All published articles of this journal are available on ScienceDirect.
Initial Evaluation on Subsidence of Cemented Collarless Polished Tapered Stem Applied to the Patients with Narrow Femoral Medullar Canal
Abstract
Purpose:
The geometry of the proximal femur is one of the important factors for choosing the suitable stem. We have been applied cemented collarless polished tapered (CPT) stem to the patients with small femur. Radiographic evaluation was performed to access the clinical feature of the stem in early stage of the follow-up.
Methods:
One hundred total hip arthroplasties with CPT system were performed between October 2004 to February 2006. This study focused on the 53 cases to whom size 1 or smaller sized stem were implanted, and its post-operative period was 41 months (30-46 months). Morphologic classification of preoperative proximal femur, stem alignment, thickness of the cement mantle, cementing technique, subsidence of the stem, improvement in the bone-cement interface, and stress shielding were assessed.
Results:
The size of the inserted stem was X-SMALL in one case, SMALL in two cases, SIZE 0 in 12 cases, and SIZE 1 in 38 cases. Canal shape of proximal femur was stovepipe type in five cases, normal type in 43 cases, and champagne-flute type in five cases. There was no subsidence in eight cases. 44 stems subsided within 1 mm, one stem subsided 1 to 2 mm, and no stem subsided over 2 mm. In 39 of 45 cases, subsidence was appeared within six months after operation. Marked progressive and excessive subsidence was not seen after the two years of follow-up.
Conclusions:
Short term radiographic results of THA with CPT stem to small femur were satisfactory with less unfavorable radiographic findings, which imply contribution to longer survivorship of the stem.
INTRODUCTION
The geometry of the proximal femur is one of the important factors for choosing the suitable cemented stem. It is well-known that some Japanese often have a smaller femur and narrower medullary canal compared with that of Western population [1]. We have applied cemented collarless polished tapered stem (CPT, Zimmer, Warsaw, USA) to the patients with narrow medullary canal. CPT stem has double taper and polished surface (Ra = 0.05 µm). The good clinical and radiological results of five-year follow-up have been reported recently [2]. The stem has wide-ranged size variation from XX-SMALL, X-SMALL, SMALL, SIZE 0, 1, 2, 3, 4, to 5. Our hypothesis was that the smaller sizes of collarless, tapered, polished stem of cobalt-chromium based alloy with strong mechanical property can be applied to the patients with narrow medullary canal and would present favorable initial radiographic findings to be anticipated the stability and longevity. In this study, morphological feature of proximal femur and short term radiographic findings were assessed in this study to reveal the correlation between the canal shape and radiographic result of CPT stem.
MATERIALS AND METHODOLOGY
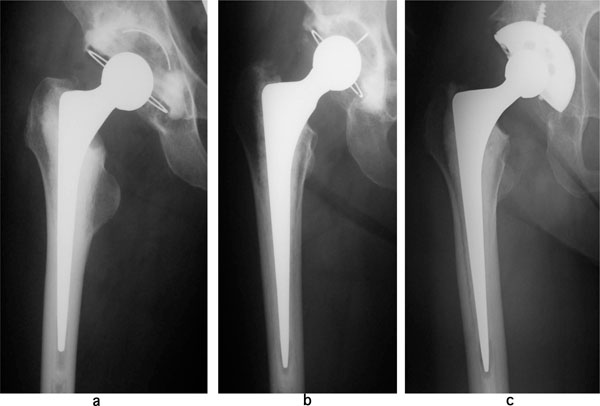
One hundred total hip arthroplasties with CPT system were performed between October 2004 to February 2006 at Department of Orthopaedic Surgery, Yamagata University School of Medicine and Saiseikai Yamagata Saisei Hospital. This study focused on the 53 joints to whom SIZE 1 or smaller sized stem were implanted. Forty-five patients were female (50 joints) and three were male (three joints). Mean age at surgery was 60.6 years (44-80 years), and mean body weight was 54.3 kg (37.2-75.0 kg), and its post-operative period was 41 months (30-46 months). Preoperative diagnosis was osteoarthritis in 46 cases, rheumatoid arthritis in one case, and rapidly destructive coxarthrosis in one case. All operations were performed by lateral position and postero-lateral approach. Forty of 53 cases were performed by consultant surgeon, nine cases were by junior surgeon, and one case was by resident surgeon. Acetabular reconstruction was performed with cemented cup (ZCA, Zimmer, Warsaw, USA) in 47 cases, cemented cup (FPW, JMM, Osaka, Japan) in one case, and cementless cup (Trilogy, Zimmer, Warsaw, USA) in five cases. CPT stem was inserted with distal centralizer after