result of OBPI [46]. The triangle tilt measures its outcomes by reducing the SHEAR percentage. Calculating this value entails measuring the scapular elevation above the clavicle in an anterior view of a 3D - reconstruction of a CT image. The area of the scapula that is visible above the clavicle is divided by the total scapular area and corrected for rotational artifacts by subtraction of the unaffected side from the affected side before multiplying by 100 to obtain percent elevation [24].
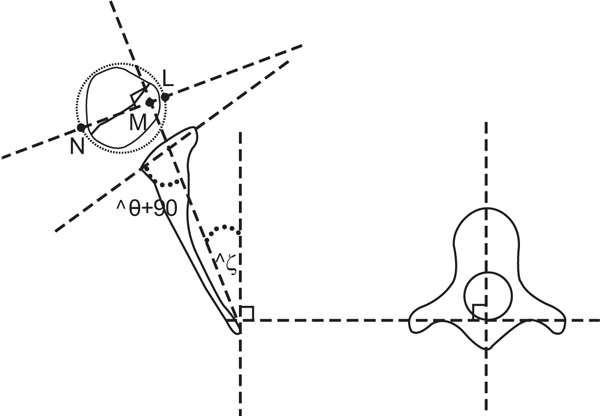
Schematic drawing showing the method of calculating glenoid version (θ), according to Friedman et al. [45], and percentage of humeral head anterior to scapular line (PHHA), according to Waters et al. [33]. Measuring the glenoid version angle (θ): The scapular line is drawn between the medial margin of the scapula to the midpoint of the glenoid. Another line is drawn through the anterior and posterior aspects of the glenoid labrum. The angle between these two lines is measured, and 90° is subtracted. A negative value indicates a retroverted glenoid. A line perpendicular to the scapular line is drawn and the PHHA is defined as the ratio of the distance from the scapular line to the anterior portion of the head to the diameter of the humeral head (LM / LN X 100). Reproduced from Nath RK, Paizi M: Scapular deformity in obstetric brachial plexus palsy: a new finding. Surg Radiol Anat 2007, 29: 133-140.
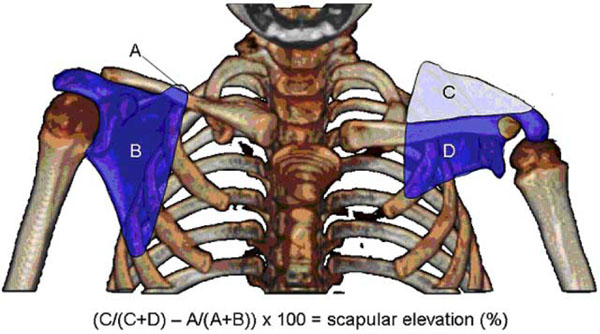
Measuring scapular elevation to quantitate extent of SHEAR deformity. An anterior 3D-CT is used to measure scapular elevation. The area of each portion of both scapulas is measured as indicated (areas A-D). The area above the scapula is divided by the total scapular area and corrected for rotational artifacts by subtraction of the unaffected side from the affected side before multiplying by 100 to obtain percent elevation. Shown is the CT of a patient who was calculated to have 37% scapular elevation. Reproduced from Nath RK, Somasundaram C, Melcher SE, Bala M, Wentz MJ: Arm rotated medially with supination - the ARMS variant: description of its surgical correction. BMC Musculoskelet Disord 2009, 10: 32.
For dysplastic hips, we find comparable methodologies to evaluate outcomes anatomically and radiographically. One of the most important parameters is the CE angle (Fig.6), as described by Wiberg [47], measured on an AP view of the pelvis. This measurement is critical since an abnormal CE angle is diagnostic of acetabular dysplasia. This angle is used to evaluate the lateral and superior coverage of the femoral head by the bony acetabulum. This measurement is obtained by drawing a vertical line through the center of the femoral head perpendicular to the horizontal line extending through the center of both femoral heads: respectively C1 and C2. Another line is then drawn from the center of the femoral head to the most superolateral point of the acetabulum, representing the E (edge) point. The angle between this line and the vertical line represents the CE angle. According to Wiberg, values above 25° are reported as normal; values between 20° and 25° are considered borderline; and a CE angle of less than 20° is considered diagnostic of acetabular dysplasia [31].
