All published articles of this journal are available on ScienceDirect.
Re-evaluating Cartilage Defect Measurement Methods and Standard Surgical Thresholds: An Opinion Piece
Abstract
Cartilage lesion size is an essential component in treatment algorithms for various therapeutic and surgical interventions. Obtaining accurate and precise measurements is critical to formulating a comprehensive treatment plan. Standard measurement methods overestimate lesion size due to inadequate shape evaluation. Furthermore, currently accepted surgical intervention thresholds are elevated beyond the level at which rim stress demonstrates significant load distribution within the knee. Based on the current literature, evaluating a chondral lesion based on the oval area proved to be a novel proposition. The excess area (EA) that accounted for in following the rectangular area (RA) measurement method is described by the following equation: EA
 0.858 (r1 x r2). Furthermore, the EA occupies roughly 21.45% of the defect area regardless of lesion size.
0.858 (r1 x r2). Furthermore, the EA occupies roughly 21.45% of the defect area regardless of lesion size.
Additionally, the lesion size threshold within the knee has significant implications beginning at 1cm2, as opposed to the currently accepted surgical threshold of 2cm2. However, how cartilage defects are measured needs to be rooted in more scientific and precise manners to best aid in clinical and pre-operative decision-making. Utilizing the alternative measurement method, surgeons can make more informed treatment plans with each patient. While the decision to treat cartilage defects is multifactorial, surgical intervention algorithms should be re-evaluated, provided the refined measurement methods and newer threshold recommendations.
1. INTRODUCTION
Articular cartilage is one of the quintessential components of standard joint physiology that allows for seamless movement in everyday life. The effortless gliding within the joint capsule largely goes unappreciated until it is damaged in isolation or conjunction with bone deformities, ligament injuries, and traumatic collisions, a prognosis that can be symptomatically similar to osteoarthritis [1-11]. Osteochondral defect size is an integral component in every algorithm of decision-making pertaining to the treatment plan devised for each patient [4, 10]. While an accurate lesion size is obtained intra-operatively following debridement, the measurements taken from pre-operative radiography, primarily from magnetic resonance imaging (MRI), are the predominant method of assessment [2]. Since chondral defect size is a critical determinant in treatment planning, obtaining an accurate measurement is necessary to provide patients with the best treatment regimen possible.
Under current practices, osteochondral defect sizes are two-dimensional measurements taken by the standard area of a square through the equation of length times width [3]. While this methodology provides a quick and preliminary size calculation, it is ineffective in estimating overestimating defect size in non-rectangular-shaped lesions. Due to this, the utilization of a flawed measurement method in treatment algorithms is compromised. When examining various treatment algorithms, the cut-offs for intervention reveal that there are different recommended treatments that are predominantly dependent upon lesion size [6, 12-15]. Therefore, having an altered measurement from a defect size that includes additional area from improper area evaluation can impact treatment protocol.
Due to the vast nature and variety of cartilaginous lesion shapes that can present in vivo, there is a recognition that taking measurements as accurately and precisely as possible is to the benefit of the patient and surgical team as a whole. If lesion size is determined to be altered from the initial pre-operative assessment, it could potentially introduce added delays and complications to the case as a result of the need for increased graft material or varying graft harvest location. This is the basis for this article, which evaluates the impact that incorrect measurement of articular cartilage damage can have on the overall lesion size calculated and opens the discussion pertaining to alternative measurement methods and algorithm thresholds surrounding cartilaginous defects in the human knee.
2. DISCUSSION
Following a patient presentation of generalized knee pain, tenderness, swelling, and locking, MRI imaging is the superior evaluation for suspected cartilage and soft tissue morphology [5]. Evaluating the cartilaginous surfaces for defects along the distal femoral medial and lateral condyles, in which the medial condyle shows a statistically significant increase in peak rim stress values compared to the lateral condyle [6], proximal tibial condyles, and posterior patellar surface, is necessary. Through this, apparent lesions are observed and subsequently measured to assess the defect area. Regardless of which treatment algorithm a surgeon utilizes, one component is universal in treatment technique consideration, i.e., lesion size. Other attributes follow closely behind, such as lesion location, subchondral bone involvement, and the latest vetted level of evidence [7]. Therefore, an accurate assessment of the lesion size via pre-operative MRI is imperative in refining patient treatment.
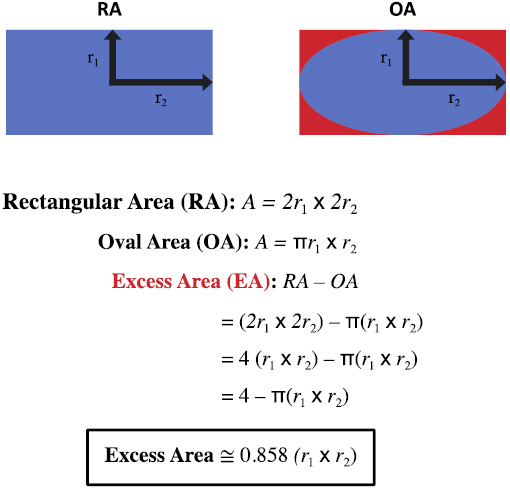
Mathematical assessment of the current cartilage defect measurement method via rectangular area (RA) compared to the alternative defect measurement method via oval area (OA). The difference between RA and OA is taken to be the excess area (EA). The resultant equation indicates the additional area in the figure above shaded red that is accounted for when the RA method is utilized.
