All published articles of this journal are available on ScienceDirect.
Treatment of Unstable Thoracolumbar Burst Fractures by Indirect Reduction and Posterior Stabilization: Short-Segment Versus Long-Segment Stabilization
Abstract
In order to compare short-segment stabilization with long-segment stabilization for treating unstable thoracolumbar fractures, we studied fifty patients suffered from unstable thoracolumbar burst fractures. Thirty of them were managed with long-segment posterior transpedicular instrumentation and twenty patients with short- segment stabilization. The mean follow up period was 5.2 years. Pre-operative and post-operative radiological parameters, like the Cobb angle, the kyphotic deformation and the Beck index were evaluated. A statistically significant difference between the two under study groups was noted for the Cobb angle and the kyphotic deformation, while, as far as the Beck index is concerned, no significant difference was noted. In conclusion, either the long-segment or the short-segment stabilization is able for reducing the segmental kyphosis and the vertebral body deformation postoperatively. However, as time goes by, the long-segment stabilization is associated with better results as far as the radiological parameters, the indexes and the patient’s satisfaction are concerned.
INTRODUCTION
The restoration of the vertebral column stability and the decompression of the spinal canal are the goals of the treatment of thoracolumbar fractures. Earlier mobilization of the patient is the profit when they are achieved. By leaving uninjured segments intact, transpedicular constructs diminish the number of segments stabilized and fused, preserving the maximal thoracolumbar motion.
It has been demonstrated that short-segment (SS) instrumentation is associated with an unacceptable rate of failure [1]. The highest rate of the instrumentation failure resulting in re-kyphosis of the entire segment is associated with SS posterior reduction and stabilization of burst fractures showing the inadequacy of the SS transpedicular instrumentation used for the treatment of thoracolumbar and lumbar fractures [2]. Bent screws and kyphosis did not always herald a clinical failure, but patients who have kyphosis more than 10 degrees even if it is progressively increased, feel substantially more pain that those who have little or no loss of correction of the fractured vertebral body [3]. Significant correction loss and failure was also found in long-segment (LS) instrumentation [2].
The current study is based on the operative treatment of a single type of fractures (fractures classified as AO “A3.3”). The particular question addressed by this study was whether LS posterior stabilization gives significantly better results comparing to SS stabilization.
MATERIALS AND METHODOLOGY
Fifty patients operated for unstable thoracolumbar burst fractures were reviewed as part of a prospective randomized study. Indirect reduction and stabilization was performed using the Miami-Moss system (DePuy Orthopaedics, Inc., USA). Long-segment posterior transpedicular instrumenta-tion combined with short-segment fusion was performed in 30 cases and short-segment stabilization and fusion in 20 cases.
Patients with pathological fractures or multilevel injuries were excluded from the study. In addition, patients who were managed with a delay of 10 days or more were also excluded of this study. The most common level of injury was L1 (n = 25) and T12 (n = 18) as seen in Table 1.
Causes and Location of the Spinal Fractures Treated Operatively – Additional Lesions
| Cause of Accident | ||
|---|---|---|
| Automobile | 28 | |
| Occupational | 11 | |
| Motorcycle | 8 | |
| Horse | 3 | |
| Location of the Fracture | ||
| T11 | 6 | |
| T12 | 16 | Two pts also presented with a L3 vertebral body burst fracture |
| L1 | 23 | |
| L2 | 5 | |
| Additional Lesions | ||
| Long Bone Fracture | 9 | |
| Other Fractures | 6 | |
| Rib Fractures | 5 | |
| Concussion | 4 | |
| Heart Contusion | 2 | |
| Lung Contusion | 2 | |
| Without Other Lesions | 23 | |
The mean patients’ age was 32 years old (13-55 years old) and the leading cause of the fracture was motor vehicle accidents followed by occupational injuries (Table 1). The pre-operative evaluation included computed tomography (CT) scanning of the spine. Twenty-five patients were evaluated additionally with magnetic resonance imaging (MRI). All fractures were classified as AO “A3.3” which characterized by at least partial comminution of the vertebral body with centrifugal extrusion of the fragments [4].
Patients were divided into two groups. The first group included 20 patients (12 males and 8 females) who had been managed with SS pedicle instrumentation constructs spanning two vertebrae, one cephalad and one caudal to the fracture (Fig. 1a, b). The mean follow up for this group was 34 months (range, 25-70 months).