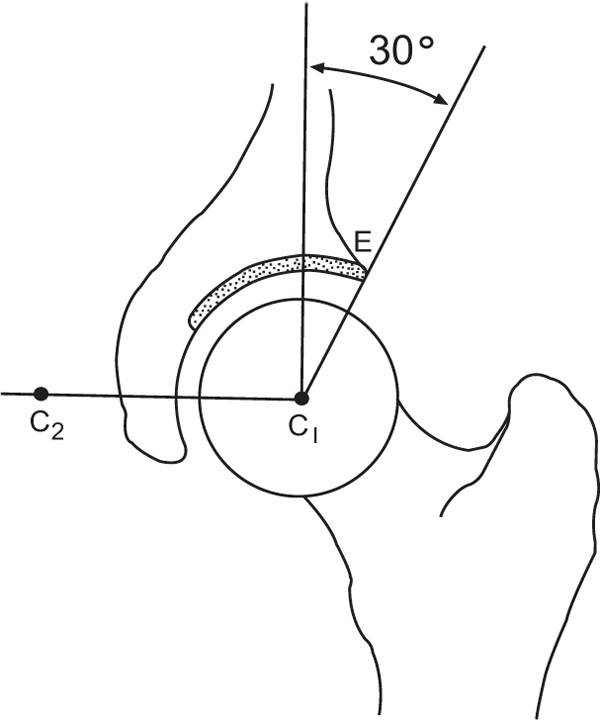
CE angle. A horizontal line extends from the center of each femoral head (C1 and C2). A vertical line is drawn perpendicular to this line. Point E (edge) is the most lateral point of the acetabulum. The CE angle is measured between the vertical and the line passing through C1/C2 and E. CE angle > 25° is normal. (With kind permission from Springer Science + Business Media: Skeletal Radiology, “Radiographic measurements of dysplastic adult hips”, Vol. 26, 1997, p. 76, Delaunay S, Dussault RG, Kaplan PA, Alford BA, Fig. 1)
There exists another entity called the anterolateral acetabular lip angle (ALAL, Fig.7). This measurement is the angle (α) formed by a line along the anterolateral rim of the acetabulum and the horizontal reference line. On an anterior view, the horizontal reference line is constructed by the perpendicular to a line through the center of the pubic symphysis and the center of the sacrum. This measurement provides information about the orientation of the acetabulum in the frontal plane and thus is used to determine the postoperative changes in the abduction/adduction of the acetabulum.
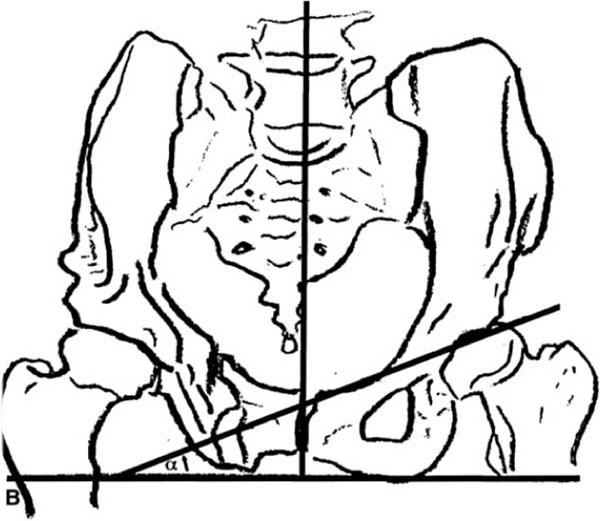
Anterolateral acetabular lip angle (ALAL). This measurement is the angle (α) formed by a line along the anterolateral rim of the acetabulum and the horizontal reference line. On an anterior view, the horizontal reference line is constructed by the perpendicular to a line through the center of the pubic symphysis and the center of the sacrum. This measurement provides information about the orientation of the acetabulum in the frontal plane and thus is used to determine the postoperative changes in the abduction/adduction of the acetabulum. Reproduced with permission from Frick S, Kim S, Wenger D; “Pre- and Postoperative Three-Dimensional Computed Tomography Analysis of Triple Innominate Osteotomy for Hip Dysplasia”, Journal of Pediatric Orthopaedics, Vol. 20, Issue 1, pp.116-23.
The CE and ALAL angles correlate with the glenoid version parameter in OBPI. The acetabulum and glenoid are similar in that they both form the “socket” of a ball-and-socket joint. When the secondary deformities due to OBPI and DDH occur [26], the normal anatomical orientation of the articulation between the “balls” (humeral and femoral heads) and “sockets” (glenoid, acetabulum) is altered and new and different “angles” and “versions” develop.
