All published articles of this journal are available on ScienceDirect.
Improving Completion Rates of Orthopaedic Surgery Discharge Medication Reconciliation: A Quality Improvement Initiative
Abstract
Aim
Discharge Medication Reconciliation (DMR) is critical in the transition from inpatient to outpatient care. Incomplete or inaccurate DMR results in medication errors, polypharmacy, or missed medications. Our high-volume tertiary care orthopaedic division was identified as an underperformer in DMR. Therefore, this Quality Improvement initiative aimed to achieve >85% DMR completion at hospital discharge by June 30, 2023.
Methods
An interrupted time series study design, following the “Model for improvement” of the Institute for Healthcare Improvement, was used with a committee formed with CTU representatives, a resident, and two facilitators. Diagnostic tools, including root cause analysis, stakeholder interviews, process mapping, and driver diagrams, were employed. Multiple Plan-Do-Study-Act cycles were executed, along with interventions, such as audit and feedback and involvement of medical residents and nurse practitioners. Electronic medical record functionality was enhanced to facilitate medication reconciliation, with 'Continue all Remaining Home Medications'. In addition, for monthly data tracking, statistical process control charts were employed.
Results
Initial analysis showed a 38% DMR completion rate pre-implementation. Post-intervention, completion rates rose to 90%. The 'Continue all Remaining Home Medications' feature saw near-universal adoption among orthopaedic residents.
Conclusion
The initiative boosted the timely completion rates of DMR, achieving project-specific and institutional objectives. Key factors contributing to this success included active stakeholder engagement, representation from CTUs, timely analysis of performance data, and thorough root cause analysis. Resident involvement was pivotal in identifying and implementing workflow improvements. The audit and feedback system fostered a competitive environment, driving enhancements. Overall, this project improved DMR timeliness, enhancing the safety of patient transitions from hospital to outpatient care.
1. INTRODUCTION
Medication errors represent the most common type of medical error and represent a significant source of morbidity and mortality for hospitalized patients [1-4]. Up to 60% of medication errors occur during transitions of care, and up to 32.7% of hospitalized patients from the hospital will have one or more medication discrepancies at the time of discharge.
Medication Reconciliation is a process by which the medications of a patient are evaluated by the care team to facilitate transitions of care. At the time of admission, a Best Possible Medication History (BPMH) is completed to ensure that provider teams have access to the home medication list. These are then evaluated as part of the Admission Medication Reconciliation (AMR), and medications are either continued, held, or discontinued at the providers’ discretion. Finally, at the time of discharge from the hospital, the hospital medications of a patient are evaluated and either continued, prescribed, or stopped at the provider’s discretion in the Discharge Medication Reconciliation (DMR) [5, 6].
Clear, accurate, and timely completion of DMR is essential in reducing medication errors, ensuring patients know what medications they should be taking upon discharge, and communicating in-hospital medication changes to the patient’s community-based providers [2, 5, 7]. DMR has been identified by numerous organizations, including Health Quality Ontario (our institution's regional quality partner), as a key quality indicator.
At the London Health Sciences Centre (LHSC), the target for DMR completion is 85%. At project initiation, the Department of Surgery was the lowest-performing department, and the Division of Orthopaedic Surgery was the worst-performing surgical division, with a DMR completion rate of 42%. Hence, the purpose of this quality improvement initiative was to improve completion rates of DMR within our high-volume Orthopaedic Surgery division, with a specific goal of achieving at least 85% DMR completion by June 2023.
2. METHODS
2.1. Defining the Problem
Process mapping and a review of baseline data demonstrated failure points within the medication reconciliation process (Fig. 1). An Ishikawa diagram (Fig. 2), as well as a driver diagram (Fig. 3), were created to identify the root causes of incomplete DMR. Further, an analysis of the driver diagram was performed to identify potential change ideas.