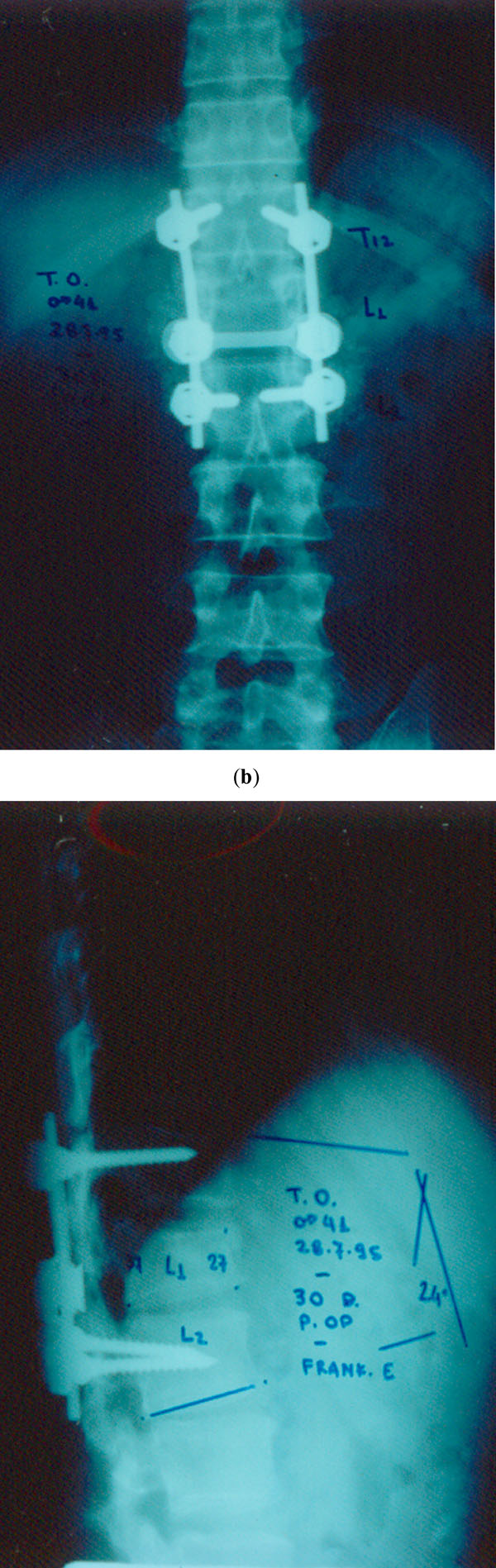
(a, b) Anteroposterior and lateral radiographs showing a Short-segment instrumentation system.
The second group included 30 patients (20 males and 10 females) who had been managed with LS pedicle instrumentation constructs (Fig. 2a, b). In this group the instrumentation spanned four vertebrae, two cephalad and two caudal to the fracture. The mean follow up of this group was 36 months (range, 24-72 months). In two cases a long instrumentation construct was applied to stabilize both a thoracic (T12) fracture and a lumbar L3 fracture.
