All published articles of this journal are available on ScienceDirect.
Dynamic Postural Stability after Cartilage Repair in the Knee
Abstract
Background:
Articular cartilage has an exceptionally poor capacity for healing, but Autologous Matrix Induced Chondrogenesis is a procedure with a substantial body of literature that demonstrates its performance in chondral and osteochondral repair. However, data concerning dynamic postural stability after cartilage repair procedures is lacking.
Objective:
Therefore, the present study was designed to assess postural stability following cartilage repair in the knee.
Methods:
20 adults had undergone Autologous Matrix Induced Chondrogenesis for the treatment of full-thickness cartilage defects, with minimum 36 months of follow-up. Clinical outcomes were evaluated by patient reported outcome measures while dynamic postural stability was assessed using the star excursion balance test. The untreated, contralateral limbs served as controls.
Results:
At a mean follow-up of 43 months, patients reported a Visual Analog Score for pain of 1.6±2.2, a mean Lysholm score of 78.5±17.9 and a mean Knee Osteoarthritis Outcome Score of 143.3±16.1. The star excursion balance test showed no significant difference between limbs.
Conclusion:
With no difference in dynamic postural stability, our results indicate that this treatment provides a positive clinical outcome, with no deficits in postural stability when compared to the contralateral, untreated leg.
1. INTRODUCTION
It is no surprise to state that neuromuscular control is essential to maintaining balance as well as producing desired movements. The neuromuscular system is comprised of a variety of sensorimotor units and the central integration and processing of various components provide for overall functional joint stability and control of movements [1]. Stability and balance are based on inputs from a host of afferents that provide input to the central nervous system, which then affects muscle control to maintain postural stability [2]. This is all done unconsciously, yet if there is a deficit in proprioceptive input, the neuromuscular pathways can be impacted, potentially leading to the development of risk factors that may contribute to injury [3].
Among the tissues in the knee joint, mechanoreceptors have been previously documented in detail [4, 5], with peripheral receptors (mechanoreceptors) being found within joints, ligaments, tendons, muscles, and skin [6]. It has been stated that this afferent system controls motion with a high degree of regulation against internal and external disturbances and maintains joint stability [7]. However, there is little understanding of the role, if any, that articular cartilage may play in proprioception. There has been some indication that chondrocytes may contain mechanoreceptors [8], while an earlier article had proposed a chondrocyte mechanoreceptor model [9]. More recently, Donnell et al. (2019) stated that subchondral bone may provide ingrowth of sensory nerves into the articular cartilage [10].
However, there has been little research into articular cartilage's role in neuromuscular control and joint stability. Dynamic postural stability (DPS) has already been documented to be affected by a variety of lower extremity injuries [11-14]. However, very little data has been presented, which has assessed DPS regarding chondral lesions. Unfortunately, articular cartilage has a very limited capacity for intrinsic repair [15]. Full-thickness cartilage lesions may be associated with significant pain and impaired function, and if left untreated, these defects will fill with biomechanically incompetent fibrous tissue, eventually leading to premature osteoarthritis [16]. While it is generally recognized that symptomatic articular cartilage defects ought to be restored, these lesions remain a difficult medical problem to treat [17]. As a result, cartilage defects, with their associated degenerative changes, maybe a major source of disability and present a significant socioeconomic burden [18].
A recent paper investigated the proprioceptive function of patients with isolated articular cartilage lesions of the knee [19]. The authors reported that patients with isolated articular cartilage lesions of the knee demonstrated a significant proprioceptive deficit as compared to a control cohort with normal knees. These authors further hypothesized that a proprioceptive deficit may lead to altered gait, with the resultant unphysiological joint loading, thereby leading to degenerative changes within the joint [19]. As a treatment for chondral lesions, a variety of surgical techniques have been developed that aim to restore the articular surface and tissue specific integrity, thereby restoring joint function and preventing progressive joint degeneration [17, 20]. Among these techniques, our clinic uses a one-stage procedure in which a bone marrow stimulation procedure is enhanced by covering the treated site with porcine-derived collagen I/III membrane. This procedure, known as autologous matrix induced chondrogenesis (AMIC), has already been shown to result in positive outcomes [21-23].
While the patient reported outcomes measures (PROM) have been encouraging, it would add to our knowledge base if there was an objective assessment of biomechanics following treatment. To this end, we sought to evaluate the proprioceptive function of patients who had undergone AMIC by assessing their dynamic postural stability (DPS) using the untreated knee as a control.
2. METHODS
2.1. Patients
Adult patients who had undergone surgery for full thickness chondral or osteochondral lesions in the knee (Outerbridge Classifcation III or IV) were included in this study. The index procedure was performed by 1 of 3 trained orthopaedic surgeons, using a mini-open approach [24]. After debridement, a 1.2-mm drill was used to perforate the subchondral bone plate to a depth of 1 cm, thereby mobilizing bone marrow stem cells into the defect. Care was taken to leave areas of the intact subchondral bone plate between the drill holes. A bilayer type I/III collagen membrane (Chondro-Gide®, Geistlich Pharma AG, Wolhusen, Switzerland) was then placed over the treated area and a fibrin sealant was then applied.
