CASE REPORT
Circular External Fixation for Distal Femoral Physeal Injury: A Case Report
Takahiro Sato1, *, Shuichi Chida2, Koji Nozaka1, Moto Kobayashi2, Tsutomu Sakuraba2, Ken Sasaki2, Naohisa Miyakoshi1
Article Information
Identifiers and Pagination:
Year: 2022Volume: 16
E-location ID: e187432502208220
Publisher ID: e187432502208220
DOI: 10.2174/18743250-v16-e2208220
Article History:
Received Date: 2/2/2022Revision Received Date: 31/5/2022
Acceptance Date: 15/7/2022
Electronic publication date: 10/10/2022
Collection year: 2022

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background:
Distal femoral physeal injuries are a challenging clinical scenario because the injuries have a high risk of growth disturbance. The selected treatments include closed reduction and cast immobilization, percutaneous pin fixation, and cannulated screws or internal fixation, but these treatments have some complications. Circular external fixation enables rigid immobilization and walking with full weight bearing. To the best of our knowledge, there is no article on the results of using circular external fixation for distal femoral physeal injury. This case is the first in which circular external fixation for distal femoral physeal injury is used.
Case Presentation:
A 9-year-old boy was injured in a skiing accident, and his injury was a Salter-Harris type II fracture of the distal femoral epiphysis. We immediately performed percutaneous pin fixation with circular external fixation under general anesthesia. After surgery, he was allowed to walk with full weight bearing. One year after surgery, he had no pain, and his knee regained full extension and 140°flexion.
Conclusion:
We consider circular external fixation to be an effective treatment option because of its rigid immobilization without injury to the plate. However, we and patients must fully acknowledge its difficulties (i.e., pin-site problems, neurologic injury, vascular injury, joint stiffness, and pain, and difficulty sleeping).
1. BACKGROUND
Distal femoral physeal injuries account for 1% to 6% of all physeal injuries and for less than 1% of all fractures in all children [1, 2], However, it is reported that these injuries have a high incidence of physeal arrest, ranging from 27.3% to 90% [3]. The selected treatment is closed reduction and cast immobilization, percutaneous pin fixation, cannulated screws, or internal fixation. Closed reduction and cast immobilization have a high risk of redisplacement [4], so we usually select percutaneous pin fixation cannulated screws for cast immobilization. However, percutaneous pin fixation requires pins across the physis and inappropriate invasion of the physis may cause growth arrest. Internal fixation requires reoperation for implant removal.
We used circular external fixation, which enables rigid immobilization and walking with full weight bearing without pins injuring the physis.
2. CASE PRESENTATION
Our case was a 9-year-old boy who had a skiing accident. He complained of severe pain in his left knee and swelling. After evaluating the radiograph, we diagnosed a Salter-Harris type-II fracture of the distal femoral epiphysis (Fig. 1). The Computer Tomography scan showed displacement of the epiphysis into the valgus, angulation, and flexion. Under general anesthesia, we performed percutaneous pin fixation with circular external fixation. First, we inserted two straight wires into each distal femur and proximal tibia. We attached full rings and performed closed reduction with distraction. After closed reduction, we inserted 2 Kirschner wires crossing from medial and lateral distal femoral metaphyses without crossing the physis. Permanent fixation was performed using 2 full rings for distal femur and a full ring for proximal tibia (Fig. 2). Immediately after surgery, he was allowed to walk with full weight bearing. Six weeks after surgery, we removed the external fixation under the nerve block, confirmed radiographic bone union, and started a knee range-of-motion exercise in addition to full weight bearing.