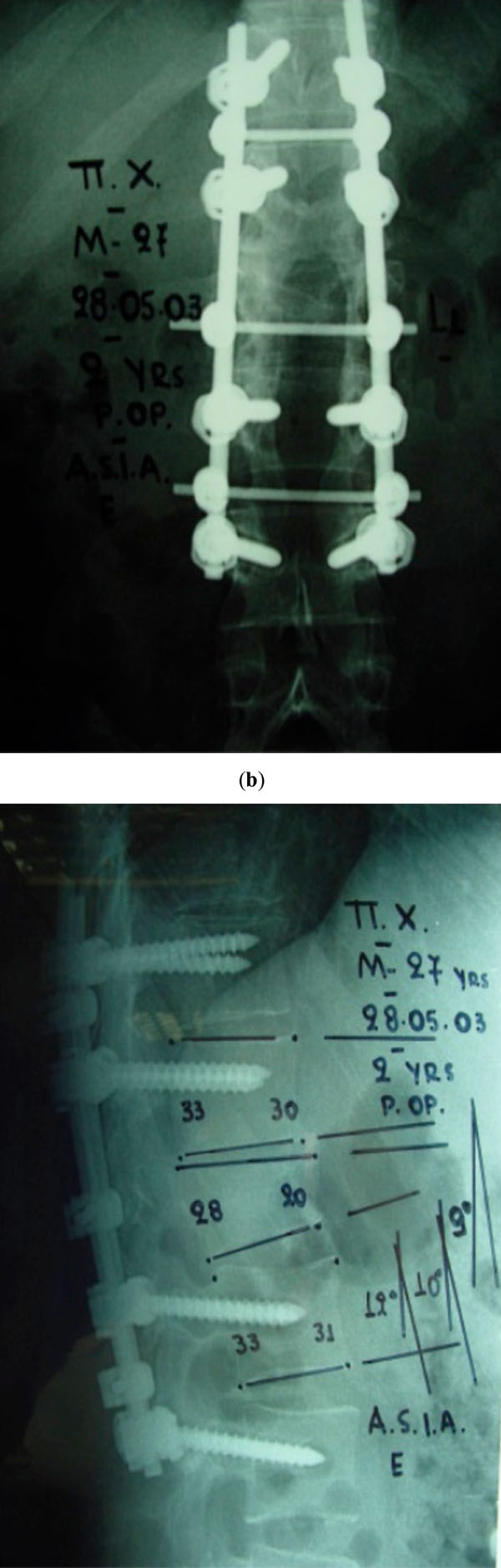
(a, b). Anteroposterior and lateral radiographs showing a Long-segment instrumentation system.
Screws which were used were forty or forty-five millimeters long depending on the level and size of the vertebra. Screws with diameter five and a half millimeters were used caudally to the eleventh thoracic vertebrae level. The instrumentation was applied bilaterally and cross-links (transverse traction devices) were placed cephalad and caudal to the fracture in order to augment the torsional rigidity. Laminectomies were performed in 10 patients with SS screw constructs and in 15 patients with LS screw constructs. Laminectomy performed in cases with severe neurological deficit (Frankel A, B, C), in order either to excise the retropulsed bone fragments or the disc remnants from the spinal canal or to push them back into the vertebral body. Grafts have been used one level above and one below the fractured vertebra. Autologous graft or frozen femoral heads was the most used grafts. All patients were managed postoperatively with immobilization in a custom-molded thoraco-lumbo-sacral brace for three months.
Radiographic and clinical outcome of 50 patients who was operated due to a thoracolumbar burst fracture was evaluated. The Low Back Outcome Score (LBOS) was used for the clinical evaluation of the patients [3]. According to LBOS, overall scores can vary from 0 (very disabled) to 75 (not at all disabled). The patients were placed in one of four outcome categories depending on their overall pure scores: 65 or higher (excellent), 50-64 (good), 30-49 (fair), 29 or lower (poor). Neurological recovery or functional result, were not objectives of this study.
Radiographic Measurements
Patients were followed up with physical examination and X-Ray imaging using a lateral radiograph cantered on the fracture level. Progressive deformity was considered as the change of the sagittal alignment of the spine comparing the initial post-operative weight-bearing radiograph to the most recent radiograph of the follow up. This progression was considered to be absent, minor, or major. A 5 to 10 degrees increase of the kyphosis was defined as minor progression; an increase of more than 10 degrees was defined as major progression. Successful instrumentation was considered when solid fusion without progressive deformity or failure of the implant was achieved. Failure or bending of the implant, or development of major kyphosis before fusion was occurred, were considered as failure of the fixation regardless of the duration of the follow-up.
All the radiographic measurements were taken preoperatively (pre-op), postoperatively (post-op) and at the time of latest follow up, except for the intervertebral motion, which was measured only at the follow-up. Local kyphosis angle of the vertebral body (Cobb angle) was measured as the angle between the superior and the inferior vertebral endplate. Segmental kyphosis was measured as the angle between the inferior endplate of the superior adjacent vertebral endplate and the superior endplate of the inferior adjacent vertebra. This method of measurements incorporates both discs in the instrumented spine section. Overall disc height was defined as the average of anterior and posterior disc height (Beck index). Follow-up measurements were expressed in relation to disk height immediately after the operation.