the filling the medullary cavity with bone cement (Endurance, DePuy, Leeds, UK), followed by proximal femoral pressurization. Anterior and lateral projection of radiographs were obtained before operation, just after operation, at three months, six months, one year, and yearly thereafter. Morphologic classification of proximal femur, as described by Noble et al. [3], was assessed from radiograph taken before operation (Fig. 1). Canal shape was classified by canal flare index, defined as ratio of the intracortical width of the femur at a point 20 mm proximal to the lesser trochanter and at canal isthmus. Canal flare index of less than 3.0 described stovepipe, 3.0-4.7 was normal and 4.7-6.5 was champagne-flute. Stem alignment, thickness of the cement mantle and cementing technique, as described by Barrack et al. [4], were assessed in all the 14 zone of Gruen et al. [5] and from radiographs taken just after operation. The proximal femur was delineated into 1-7 zones from the anteroposterior radiographs and 8-14 zones from lateral radiographs. As for cementing technique by Barrack, so-called white-out at the cement-bone interface was defined as grade A, the presence of slight radiolucency of the cement-bone interface was defined as Grade B, the presence of radiolucency involving 50% to 99% was defined as Grade C, and the presence of radiolucency involving 100% in any injection, or a failure to fill the canal with cement such that the tip of the stem was defined as Grade D. Subsidence of the stem was evaluated according to the method described by Fowler et al. [6]. The amount of the subsidence was evaluated by measurement of lucent line that appeared between stem and cement in the part of so-called “the shoulder” of the stem (Fig. 2). When cement was absent at the shoulder of the stem, the amount of stem tip migration in centralizer was measured. Improvement in the bone-cement interface, which can be seen as an increase in the density of the cancellous bone, described by Wroblewski et al. [7] which based on subjective view, although quantitative analysis such as DEXA or CT was not performed. This type of analysis would be required for further analysis in this type of study. All assessments were performed with radiographs taken at least two years after operation. Cortical hypertrophy and fracture of cement mantle, correlation between canal shape and cement technique, and degree of subsidence were evaluated. Correlation between improvement in the bone-cement interface and gender, age, body weight was also assessed. Chi-square test, Fisher’s exact probably test, and Mann-Whitney U test were used for statistical analysis. A value of p < 0.05 was considered to be statistically significant.

Canal shape and proximal femur. Canal shape was classified by canal flare index, defined as ratio of the intracortical width of the femur at a point 20 mm proximal to the lesser trochanter and at canal isthmus. (a): stovepipe (canal flare index < 3.0), (b): normal (3.0-4.7), (c) champagne-flute (4.7-6.5).
Subsidence in the shoulder of stem. (a): no subsidence, (b): 0-1 mm subsidence, (c): 1-2 mm subsidence.
This study was approved by the institutional review board (IRB) and the patients were informed that data from the case would be submitted for publication, and gave their consent.
RESULTS
The stem size was distributed as X-SMALL in one case, SMALL in two cases, SIZE 0 in 12 cases, and SIZE 1 in 38 cases in order of a smaller size. Canal shape of proximal femur was evaluated by a parameter called canal flare index [2]. The average of canal flare index was 3.8±0.8 and stovepipe type was found in five cases (9.4%), normal type in 43 cases (81.2%), and champagne-flute type in five cases (9.4%) (Table 1). Stem alignment was 3° of valgus to 3° of vs in the antero-posterior plane, and its mean value was 0.1 ± 1.4° of vs position. In the lateral plane, stem alignment was 4° of anterior to 4° of posterior, and its mean value was 0.9 ± 1.7° of posterior position. The average thickness of cement mantle at zone 2, 3, 5, and 6, was 2.2 ± 0.6 mm (1-4 mm). The average thickness of cement mantle at zone 1 and zone 7 was 4.7 ± 2.5 mm (1-12 mm) and 