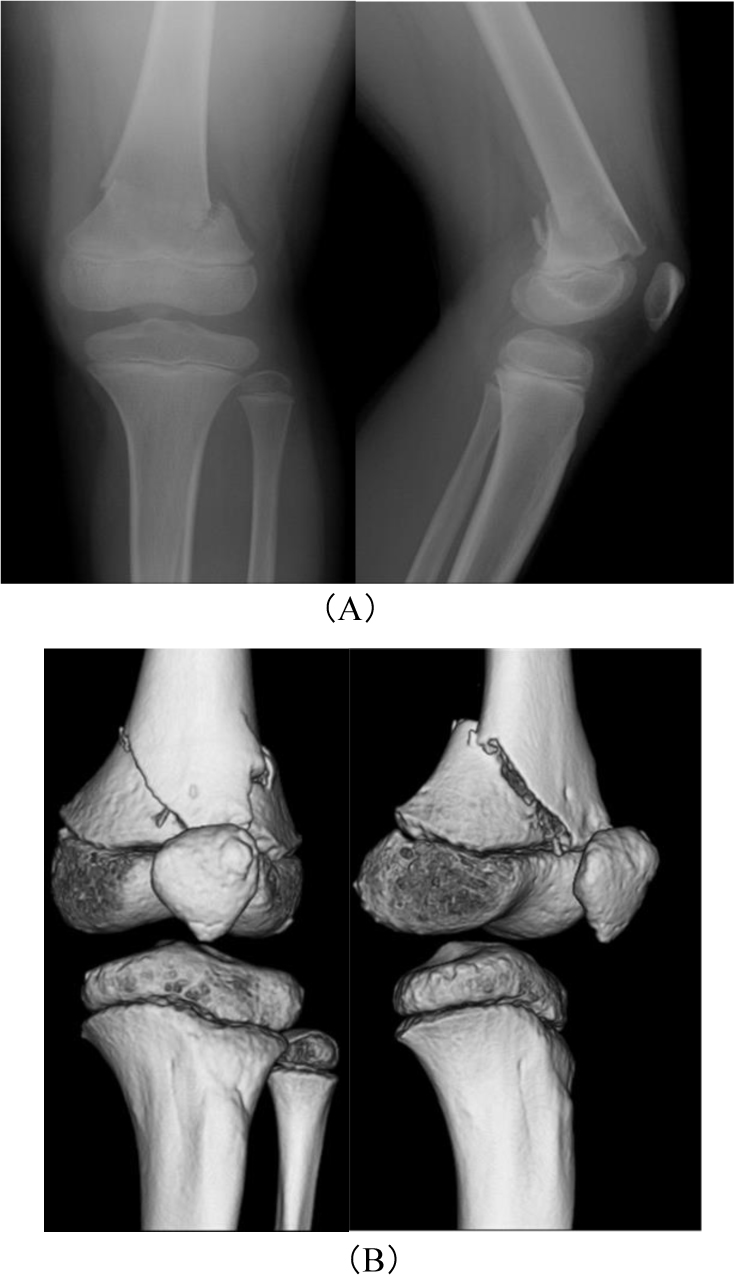 |
Fig. (1). Anteroposterior and lateral radiographs (A) of the left knee: Salter-Harris type II fracture and anteroposterior and lateral angle 3DCT (computed tomography) (B). |
 |
Fig. (2). Immediate postoperative anteroposterior and lateral radiograph. For reduction of flexion replacement, we used the arched wire technique to pin a proximal ring. |
One year after surgery, he had no pain, and his knee regained full extension and 140° flexion (Fig. 3).
 |
Fig. (3). Postoperative 1-year anteroposterior and lateral radiographs. |
3. DISCUSSION
Distal femoral physeal injuries are a challenging clinical scenario because the injuries have a high risk of growth disturbance [1]. The distal femoral physis is the fastest growing growth plate in the human body, growing at a rate of 1.0 cm per year and contributing to 70% of the longitudinal growth of the femur and 40% of the overall growth of the lower extremity [5, 6], Physeal closure and cessation of growth typically occur between 14 and 16 years of age in girls and between 16 and 18 years of age in boys. Distal femoral epiphyseal fractures are relatively rare but have a high incidence rate of complications (i.e., leg-length discrepancy, permanent decreased range of motion, and angular deformity) and are responsible for 1-6% of all physeal injuries and less than 1% of fractures in children [1].
First we tried closed reduction and cast immobilization, however conservative treatments without fixation are associated with loss of reduction. Therefore, surgical treatments are frequently needed for more rigid stabilization than cast immobilization without fixation. Surgical treatments are suggested, pin fixation, cannulated screws with cast immobilization, and open reduction and internal fixation. In the English and Japanese literature, there have been 14 studies (or case reports) describing surgical treatments and complications. (Table 1) [4, 7-18] Most authors agree that closed reduction using percutaneous pins or screws in Salter-Harris type I and II fractures is the treatment of choice. However, percutaneous pin fixation sometimes needs pins across the physis. A recent study by Arkader et al. suggested that pins across the physis may be a cause of growth arrest [4]. Moreover, Edmunds and Nade reported that they had 60% poor results with closed reduction and percutaneous pinning in contrast to 16.6% poor results with open reduction and internal fixation in Salter-Harris type II [19]. Open reduction and internal fixation require reoperation for implant removal under general anasthesia, although it provides rigid immobilization.