Statistical Analysis
All analyses were conducted using the SPSS, version 11.00 (SPSS Inc., Chicago, IL, USA). Two-factor mixed factorial ANOVA was used to examine the interaction between the type of stabilization factor and time factor. One factor Repeated Measures ANOVA model was used for the comparison of different time measurement of radiological parameters for each group. Pair wise multiple comparisons were performed using the method of Tukey critical difference. The percentage change of some parameters comparing them with the preoperative values was analysed using the Mann-Whitney test. The mean absolute change observed between preoperative, postoperative and the latest follow up values was statistically analysed by means of analysis of covariance using as dependent variable the absolute change of preoperative radiological parameters and follow up measurements as covariates. In addition, 95% confidence intervals for pair wise differences between types of stabilization means were calculated. Comparison of categorical data between groups was performed using chi-square test. The level of statistical significance was set at p < 0.05.
RESULTS
Patient demographic data is summarized in Table 2. There is no significant difference between the two groups concerning age and gender (p = N.S). The average operative time was 170min (Range, 140-220min) and the average blood loss was 1050ml (Range, 350-1800ml) for the SS pedicle instrumentation and 220min (Range, 190-300min) and 1200ml (Range, 550-2100ml) for the LS pedicle instrumentation respectively. There is a statistically significant difference between the two groups as far as the duration of operation and the blood loss are concerned (p < 0.005). On the opposite, comparing the LBOS between the two groups no significant difference is found (p = N.S). There is homogeneity between the SS pedicle instrumentation versus LS pedicle instrumentation of LBOS four categories: Poor, (5% vs 0%); Fair, (30% vs 30%); Good, (45% vs 53.3%); Excellent, (20% vs 16.7%).
Demographic Data of the Patients
| Group 1 SS | Group 2 LS | |
|---|---|---|
| Number of patients | 20 | 30 |
| Median age (years) | 33 (13-52) | 35 (17-55) |
| Male/Female | 12/8 | 20/10 |
The summary of radiographic data preoperatively, postoperatively, and at the latest follow-up for the group 1 (Short-segment pedicle instrumentation) and the group 2 (Long-segment pedicle instrumentation) are presented in Table 3.
Table 4 shows the three under comparison variances (Cobb angle, kyphotic deformation and Beck index) preoperatively, postoperatively and at the latest follow-up for each group separately and their fluctuation from preoperatively to postoperatively and preoperatively to the latest follow-up. Table 4 also shows the comparison of these variances between the groups.
Cobb Angle, Kyphotic Deformation and Beck Index Preoperatively, Postoperatively and at the Latest Follow-Up, for Short-Segment and Long-Segment Instrumentation Group. The Change of the Variables is Compared Between the Two Groups of Patients
| Cobb Angle | Kyphotic Deformation | Beck Index | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | p-Value | Mean | SD | p-Value | Mean | SD | p-Value | |
| Pre-op | |||||||||
| Short-segment | 17.0 | 7.0 | N.S | 4 | 9 | N.S | 0.6 | 0.1 | N.S |
| Long-segment | 17.5 | 6.8 | 4.5 | 8 | 0.6 | 0.1 | |||
| poST-op | |||||||||
| Short-segment | 5.0 | 3.5 | 0,051 | -9 | 4 | N.S | 0.92 | 0.2 | N.S |
| Long-segment | 3.0 | 2.0 | -8 | 4 | 0.94 | 0.2 | |||
| follow-up | |||||||||
| Short-segment | 8.5 | 6.0 | Ν.S | 4.5 | 4 | < 0.0005 | 0.90 | 0.2 | N.S |
| Long-segment | 6.0 | 4.0 | 40 | 15 | 0.92 | 0.2 | |||
| Cobb angle | Kyphotic deformation | Beck index | |||||||
| Median (%) | p-Value | Median (%) | p-Value | Median (%) | p-Value | ||||
| Comparison between pre-op and post-op | |||||||||
| Short-segment | -70,6% | Ν.S | -330% | Ν.S | -53% | Ν.S | |||
| Long-segment | -82,9% | -277% | -56% | ||||||
| Comparison between pre-op and follow-up | |||||||||
| Short-segment | -50% | 0.03 | 11% | < 0.0005 | -50% | Ν.S | |||
| Long-segment | -65,7% | 788% | -49% | ||||||
The two types of stabilization are compared in relation to the Cobb angle at each time point using the two-way mixed ANOVA model. There is a statistically significant difference for the Cobb angle between the two types of stabilization postoperatively (p = 0.051). The percentage change of the Cobb angle between these types of stabilization from preoperatively to postoperatively and from preoperatively to the latest follow-up was examined using the Mann-Whitney test. As far as this percentage change is concerned, there is a statistically significant difference between these two types of stabilization from preoperatively to the latest follow-up (p = 0.03), but there is no statistically significant difference from preoperatively to postoperatively.