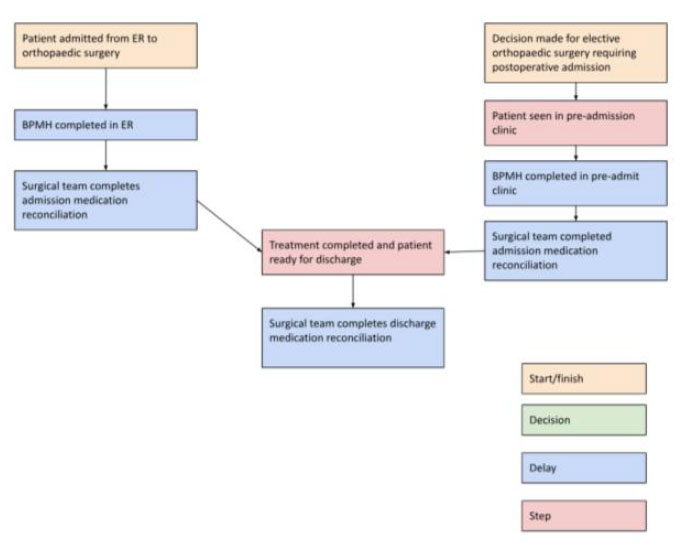
Process mapping areas of possible delay in the completion of discharge medication reconciliations.
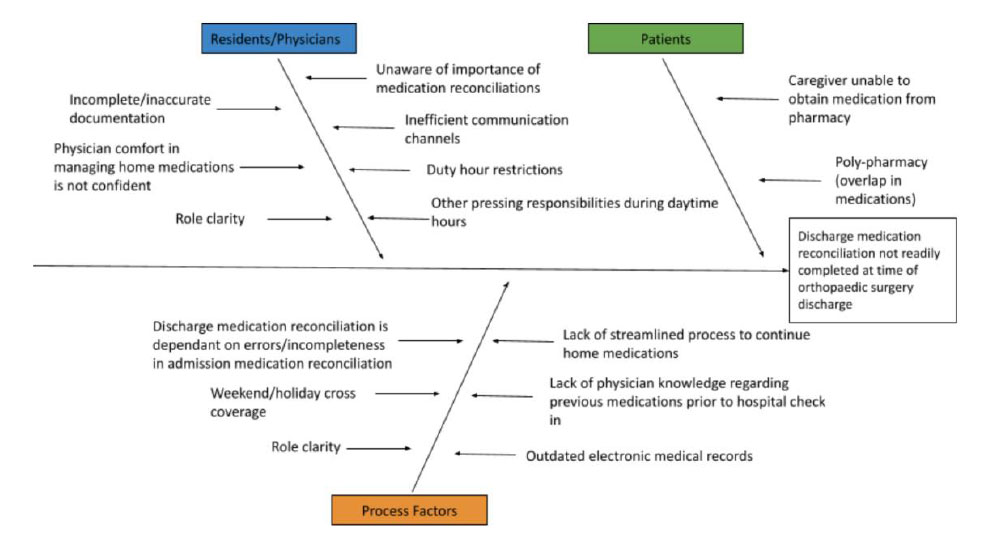
Ishikawa diagram revealing specific areas of delay.
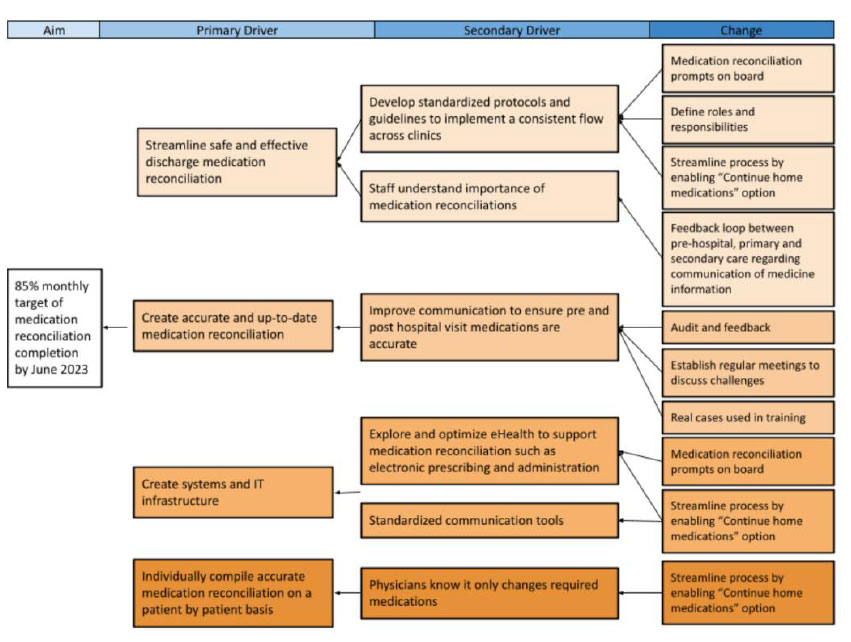
Driver diagram identifying causes of delay and corresponding change ideas.
