All published articles of this journal are available on ScienceDirect.
Multifocal Infection After Hip Fracture Fixation: A Case Report
Abstract
We present the case of a seventy five year old female diabetic patient, who sustained an inter-trochanteric fracture of her left hip and was treated by dynamic hip screw fixation on the same day. The patient developed multifocal infection with three different and unusual types of bacteria isolated in blood and wound cultures. In spite of aggressive and repeated wound debridement, infection and blood sugar levels were impossible to control until metal removal, which led to fracture malunion. The patient denied further hip reconstruction surgery and ended up mobilizing with a walker and a limp.
Multifocal infection is possible even after a routine Orthopaedic procedure on a patient with precipitating factors no more than diabetes mellitus. It is important to be aware of the possibility of simultaneous wound infection and septicemia by different agents.
CASE REPORT
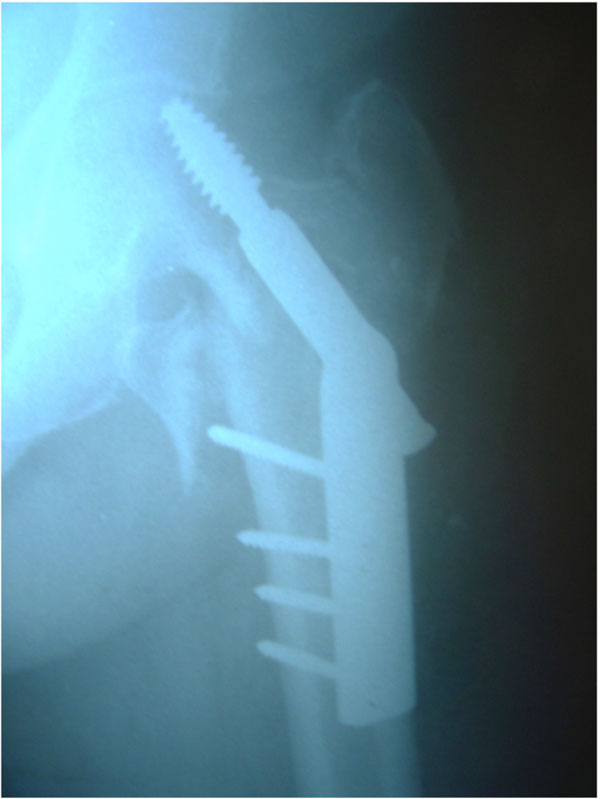
A seventy five year old female diabetic patient sustained an inter-trochanteric fracture of the left hip (Fig. 1) and underwent surgery on the same day, by means of dynamic hip screw fixation (Fig. 2). The patient was otherwise in good health with no prior active infection of any system. She was transfused with three units of blood and mobilized on the second post-operative day. Routine antibiotic prophylaxis (Cefuroxime i.v, 750 mg tds) was administered and stopped on the second postoperative day [1]. Her bladder was catheterized on the first postoperative day because of incontinence. She was afebrile until the fourth postoperative day when her temperature started to rise up to 38.5 0C. Though her wound appeared quiet, there was constant discharge of a blood stained, thick fluid through the holes of the drains, which had been removed on the second postoperative day. The elevated temperature continued and the fever became septic on the eighth post-operative day. Her wound was therefore opened and debrided thoroughly on the ninth postoperative day. No pus was found, but multiple cultures taken from the wound showed growth of staphylococcus epidermis and enterococcus faecalis. At the same time blood cultures were positive for bacteroides fragilis. Except for the staphylococcus, the rest of the infective agents were extremely rare both in our unit and hospital. At that point her condition became critical, with continuous temperatures of 40 0C. Her further treatment required i.v. administration of multiple combinations of antibiotics (Table 1) and several surgical debridements in an attempt to control infection and maintain the internal fixation until fracture union. At the same time control of her blood sugar levels was found to be impossible, with values exceeding 300mg/dL. Her general condition greatly improved, but progressively the implants became loose and two months postoperatively an eminent cut out was seen on x-rays (Fig. 3). Implant removal at this stage, led to complete control of the infection and blood sugar levels, but the fracture united in varus (Fig. 4). The patient denied further hip reconstruction surgery and ended up mobilizing with a walker and a limp.

Intertrochanteric fracture of the Lt hip.

DHS fixation of the fracture.
Implant loosening, lag screw cut out.

Fracture malunited in varus
Antibiotics Administered During Treatment of Multi Focal Infection
| Cefuroxime |
| Imipenem and Cilastatin |
| Amikacin |
| Metronidazole |
| Linezolid |
| Netilmicin sulfate |
| Vancomycin |
| Ampicillin |
| Ciprofloxacin |
DISCUSSION
Deep wound infection after routine Orthopaedic trauma surgery, such as dynamic hip screw fixation of an intertrochanteric fracture is a rare but well known and devastating complication [2]. It has been reported that deep infection after a hip fracture operation not only impairs the functional outcome but also increases the mortality rate by 10% [3]. Early diagnosis and aggressive treatment of implant-related infection with antibiotics, debridement, and maintenance of stable internal fixation are essential to successful treatment [4]. Unfortunately, it appears that this is not always possible. Reviewing the literature we were unable to find a case similar to ours, with septicaemia and wound infection due to different infective agents. We did find though a case where osteoarticular tuberculosis occured after dynamic hip screw fixation of a pertrochanteric fracture in a patient with no history of tuberculosis, pulmonary or extra pulmonary [5].
CONCLUSIONS
Multifocal infection is possible even after a routine Orthopaedic procedure on a patient with precipitating factors no more than diabetes mellitus. Blood transfusion (in spite of controversy in the literature) [6, 7] and urinary catheterization [8] can be serious risk factors and should be performed only when absolutely necessary. It is important to be aware of the possibility of simultaneous wound infection and septicemia by different agents. Great illness and septic fever with mild discharge from an otherwise inconspicuous wound should make surgeons suspicious. Rarely encountered bacteria can be the causative factor. Complete control of the wound infection appears to be impossible until implant removal, even after early, aggressive and repeated surgical debridement.