The same method was used in order to study the kyphotic deformation. Thus, using the two-way mixed ANOVA model and comparing this variable for the two types of stabilization at each time point, a statistically significant difference (p < 0.0005) is found for the LS instrumentation group at the latest follow-up. Mann-Whitney test used in order to compare the median percentage change of the kyphotic deformation between the two different types of stabilization from preoperatively to postoperatively and from preoperatively to the latest follow-up. A statistically significant difference is observed for the LS group only from preoperative to the latest follow-up (p < 0.0005).
The third variable studied is the Beck index. Thereby, the two types of stabilization are compared using the two-way mixed ANOVA model at each time point, but there is no statistically significant difference of this index at any point studied (preoperatively, postoperatively and at the latest follow-up). Moreover, there is no statistically significant difference when the percentage change of the Beck index for each type of stabilization is compared, using the Mann-Whitney test, neither from preoperatively to postoperatively nor from preoperatively to the latest follow-up.
Eventually, the absolute change for each variable is presented in Table 5. The change of each index from preoperatively to postoperatively and from preoperatively to the latest follow-up is compared for each type of stabilization, considering the preoperative measurement as covariate and using the analysis of covariance model. As far as the Cobb angle is concerned, a statistically significant difference exists between the two groups, from preoperatively to the latest follow-up (p = 0.04) but there is no respective difference between the preoperative value to the postoperative one. Using the same analysis model and comparing the absolute change of the kyphotic deformation between the two under study groups, a statistically significant difference for the LS group from preoperatively to the latest follow-up (p < 0.0005) is ascertained, but no statistically significant difference from preoperatively to postoperatively be noted. Likewise, there is also no statistically significant difference between the two groups comparing the absolute change of the Beck index with the analysis model mentioned above.
Change of the Absolute Value of Cobb Angle, Kyphotic Deformation and Beck Index a) from Preoperatively to Postoperatively and b) from Preoperatively to the Latest Follow-Up, Considering the Preoperative Measurement as Covariate and Using the Analysis of Covariance Model
| Pre-Op vs Post-Op | Pre-Op vs Follow-Up | |||
|---|---|---|---|---|
| Adjusted Mean Change-95%CI | p-value | Adjusted Mean Change-95%CI | p-Value | |
| Cobb angle | ||||
| Short-segment | -11.88 (-15.6/-7.3 ) | N.S | -8.3 (-5.1/-11.6) | 0.04 |
| Long-segment | -14.1 (-10.1/-18.2) | -11 (-7.4/-14.6) | ||
| Kyphotic deformation | ||||
| Short-segment | -13,2 (-18.2/-8.2) | N.S | 0,5 (-2/+3) | <0.0005 |
| Long-segment | -12,7 (-18.5/-6.3) | 35 (-5/+75) | ||
| Beck index | ||||
| Short-segment | 0,31 (0,2/0,4) | N.S | 0,30 (0,2/0,4) | N.S |
| Long-segment | 0,32 (0,2/0,4) | 0,31 (0,2/0,4) | ||
In terms of the implant failure, three screws (three patients) were broken and four screws (four patients) were bent in the SS segment group. On the opposite, in the LS pedicle instrumentation group, no implant failure was observed. The vast majority of the patients refused to remove the implants. Six patients had their instrumentation removed after an average of 2 years (range 9 to 35 months) after the accident. No other complication was occurred.
DISCUSSION
It is widely accepted that thoracolumbar burst fractures should be addressed surgically [6-3]. The goals of the treatment of thoracolumbar fractures, regardless of the selected method, are the restoration of the stability of the vertebral column and the decompression of the spinal canal, leading to earlier mobilization of the patient. However, the treatment of thoracolumbar burst fractures remains a controversial issue. Short-segment pedicle fixation is a popular option. Dick et al. [14], have developed the SS stabilization for the operative treatment of thoracolumbar and lumbar fractures. However, there is a controversy as far as the results of this instrumentation are concerned. There are studies that report high rate of failure because of proximal screw pullout, screw breakage, and loss of correction even if material failure does not always affect the clinical outcome [6,7,15,16]. Nevertheless, some studies demonstrate that clinical long-term results are favourable in patients who underwent SS pedicle instrumentation [17, 18]. In attempt to achieve a stiffer construct, within the limits of a SS fixation, several technical issues have been described, including addition of cross-links and supplemental hooks at the levels of the screws [19-22]. Many authors suggest that SS transpedicular instrumentation is the best option for unstable low lumbar fractures. Their advantage is that the loss of the lumbar lordosis associated with flat back syndrome can be avoided [5, 23].