| S.No | Source | Solter-Harris classification | Treatment | Complication |
|---|---|---|---|---|
| 1 | Ali Aydin et al. (2012) | Type III, IV 1 patent |
Cannulated screw | none |
| 2 | Mukohara et al. (2017) | Type II 1 patient |
Locking plate | none |
| 3 | B.R. Garrett et al. (2011) | TypeI~IV 55 patients |
Pin fixation or Cannulated screw with cast immobilization | Physeal bars Leg-length discrepancy and deformity |
| 4 | Elzbieta Kuluta-Bosak et al (2010) | TypeII 1 patient |
Pin fixation and 2 AO screw | none |
| 5 | Eric J. Wall et al. (2012) | TypeII, III 2 patients |
Pin fixation Cannulated compression screw |
A partial physeal bar |
| 6 | Arkader, Alexandre et al. (2007) | TypeI~IV 73 patients |
Pin fixation, Cannulated screw, open reduction, external fixation | Growth arrest Loss of reduction Superficial pin infection |
| 7 | Ilharreborde B. et al. (2006) | TypeII 20 patients |
Cortical screws Osteosynthesis |
LLD, Angular deformity, limitation in ROM, epiphysiodesis, ligamentous laxity |
| 8 | Plánka L. et al. (2008) | TypeI~IV 46 patients |
K wires or 1-2 cannulated tension screws |
Angulation, shortening, development of porosis, limitation in hip and knee ROM, redislocation, resurgery, damage to neurovascular plexus, complete healing of epiphysiolysis |
| 9 | Eid A. et al. (2002) | TypeI~IV 151 patients |
K wires or cancellous screw | Lower limb deformity, range of movements in the knee, ligamentous laxity thigh atrophy, limb length discrepancy, angular deformity, premature growth arrest |
| 10 | Buess-Watson E. et al. (1994) | TypeI~IV 43 patients |
Internal fixation, percutaneous pinning | Asymmetric growth arrest/axis deviation, LLD, (re)operation, stability |
| 11 | Caterini R. et al. (1991) | TypeI~IV 16 patients |
K-wire | Symptoms, physical examination findings, XR examination of complications |
| 12 | Lippert W. et al. (2010) | Type III 14 patients |
Percutaneous pinning ORIF |
LLD/growth disturbance, ROM deficit, pain, physical limitations |
| 13 | Edmunds I. et al. (1993) | TypeI~IV 33 patients |
Percutaneous fixation with wires or screws Internal fixation with K wires, AO screws, Herbert screws | LLD, angular deformity, limitation in ROM, osteomyelitis, lost position, further treatment required |
| 14 | Thomson J. et al (1995) | TypeI~IV 30 patients |
Internal fixation with screw or pin | LLD, malalignment, loss of ROM, loss of reduction, further bony surgery |
| 15 | Our case | TypeII 1 patient |
Circular external fixation | Pin-tract infection pain |
Circular external fixation enables closed reduction by using ligamentotaxis even in large displacement fractures, so it does not necessarily need pins across the physis for reduction and immobilization in surgery. Furthermore, gentle closed reduction and fixation are important for bone union in terms of biological characteristics and vascularization of the fracture area [20]. Circular external fixation may be noninvasive skin, soft tissue, and even physis. In addition circular external fixation consists of wires, which can be easily removed using a nerve block.
Our treatment has some problems. First, children may find the use of a circular external fixator uncomfortable and painful, to the point of not being able to stand it. In our case, the pain made it difficult for him to walk by himself immediately after surgery. The pain gradually improved, and he was able to walk in rehabilitation. The second problem is pin-tract infection. Meticulous pain care and immediate treatment with antibiotics are necessary at any sign of infection. In our case, he had a mild pin tract infection, which we could treat with only oral antibiotics. Paley reported the Ilizarov method for children who have many difficulties (i.e., pin-site problems, neurologic injury, vascular injury, joint stiffness, and pain, and difficulty sleeping) [21]. Therefore, we must inform patients and their parents of these difficulties when we use circular external fixation.
CONCLUSION
To the best of our knowledge, there is no article on circular external fixation for distal femoral physeal injury. In our case, we obtained good results using circular external fixation; however, we found other difficulties at the same time.
Final thoughts, we consider circular external fixation to be one of the effective treatment options, although we and patients must fully understand its difficulties.
AUTHORS’ CONTRIBUTIONS
SC and TS performed the surgery. TS, MT, KS prepared the manuscript. KN and NM assisted in drafting and review of the manuscript. All authors read and approved the final manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient's legal guardian for publication of this case report and any accompanying images because the patient was under 18 years old.
STANDARDS OF REPORTING
CARE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of this study are available within this article.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
We thank Springer Nature Author Services (https://authorservices.springernature.com/) for editing a draft of this manuscript.