Analogous to the PHHA parameter measured in cases of OBPI, there is an entity termed as the percentage of femoral head covered by the acetabulum (PFHA) (Fig.8). This is yet another important parameter of the AP view of the pelvis in the assessment of the position and appearance of the femoral head. The normal femoral head is round and congruent with the acetabulum, except for a small superior centro-medial depression which represents the fovea. However, in DDH patients, the femoral head can be abnormally flat and/or laterally displaced, with loss of congruity within the acetabulum. As a result, the mechanics of the hip are altered which can lead to early degenerative changes. The PFHA determines the congruity between the femoral head and the acetabulum [48]. Three vertical lines are utilized to determine coverage. Line 1 passes through the most medial aspect of the joint space. Line 2 passes through the lateral aspect of the acetabulum. Line 3 passes through the most lateral aspect of the femoral head. The distance between lines 1 and 2 (A) is divided by the distance between lines 1 and 3 (B). The A/B ratio obtained is converted to a percentage [R(A/B) × 100]. Coverage of less than 75% is determined to be pathologic [31].
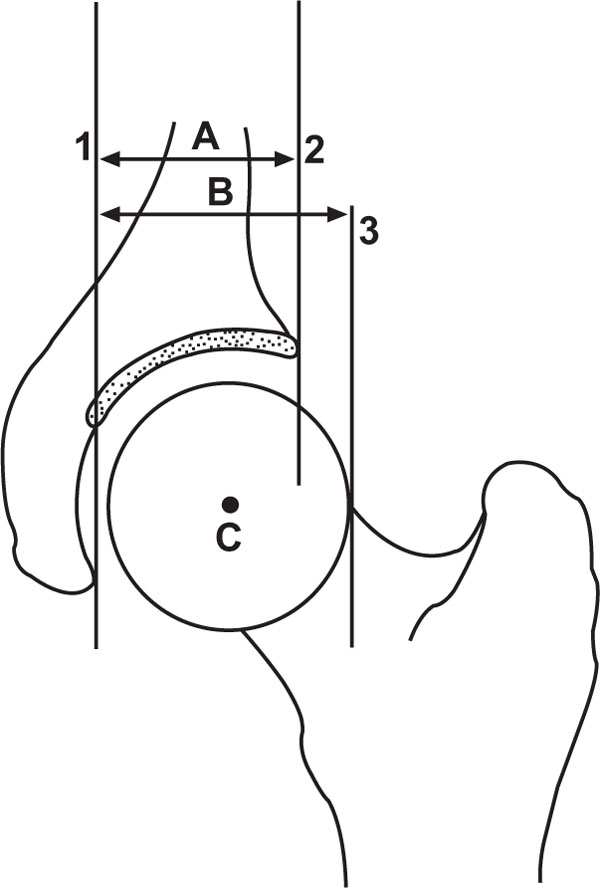
Percentage of the femoral head covered by acetabulum (PFHA): (A/B) ×100. Coverage < 75% is pathologic. (With kind permission from Springer Science + Business Media: Skeletal Radiology, “Radiographic measurements of dysplastic adult hips”, Vol. 26, 1997, p. 78, Delaunay S, Dussault RG, Kaplan PA, Alford BA, Fig. 7).
Pre- and post-operative CTs were analyzed to compare anatomical results of both procedures. Post-operative CTs outcomes of both surgeries showed improved anatomical positioning and remodeling. Figs.(9, 10) show pre- and postoperative axial 2D CTs, respectively, of Steel osteotomy for a patient with hip dysplasia. Notice the improvement in the PFHA, pre- to post-Steel osteotomy. In the pre-op CT, a large portion of the femoral head is uncovered by the acetabulum. The post-op CT shows improvement in that a greater portion of the femoral head is now being covered by the acetabulum [49].

Preoperative axial 2D CT of Steel osteotomy for a patient with hip dysplasia. Notice the large portion of the femoral head that is uncovered by the acetabulum. This patient has a less than optimal PFHA. Reproduced with permission from Frick S, Kim S, Wenger D; “Pre- and Postoperative Three-Dimensional Computed Tomography Analysis of Triple Innominate Osteotomy for Hip Dysplasia”, Journal of Pediatric Orthopaedics, Vol. 20, Issue 1, pp.116-23.

Postoperative axial 2D CT of same patient as Fig. (9). Notice the improvement in the PFHA, pre- to post-Steel osteotomy. The post-op CT shows a greater portion of the femoral head now being covered by the acetabulum. Reproduced with permission from Frick S, Kim S, Wenger D; “Pre- and Postoperative Three-Dimensional Computed Tomography Analysis of Triple Innominate Osteotomy for Hip Dysplasia”, Journal of Pediatric Orthopaedics, Vol. 20, Issue 1, pp.116-23.