7.1 ± 3.0 mm (2-15 mm). As for cementing technique, grade A was seen in 27 cases (51%). Grade B was seen in 18 cases (34.0%). Grade C was seen in eight cases (15.1%). Grade D was not seen (Table 2). Two of five cases, which shape of proximal femur was stovepipe, were grade C. Subsidence of the stem, which indicated “creep” phenomenon of the bone cement and stress relaxation by taper slip mechanism, was found in 45 cases (84.9%) at two year after operation, but eight cases (15.1 %) did not show subsidence. All subsidence was seen at stem-cement interface. Forty-four stems (83.0%) subsided within 1 mm, one stem (1.9%) subsided 1 to 2 mm, and no stem subsided over 2 mm. In 26 cases of 45 cases (57.8 %) which the subsidence was seen subsided within three months, 13 cases (28.9 %) subsided within six months, four cases (8.9 %) subsided within one year, and two cases (4.4%) subsided within two years (Fig. 3). In 39 of 45 cases (86.7 %), subsidence was appeared within six months after operation. Marked progressive and excessive subsidence was not seen after the two years of follow-up. As for the relationship to the canal shape, subsidence of the stem (0-2 mm) was found in three cases (60%) in stovepipe, 39 cases (90.7%) in normal, and three cases (60%) in champagne-flute, whereas, no subsidence was in two cases (40%) in stovepipe, eight cases (9.3%) in normal, and two cases (40%) in champagne- flute, respectively (Table 3). There was no significant difference (p = 0.051). In relationship to the cementing technique, subsidence of the stem (0-2 mm) was found in 23 cases (85.2%) in Barrack A, 16 cases (88.9%) in Barrack B, and six cases (75.0%) in Barrack C, but no subsidence was seven cases (14.8%), two cases (11.1%), three cases (25.0%), respectively. There was no significant difference (p = 0.658), but one case with grade C cementing technique showed subsidence of 1-2 mm (Table 4). Furthermore, there was no significant difference (p = 0.5) between subsidence and the thickness of cement mantle. There were six cases with less than 2 mm of cement mantle and subsidence was 0-1 mm in all cases. However, the number of cases will be increased in future, and there is a possibility that significant difference will be appeared. The limitation in this study is that evaluating factors which relates to the subsidence of the stem, such as the canal shape, the cement technique, and the cement mantle, are very limited and somewhat insufficient. It is important to evaluate detailed bone quality and the background of the patients before operation. A lot of factors might relate to the subsidence of polished stem. As for the relationship between cementing technique and canal shape, Barrack type C was found in two cases (40%) in stovepipe, six cases (14%) in normal, and none (0%) in champagne-flute. There was no significant difference (p = 0.49), but Barrack C was frequently found in stovepipe type femoral canal (Table 5).
Canal shape of Proximal Femur
| Canal Shape | Number (%) |
|---|---|
| stovepipe | 5 (9.4) |
| normal | 43 (81.2) |
| champagne flute | 5 (9.4) |
Cementing Technique
| Barrack | Number (%) |
|---|---|
| grade A | 27 (50.9) |
| grade B | 18 (34.0) |
| grade C | 8 (15.1) |
| grade D | 0 |
Subsidence (mm) and Canal Shape
| Subsidence (mm) | Stovepipe | Normal | Champagne-Flute |
|---|---|---|---|
| 0 | 2 | 4 | 2 |
| 0-1 | 3 | 38 | 3 |
| 1-2 | 0 | 1 | 0 |
Subsidence (mm) and Cementing Technique
| Subsidence (mm) | Barrack | ||
|---|---|---|---|
| A | B | C | |
| 0 | 4 | 2 | 2 |
| 0-1 | 23 | 16 | 5 |
| 1-2 | 0 | 0 | 1 |
Cementing Technique and Canal Shape
| Barrack | Stovepipe | Normal | Champagne-Flute |
|---|---|---|---|
| A | 2 | 22 | 3 |
| B | 1 | 15 | 2 |
| C | 2 | 6 | 0 |
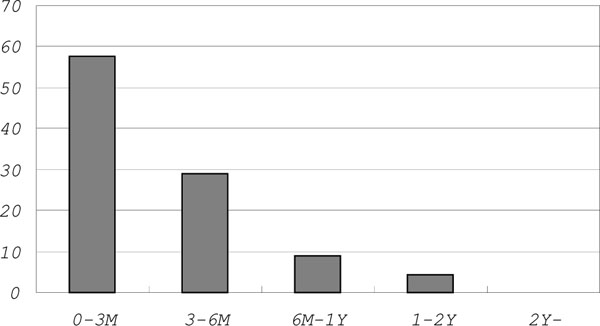
First appearance of stem subsidence (%).
Improvement in the bone-cement interface was seen in three cases (5.7%) at zone 7, and two of them were male. There was a significant difference in gender (p = 0.006), but no differences in age (p = 0.55) and body weight (p = 0.06). Cortical hypertrophy was found in one case; however hypertrophy did not accompany any clinical symptom. There was no fracture of cement mantle.