Significant correction loss and failure is also noted in the LS (greater than two segments) instrumentation with two-level fixation. Sasso and Cotler used this method, which failed at 12 months follow-up [12]. Verlaan et al. [24], reviewed 132 papers, published within a 30-year period (1970-2001), for studying the surgical outcome of this instrumentation in the management of thoracic and thoracolumbar fractures and its complications rates. Most of these papers are retrospective studies which examine different types of implants and different surgical techniques. Moreover, there are inequities as far as the severity of the injury is concerned between the divided groups. Eventually, no difference found between the outcomes of patients treated with long constructs compared to them who treated with short constructs. Additionally, pedicle screws fixation needs more time to perform than hook fixation. Regarding to the complications, a low rate of complications and a very low rate of serious complications was reported. The time needed for returning to work and the pain that these patients suffered seemed to be better than the general belief.
McLain [25] studied patients with severe spinal fractures treated with segmental fixation and found that those who had treated with long surgical reconstructions had not more impairment than those who had treated with shorter constructs and less dissection. The advantages of segmental instrumentation that used in this study is the immediate mobilization of patients with less dependence on bracing, the distribution of corrective forces over multiple levels and the reduction of the likelihood of implant failure, which is a common complication of Harrington rod constructs.
Serin et al. [1], reported that four levels posterior fixation is superior to two levels posterior fixation and that this fixation is more stable when using an accessory offset hook. Tezeren et al. [26] demonstrated that final outcome regarding sagittal index and anterior body compression is better in the LS instrumentation group than in the SS instrumentation group.
The aim of the current study is to compare the SS fixation to LS fixation as far as the surgical correction is concerned. These surgical methods were compared using the statistical analysis of specific indexes (Cobb angle, kyphotic deformation and Beck Index) in order to investigate which technique gives better results according to these indexes.
Our experience showed that the majority of the problems related with fixation and instrumentation failure occurred when the injury was located at the first or second lumbar vertebra level. This observation is consistent with the higher injury prevalence at these levels, but it may also reflect a greater degree of instability at these levels.
In seven patients included in the SS pedicle construct group, the loss of correction was in the range of the initial reposition. Broken and bended screws were noted within the first year and probably were due to long term cyclic loading. Interestingly, implant failure was not related to apparent pseudarthrosis.
Two basic conclusions can be exported from this study. The first is that according to the statistical analysis using the Mann-Whitney test there is a significant difference for both the Cobb angle and the kyphotic deformation, between the two different under study groups. In the SS group, the median value of the Cobb angle at the latest of follow up is diminished 50 per cent from the value of this index postoperatively. In the LS group the respective change of the Cobb angle is 65.7 per cent (p < 0.05). The fluctuation of the median value of the kyphotic deformation from preoperatively to the latest follow up is 11 per cent in the SS group and 788 per cent in the LS group respectively (p < 0.0005). The second result exported from this study is that as far as the Beck index is concerned, there is no significant difference according to all the statistical tests used this study, indicating that this index is not reliable enough for the follow up of the patients suffered from similar fractures. Finally, no significant difference was found for all the indexes between their preoperative and immediate postoperative values.
The outcomes of the radiographic indexes studied (Cobb angle and kyphotic deformation) are better in the LS pedicle instrumentation group than in the SS pedicle instrumentation group implying that the LS instrumentation is more effective method for the management of the burst thoracolumbar fractures than the SS instrumentation. SS instrumentation seems to have higher rate of failure. However, this method has smaller operation time and less blood loss. As far as the clinical outcome of the patients according to LBOS is concerned, no statistically significant difference was note between the SS and LS instrumentation group. These results suggest that LS and SS stabilization are equivalently able in reducing the segmental kyphosis and the vertebral body deformation, however at the long term follow-up the LS stabilization was associated with better results concerning the radiological parameters and the patients’ satisfaction.