Similarly, Fig. (11) demonstrates an axial CT of an affected shoulder of an OBPI patient before and after triangle tilt surgery.
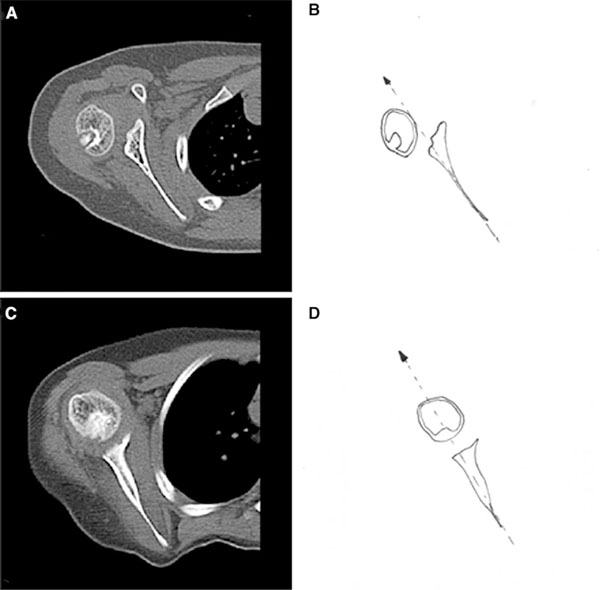
Axial CT of an affected shoulder of an OBPI patient before and after triangle tilt surgery. (A) CT image before triangle tilt surgery showing posterior subluxation of the humeral head, measured by PHHA, and joint incongruity of the glenohumeral joint, measured by glenoid version. (B) Line diagram of the pre-triangle tilt CT image seen in (A). (C) CT image after triangle tilt surgery showing improvement in PHHA and glenoid version. (D) Line diagram of the post-triangle tilt CT image seen in (C). Reproduced from Nath RK, Avila MB, Karicherla P. “Triangle tilt surgery as salvage procedure for failed shoulder surgery in obstetric brachial plexus injury.” Pediatr Surg Int. 2010 Jul 29. [Epub ahead of print].
- CT image before triangle tilt surgery showing posterior subluxation of the humeral head, measured by PHHA, and joint incongruity of the glenohumeral joint, measured by glenoid version.
- Line diagram of the pre-triangle tilt CT image seen in (A).
- CT image after triangle tilt surgery showing improvement in PHHA and glenoid version.
- Line diagram of the post-triangle tilt CT image seen in (C) [18]
Another related parameter that is used in the evaluation of dysplastic hips is the acetabular index (Fig.12). This value is an index of depth to width which assesses the depth of the acetabulum. The width (W) of the acetabulum is measured from point E to the lowermost point of the acetabulum. The depth (D) is evaluated by measuring the perpendicular distance to the most medial point of the weight-bearing portion of the acetabulum, recognized by its sclerotic, arched appearance, resembling an eyebrow (“sourcil cotyloïdien”). The ratio (D/W) ×100 is then calculated. Values over 38% are considered normal and values below are dysplastic [31, 50].

Acetabular index of depth (d) to width (w). (With kind permission from Springer Science + Business Media: Skeletal Radiology, “Radiographic measurements of dysplastic adult hips”, Vol. 26, 1997, p. 76, Delaunay S, Dussault RG, Kaplan PA, Alford BA, Fig. 3).
DISCUSSION
This review article compares the triangle tilt surgery to the Steel pelvic osteotomy and discusses their similar approaches to common problems. Both procedures share similarities between their indications, involved anatomy, surgical techniques, and measurements of clinical and anatomical outcomes. In fact, the triangle tilt surgery was conceptually designed initially to mimic the surgical approach taken by the Steel osteotomy.
The triangle tilt is indicated for the surgical correction of bony deformities secondary to OBPI, such as glenohumeral dysplasia, posterior subluxation and dislocation of the humeral head, medial rotation contracture, and SHEAR deformity. The Steel osteotomy is indicated for the surgical correction of the bony deformities of DDH, including acetabular dysplasia and subluxation or dislocation of the femoral head. Both OBPI and DDH are conditions noted in children immediately after birth.