2.2. Stakeholder Engagement
Early in the improvement process, critical stakeholders were identified and actively engaged. An Orthopaedic Surgery Quality Committee was established to address various projects, involving representatives from every Clinical Teaching Unit (CTU), a resident, a National Surgical Quality Improvement Program (NSQIP) case reviewer, and two quality facilitators. Additionally, nurse practitioners from CTUs identified as underperforming within the division were integrated into the committee. Executive sponsors at divisional, departmental, and institutional levels provided robust support for the Quality Improvement initiative.
2.3. Interventions
This project was guided by the “Model for Improvement” of the Institute for Healthcare Improvement. Plan-Do-Study-Act (PDSA) cycles were performed and evaluated in an iterative fashion.
The first intervention, initiated in October 2022, consisted of education and engagement of team members. As part of our divisional ‘Continuous Quality Improvement’ Rounds, attending surgeons, trainees, and allied health professionals in the Orthopaedic Surgery team were educated on the importance of DMR, institutional and provincial targets for DMR, and the potential implications of incomplete DMR.
Our second intervention, implemented in December 2022, focused on the timely completion of BPMH. Through our stakeholder engagement and discussion arising from these education sessions, a couple of barriers to DMR were identified. Specifically, one of the challenges with completing DMR in our orthopaedic surgical patients is the short turnover (27% of admissions were discharged within 24 hours). DMR is dependent on the timely completion of BPMH, and the institutional target of BPMH within 24 hours did not facilitate the timely completion of BPMH. As a result, we engaged our pharmacy team to facilitate the completion of BPMH as part of the pre-admission clinic process to ensure that the necessary information was available at the time of discharge.
Our third intervention, implemented in December 2022, focused on developing an efficient workflow for DMR. Another theme arising from stakeholder engagement and our education sessions was that evaluating the home medications of many of the patients was outside the practice scope of orthopaedic surgeons.
More importantly, patients on the orthopaedic floor were admitted for post-operative rehabilitation, which did not necessitate changes to their home medications. As a result, we worked with our medical informatics team to develop a ‘Continue all Home Medications’ button. This would allow a single click to indicate that no changes were necessary to the pre-admission home medications, even if they were changed as part of the admission.
In January 2023, a fourth intervention was introduced: an audit and feedback system aimed at encouraging friendly competition to boost DMR completion rates. The Orthopaedic Surgery Division was split into six Clinical Teaching Units (CTUs), with 3-7 faculty members participating in each. Monthly performance data was gathered, analyzed, and shared across the division, highlighting both top and underperforming CTUs.
2.4. Process and Evaluation
Outcome, process, and balancing measures were developed. Our primary outcome measure consisted of the rate of completion of DMR at the time of discharge. Process measures included the proportion of BPMH completed within 24 hours of admission for trauma/emergency patients and the proportion of BPMH completed at the time of admission for elective patients. Balancing measures included any reports of medication errors. We also collected qualitative data through discussion with team members to assess the flow and efficiency of this process. Data were tracked and evaluated monthly on statistical process control charts, which were shared with team members, division members, and other institutional stakeholders via our audit and feedback mechanism.