DISCUSSION
CPT stem was designed based on taper-slip principle [8]. The feature allows subsidence at stem-cement interface [9, 10]. Stem subsidence has been considered as a result from creep of bone cement and stress relaxation [11], which could minimize cement damage. Gellar et al. [12] had reported femoral stem was subsided within the first six months after implantation by RSA study. The limitation in this study is that evaluation of the subsidence was semiquantitative analysis although it is important to assess quantitatively accurate change by EBRA or RSA. In this study, stem subsidence was found already in 26 of 53 cases (49.1%) at three months and in 39 cases of 53 cases (73.6%) at six months. This result was similar to their reports. The amount of subsidence was almost within 1 mm and no case showed progressive and excessive subsidence. Yates et al. [2] had reported that subsidence was related significantly to cement mantle defect. In our study, subsidence was not related to age (p = 0.31), body weight (p = 0.12), canal shape and cementing technique, but one case with normal type medullary canal and grade C cementing technique showed subsidence of 1-2 mm. There was no clinical problem for the short term observation.
Total hip arthroplasties to the patients with small femur and narrow medullary canal is technically difficult. Chiu et al. [13] had reported that incomplete cement mantle (discontinuity or less than 2 mm) was a factor of poor clinical results in Exeter stem to small femur. In our series, the mean thickness of minimum cement mantle at zone 2,3,5, and 6 was 2.2 mm (1-4 mm) and the mean thickness of cement mantle at zone 1 and zone 7 was 4.7 ± 2.5 mm (1-12 mm) and 7.1 ± 3.0 mm (2-15 mm). It seemed sufficient to obtain adequate thickness for narrow medullar canal. As for the relationship between cement mantle and subsidence, subsidence of the stem (0-2 mm) was found in six cases (11.3 %) with less than 2 mm of cement mantle, in 0 case (0 %) with more than 2 mm, whereas, no subsidence was in eight cases (15.1 %) with less than 2 mm of cement mantle, in 39 case (73.6 %) with more than 2 mm. There was no significant difference (p = 0.57). Yates et al. [14] was reported 14 cases with fracture of modern high nitrogen stainless steel cemented stem. They reported careful consideration and attention to technique is required to the patients with high body weight and small femur with champagne-glass canals.
When load is applied to the polished and tapered stem, radial compressive forces are created and transferred to bone as hoop stress. It can be seen as an increase in the density of the cancellous bone. Wroblewski et al. [7] showed apparent improvement in the bone-cement interface in 20% of hips at a mean follow-up of three years. In our cases, an increase in the density of the cancellous bone was seen in three cases (5.7%) at zone 7, and two of three cases were male. There was no significant difference between these three cases and other 50 cases about age (p = 0.55) and body weight (p = 0.06). The incidence of improvement in the bone-cement interface was smaller than the report of Wroblewski. In the report, there were 262 female and 193 male, and their mean age was 53.7 years, and mean body weight was 72 kg. There was apparent difference regarding background of patients between two studies. Characteristics of patients, such as bone quality, gender, age, body weight and activity of the patient, were not significant contributing factors to improve bone-cement interface in our present study. However, significant correlation between body weight and improvement in the bone-cement interface might become apparent, if number of patients of the series increase in the future.
The CPT femoral prosthesis is made of the cobalt-chrome-molybdenum (Co-Cr-Mo) alloy, and its mechanical strength combined with polished surface is better than the other alloys. Based on such mechanical property, we considered that smaller sized CPT stem was possible to be applied to small and or narrow medullary canal of femur with cement fixation. Harald et al. [15] reported on clinical use of small stem total hip arthroplasties. In the report, clinical results of off-the-shelf stem, custom-made stem with or without cement were compared. Their implant survivorship at 15 years with small cemented off-the shelf Weber curved stem was 90 % which equaled results of the large stem. Although the number of patients was small and follow-up period was short in this study, continuous follow-up will make it possible to strengthen the clinical results and to compare with other type of stems in the future.
CONCLUSION
In this study, morphological feature of proximal femur and short term radiographic findings were assessed to reveal the correlation between the canal shape and radiographic result of cemented CPT stem to the patients with small femur. Radiographic assessment showed satisfactory short-term outcome with less unfavorable radiographic findings, which imply contribution to longer survivorship of the implant.
The authors did not receive and will not receive any benefits and or funding from any commercial party related directly or indirectly to this manuscript.