The anatomy that is affected in both of the conditions and procedures is also very comparable. OBPI and DDH both affect limb girdles; OBPI affecting the shoulder girdle while DDH affects the hip girdle. Both surgeries involve ball-and-socket joints, with the triangle tilt addressing the humeral head and glenoid while the Steel osteotomy addresses the femoral head and acetabulum.
Both procedures are also comparable in terms of measuring their clinical and anatomical outcomes. While the triangle tilt assesses its clinical outcomes using the Modified Mallet Scale, the Steel osteotomy evaluates clinical functioning of the hip in a similar way using the Modified Merle d'Aubign´e and Postel clinical scoring system. The Modified Mallet Scale evaluates the ability to carry out five functions: external rotation, abduction, hand to mouth, hand to lower spine, and hand to back of neck. Each movement is scored on a scale of 1 to 5 (1 being no function, 5 being full function). The Nath modification of Mallet’s system includes additional functions and positions such as arm at rest and supination [24, 37]. The Modified Merle d'Aubign´e and Postel clinical scoring system accounts for the quality, distance, form, difficulty, and range-of-motion of the activity level. It scores the overall clinical grade by total points on a scale with four categories of functioning.
Similarities also exist between techniques of measuring anatomical results of both procedures. Triangle tilt measures such parameters as glenoid version, PHHA, and SHEAR deformity. Comparably, Steel osteotomy evaluates its results with similar entities such as the CE and ALAL angles, PFHA, and the acetabular index.
The CE and ALAL angles correlate with the glenoid version parameter in OBPI. This, again, is related to the anatomy involved in both conditions. As secondary deformities due to OBPI and DDH occur, the normal anatomical orientation of the articulation between the “balls” (humeral and femoral heads) and “sockets” (glenoid, acetabulum) is altered and new and different “angles” and “versions” develop. These parameters allow for an objective, quantitative method to measure pre-operative conditions and evaluate post-operative results, assessing overall outcome in terms of total improvement.
PHHA and PFHA, likewise, are analogous to one another in the way they are calculated and the meaning of their values. Both parameters measure the percentage of dislocation/ subluxation. Again, both values are linked to the similar anatomy of the ball-and-socket joints of the shoulder and hip.
The SHEAR deformity and acetabular index also are very comparable in the way they are calculated. Both of these parameters quantitatively assess the level of abnormal morphology of the involved deformities. The SHEAR percentage is calculated as
(C/(C+D) – A/(A+B)) X 100 = scapular elevation (%), where:
A = area of scapula visible above clavicle (unaffected side)
B = area of scapula visible below clavicle (unaffected side)
C = area of scapula visible above clavicle (affected side)
D = area of scapula visible below clavicle (affected side)
Essentially, the area of the scapula that is visible above the clavicle is divided by the total scapular area and corrected for rotational artifacts by subtraction of the unaffected side from the affected side before multiplying by 100 to obtain percent elevation
The acetabular index is a related parameter that is used in the evaluation of dysplastic hips. This value is an index of depth (D) to width (W) which assesses the morphology of the acetabulum. The measurement is calculated as follows: (D/W) ×100. Values over 38% are considered normal and values below are dysplastic. The SHEAR percentage and acetabular index both involve ratios and percentages to quantitate the abnormal anatomy involved in both of these conditions.
The similarities between the indications, involved anatomy, surgical techniques and measurements of clinical and anatomical outcomes of the triangle tilt surgery and Steel pelvic osteotomy can be extrapolated to other aspects and comparisons between not only these surgeries but other procedures involving the shoulder and hip as well. Future clinical applications include other surgical procedures being developed and implemented based on comparisons and adaptations from surgical procedures involving the hip to those of the shoulder and vice versa. More recently, the lead author (RKN) has shown that triangle tilt surgery has better functional outcomes when performed in patients less than 2 years of age, when compared to patients over 2 years old [51]. In addition, this study [51] demonstrated that triangle tilt can be performed and effective in as early as 9 months old patients, who have not undergone other surgeries. This approach described in OBPI patients by Nath et al. 2011 [51] may be considered for hip dysplasia patients as well.
COMPETING INTERESTS
The authors declare that they have no competing interests.
AUTHORS' CONTRIBUTIONS
RKN conceived and participated in the design of the study and revision of the manuscript. FM participated in the design of the study, collection of data, and drafting the manuscript. CS participated in collection and interpretation of data, and revising the manuscript addressing the reviewers’ comments. All authors have read and approved the final manuscript.
ACKNOWLEDGEMENTS
The authors would like to thank Mr. Aniket Mehta, M.S., for his technical assistance in this article.