Patients with a minimum follow-up of 36 months were included in this study. Having concomitant surgeries and poor compliance at the time of AMIC. Relevant comorbidities and current injuries were exclusion criteria. Individuals with bilateral cartilage defects or limb pain that would affect their gait were also excluded.
2.2. Clinical Outcomes
In order to gain a subjective assessment of the clinical outcomes, we used 2 instruments to gather the PROMs. While the visual analogue scale (VAS) for pain is well established and used in many fields, we additionally used an instrument specific to the knee. The Lysholm scale has been validated as an acceptable tool for outcomes assessment of various chondral disorders [25].
2.3. Star Excursion Balance Test
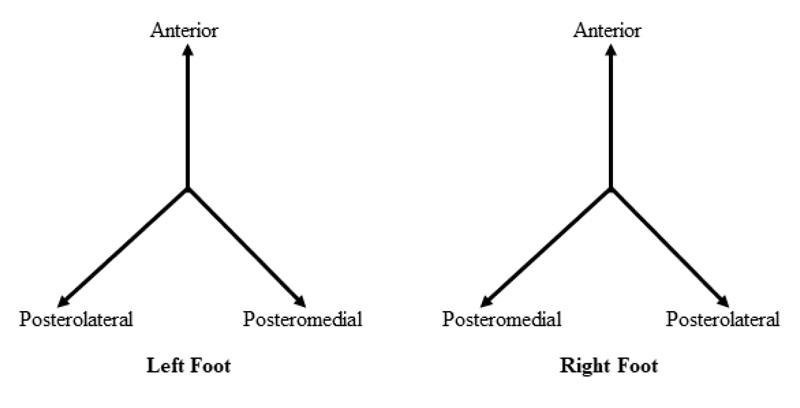
The star excursion balance test (SEBT) is a simple yet reliable tool to detect dynamic balance deficits [26]. The participants were requested to perform a series of single limb squats during which the non-stance limb touches the farthest points point along the directional axes (anterior, posterolateral, posteromedial) marked on the floor [13]. A schematic of the test is depicted in Fig. (1). The sum of the maximum of each reaching distance normalized to leg length equals the composite reach distance [14]. Additionally, the maximum anterior reaching distance was measured and compared with the non-operated limb, as previous research has indicated this may be predictive of a lower extremity injury [14].
Means and standard deviations were calculated for the baseline characteristics, SEBT reaches distance and limb length. As reach distance has been associated with limb length, reach distance was normalized to limb length to allow a more precise comparison between patients. In order to express reach distance as a percentage of limb length, the normalized value was calculated as reach distance divided by limb length and then multiplied by 100. Composite reach distance was the sum of the 3 reach directions divided by 3 times limb length, then multiplied by 100 [14].
2.4. Statistical Analysis
Statistical analysis was conducted with Graph Pad Prism 7 (Graph Pad Software, San Diego, USA). With regard to the SEBT, a t-test was used for the comparison of index limbs to control. In order to evaluate any relationship between Lysholm scores and SEBT results, the Pearson product moment test was used for the correlation analysis. Level of significance was set at p <0.05.
3. RESULTS
3.1. Demographics
From our patient database, we randomly selected 50 patients who met the inclusion criteria. Of these, 22 patients gave informed consent to participate in this study but 2 patients were excluded due to bilateral knee pain, leaving 20 patients (9 female, 11 male). The mean age was 38 ± 15 years, while the mean BMI was 25.7 ± 4.2. The cartilage lesions (all grade III or IV) had a mean size of 2.6cm2 (range: 1-3.4). The mean post-surgical follow-up was 43 months (range: 36-47 months).
3.2. Clinical Outcome
We recorded 2 PROMs. The mean VAS at the time of follow up was 1.6 ± 2.2 (range: 0-7). Only 3 patients reported pain ≥5. The mean of the KOOS was 143.3 ± 16.1 (range: 116-166), while the mean Lysholm score was 78.5 ± 17.9 (range: 53-100). Only 3 patients, all female, presented a Lysholm score <65. The lowest Lysholm score among our patients (a Lysholm score of 26) was reported by a patient who was 70 years old at the time of surgery.