3. RESULTS
The timely completion rates of DMR increased dramatically over the duration of this quality improvement initiative (Fig. 4). Statistical process control charting suggested a significant increase in the timely completion of DMR after implementation of the first intervention in October 2022 until June 2023. At project initiation, DMR rates were 38%, reaching a nadir of 28% in August 2022. Over the final three months of the study, DMR rates were at 83%, reaching a peak of 90% in May 2023.
4. DISCUSSION
Errors and delays in DMR represent the most common patient safety error, causing healthcare staff to be unaware of how to conceive an accurate post-discharge medication plan. Medication errors are the most common type of hospital-based patient safety errors, with DMR representing a key transition point in patient care where medication errors are more likely to occur [7, 8]. Failures associated with DMR include failure to prescribe clinically important medications in the hospital that must be used post-discharge, incorrect dosage, poor communication during transition points of care, failure to specify which medications should be stopped or resumed post-discharge, inadequate reconciliation in handoffs during transfer, discharge, and admission of patients, and duplicate therapy at discharge as a result of hospital formulary substitutions or generic/brand name combinations [7, 9, 10]. The impact of risks, such as these, may also be intensified for families who are unable to access timely healthcare providers post-discharge [11, 12].
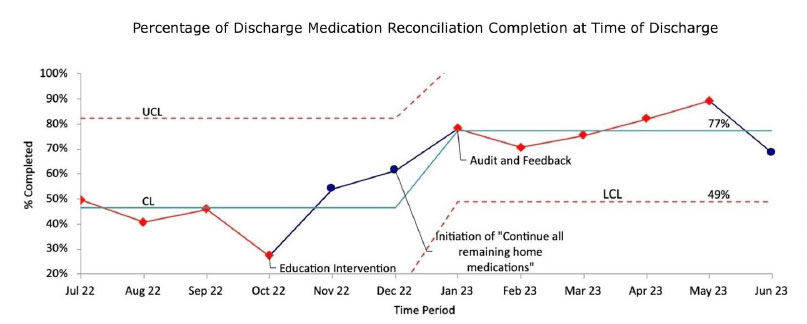
The statistical process control chart shows the percentage of discharge medication reconciliation completion at the time of discharge. Note: CL, center line; LCL, lower control line; UCL, upper control line.
Through the course of this quality improvement initiative, four interventions were implemented on the basis of our diagnostic tools. These combined to a dramatic increase in our DMR rates, from 38% at study initiation to 90% in May 2023. Additionally, orthopaedic surgery was the poorest-performing surgical division at project initiation, and by project completion, it was the top-performing surgical division. This also elevated completion rates for the entire department of surgery from 60% to 80%, with the vast majority of the improvement attributable to the orthopaedic surgery division.
There were several critical features of this project that we believe contributed to the overall success of this initiative. Firstly, broad stakeholder engagement and buy-in helped ensure our division was working collaboratively towards this common goal. One of the themes that emerged through our stakeholder engagement was improving the workflow. This stakeholder engagement allowed us to identify the ‘pain points’ for the orthopaedic residents who were responsible for the vast majority of the DMRs. This allowed us to develop EMR functionality to ensure the timely completion of BPMH and facilitate the safe and efficient completion of DMRs for patients without medication changes. Not only did this lead to a more efficient workflow, but our team feels that this allowed the front-line team members to feel that their concerns were heard and addressed, leading to increased engagement and buy-in.
Second, having access to timely and accurate data was instrumental in the success of this project. This facilitated our monthly audit and feedback and also allowed for rapid implementation of several interventions.
Third, the audit and feedback system significantly contributed to improvements. It ensured that attending physicians, medical trainees, and nurse practitioners across the division closely monitored this vital metric. By leveraging the inherent competitiveness of orthopaedic surgeons, it encouraged collegial rivalry and motivated underperforming CTUs to improve their performance each month. Impressively, in five of the nine months, the CTU with the lowest performance in one month ascended to the highest performance the following month, likely driven by the effectiveness of this system.