Under current practices, osteochondral defects are measured two-dimensionally, taken by the area of a square through the equation of length times width [3]. The surgeon utilizes the resultant to evaluate the best course of treatment provided for each patient's unique presentation. While this methodology of length times width measurement provides an accurate calculation of rectangular osteochondral lesions, it is problematic when applied to other morphologies of lesions that do not follow the standard rectangular outline. It would logically make sense to measure a circle as a circle and a square as a square. Therefore, the utilization of the area of an oval, A = Π r1 x r2 (Fig. 1), would be best utilized when the assessment of a circular osteochondral lesion is needed. Measuring a circular-based lesion through a rectangular method leads to immense over-measurement. The excess area that is included in these measurements is defined by the mathematical difference between the area of a rectangle and the area of an oval. Fig. (1) demonstrates this phenomenon of over-measurement shown by the space shaded in red, represented by the equation: Excess Area
 0.858 (r1 x r2). Subsequently, this becomes problematic for patient evaluation in the way of having an artificially inflated measurement for a component of treatment algorithms critical to decision-making. Furthermore, excess area, when taken as a proportion of the overall rectangular area, accounts for approximately 21.45% of the overall lesion size when utilizing the rectangular measurement method (Fig. 2). Through an analysis of the current literature surrounding osteochondral lesion size measurement via MRI in a pre-operative setting, defect measurement through a more shape-specific technique is a novel recommendation at this time.
0.858 (r1 x r2). Subsequently, this becomes problematic for patient evaluation in the way of having an artificially inflated measurement for a component of treatment algorithms critical to decision-making. Furthermore, excess area, when taken as a proportion of the overall rectangular area, accounts for approximately 21.45% of the overall lesion size when utilizing the rectangular measurement method (Fig. 2). Through an analysis of the current literature surrounding osteochondral lesion size measurement via MRI in a pre-operative setting, defect measurement through a more shape-specific technique is a novel recommendation at this time.
Following the acquisition of patient cartilaginous lesion size, treatment algorithms can be implemented to aid a surgeon in making the appropriate next steps. A review of the literature reveals that a vast array of threshold sizes are currently implemented in treatment algorithms for focal cartilage defects of the knee [12]. Most contemporary algorithms reference the “2 cm2” threshold when differentiating between treatment choices [6, 8, 9]. However, Guettler et al. concluded through a biomechanical cadaveric study that a significant rim stress increase is observed in osteochondral defects of the distal femoral condyles beginning at 1 cm2 [6]. Koh et al. verified this phenomenon by assessing the maximum contact pressure versus chondral defect size [13]. This investigation yielded results indicative of changing biomechanical parameters in defect sizes as small as 0.49 cm2 in full-thickness chondral defects [13].
3. LIMITATIONS
The shortcomings of this investigation are not without recognition. It should be noted that the basis of evaluation between rectangular and circular areas of articular cartilage lesions is based primarily on mathematical analysis instead of through a cadaveric assessment and measurement. These measurements are based on a two-dimensional assumption for simplicity and alignment with current clinical practice, whereas most lesions occur on rounded, three-dimensional surfaces and, therefore, will yield size discrepancies to those presented in this review. Furthermore, not all high-impact databases were utilized for this literature review, and therefore, there is the possibility of contrasting information in this article.

Mathematical assessment of the percentage of additional area composed within cartilage defect measurement through the RA method.
CONCLUSION
Obtaining a more accurate assessment of osteochondral defect size via pre-operative magnetic resonance imaging through circular size analysis will provide a more effective patient evaluation and treatment planning. The excess area accounted for when measuring focal cartilage defect size through the current rectangular methodology can be corrected by evaluating a circular lesion as a circle instead of utilizing the current rectangular method. Incorporating this novel osteochondral lesion measurement method into clinical practice may benefit clinicians' multifactorial decision-making treatment assessment process. Furthermore, the current treatment algorithms for tibiofemoral cartilage damage sizing implementation should take into consideration the evolving scientific findings of lesion size, such that modern literature suggests that significant stress concentration occurs far below the current thresholds utilized in most algorithms.
AUTHORS’ CONTRIBUTION
J.G.: Study conception and design; J.B.: Conceptualization; M.C.: Draft manuscript. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| MRI | = Magnetic Resonance Imaging |
| RA | = Rectangular Area |
| OA | = Oval Area |
ACKNOWLEDGEMENTS
Declared none.