When rolling out the audit and feedback system, it was decided to present results at the CTU level instead of singling out individual providers. This strategy prevented any attending surgeons or trainees from feeling isolated based on their performance. However, individual performance data were accessible to providers upon request.
Segmenting the results at the CTU level rather than focusing on individual providers also facilitated collaboration with physician extenders from the identified CTUs. Upon identifying two CTUs with consistently lower completion rates, the project engaged three nurse practitioners supporting these units. Their feedback led to minor workflow adjustments, enabling them to participate more effectively in the DMR completion process.
Other methods of action have been tried to combat delays in DMR, such as utilizing a pharmacist-facilitated workflow. Seraphin et al. [13] piloted a pharmacist-facilitated workflow to decrease the number of errors that occur in DMR. This method involved the clinical pharmacist reconciling and reviewing inpatient and outpatient medications prior to discharge, consulting with the physician, and storing the DMR in an EMR so that the discharging hospital can review it. They found 19 discrepancies in the pre-pilot group, while only 6 in the post-pilot, with an overall success. This method to combat delays in DMR relies on strong communication with the pharmacist. Similarly, the American Society of Health-System Pharmacists suggests that the most effective strategy to combat delays in DMR is to allow pharmacists to take leadership of them, as they have distinct education and understanding that qualify them to take on efforts to maintain a medication reconciliation process that is productive in conjunction with hospitals [14].
The World Health Organization reports a series of steps to lead surgical departments to the success of timely DMR. These steps include education and training, implementing goals and a timeline, securing senior leadership, forming a team, developing a work plan, process mapping, defining problems, collecting current data, starting with small changes, and spreading information [15]. This project leveraged these principles to address the unique challenges in the completion of DMR within our division and ensure that improvement was achieved.
4.1. Limitations and Challenges
There were several limitations noted as part of this study. First, while our data allowed us to easily track the completion of DMR, there was no mechanism by which we could ensure the accuracy or appropriateness of the DMR. Over the course of the study period, there were no known reports or feedback about inaccuracy by either community care providers or pharmacists, but this is an important area that we were unable to assess.
Additionally, due to personnel changes in the Surgical and Quality and Performance Departments of our institution, we were unable to continue data analysis beyond June 2023. While we achieved excellent improvement over the study period, we were unable to assess the sustainability of this improvement.
Finally, these improvements are specific to the local context. These were implemented in a single, large orthopaedic surgical division of an academic teaching hospital, and strategies that led to improvement within our institution are not necessarily generalizable. While some of the themes of this project, including the importance of stakeholder engagement, addressing ‘pain points’, and the value of audit and feedback, are highly relevant to similar initiatives at other institutions, specific interventions must be tailored to and tested within the local environment and context.
CONCLUSION
In conclusion, a dedicated quality improvement project can successfully improve completion rates of discharge medication reconciliation in a high-volume, tertiary-care orthopaedic surgery division. In our study, critical drivers of success included broad stakeholder engagement and buy-in, simplification of workflow, and an audit and feedback system to deliver timely results and foster collegial internal competition. Thus, these strategies can be utilized to achieve success in similar quality improvement initiatives in different clinical settings.
AUTHORS’ CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| DMR | = Discharge Medication Reconciliation |
| BPMH | = Best Possible Medication History |
| AMR | = Admission Medication Reconciliation |
| LHSC | = London Health Sciences Centre |
| CTU | = Clinical Teaching Unit |
| NSQIP | = National Surgical Quality Improvement Program |
| PDSA | = Plan-Do-Study-Act |
ETHICAL STATEMENT
Ethics exemption was received by the Research Ethics Board at Western University (London, Canada).
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
ACKNOWLEDGEMENTS
The authors would like to acknowledge Dr. Julie Strychowsky and Dr. Louise Moist for guiding these improvement efforts and the quality and performance team at London Health Sciences Centre for providing timely and accurate data. Most importantly, Western University’s Orthopaedic Surgery Residents were instrumental in the success of this project, and their engagement and dedication to patient care was the driving force in the success of this initiative.