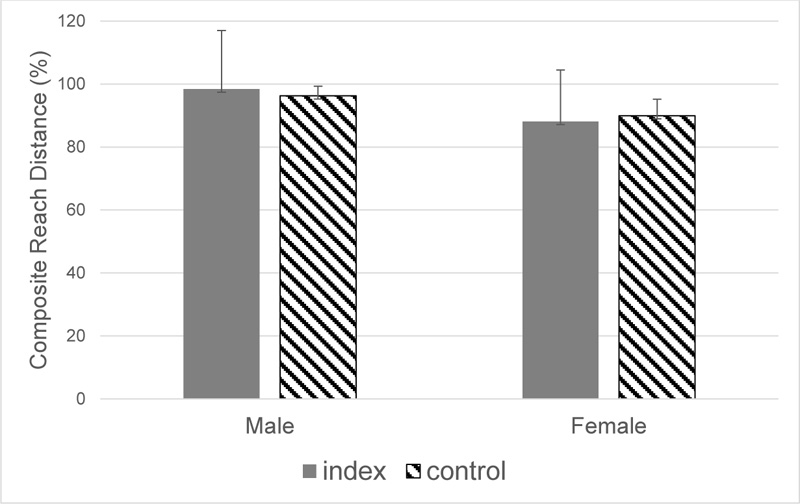
3.3. Star Excursion Balance Test
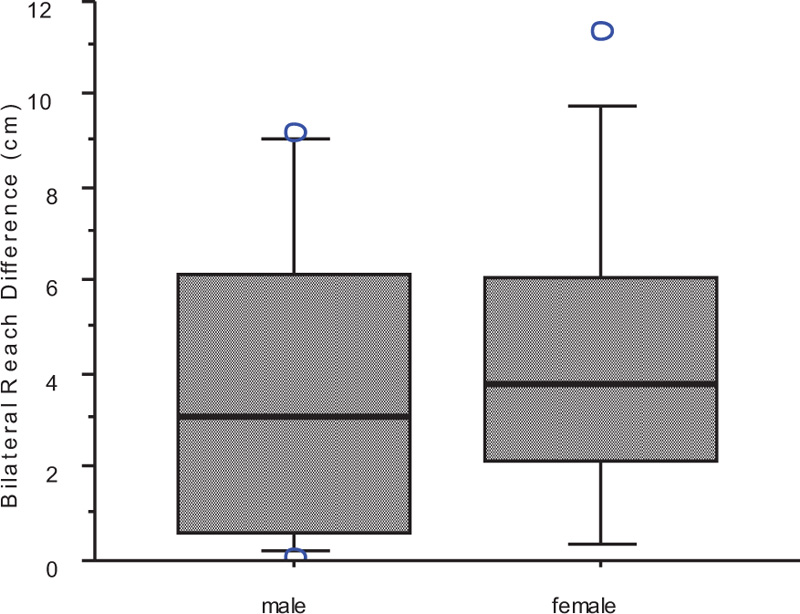
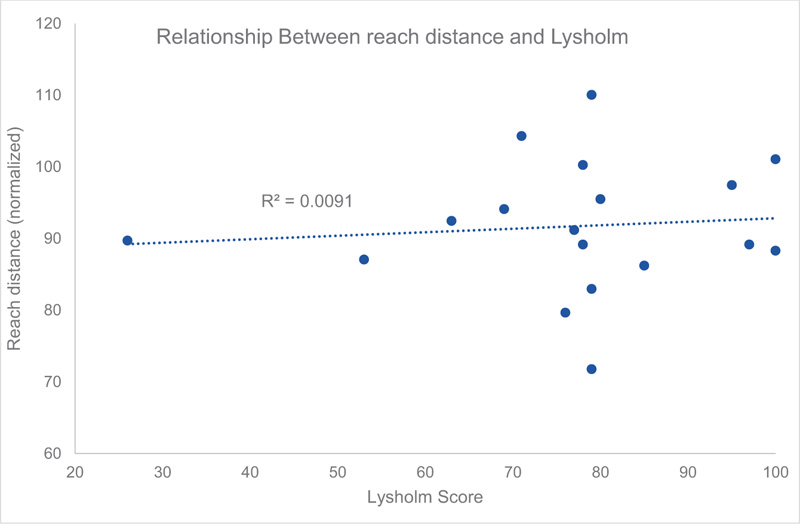
The mean of the normalized composite reach distance of the index limbs was 91.14 ± 8.88cm versus 92.82 ± 8.86cm for the control limbs. Statistical analysis of the SEBT revealed no significant differences in the normalized composite reach distance of index limbs compared to contralateral limbs (p = 0.479), which was also independent of gender overall (p= 0.543), as depicted in Fig. (2). The bilateral difference in the anterior reach distance exhibited a mean of 3.89 ± 3.3 cm, which was likewise independent of gender (Fig. 3). There was no relationship between Lysholm scores and the SEBT (p = 0.1, r2 = 0.009), as shown in Fig. (4).
4. DISCUSSION
To the best of our knowledge, this has been the first study reporting results regarding the bilateral difference in DPS following cartilage repair procedures in the knee. Our results indicate that DPS is bilaterally comparable following AMIC for the repair of chondral lesions. Until now, most studies reporting the outcome after cartilage repair have focused on functional outcome measures by established clinical outcome scores [27] and/or MRI scans [28]. The results of the functional outcome scores in our series have shown positive outcomes after the index procedure, which agrees with our previously reported results in midterm follow up [23]. The PROMs that we have reported are consistent with previously published data, in which a significant decrease in pain, as assessed by VAS, was noted in several studies following AMIC, with follow-up even in the longer term [23, 27]. With regard to PROMs, the Lysholm scale has been validated as a patient-administered instrument to measure the domains of symptoms and complaints in daily activities [29], and our results are in agreement with the literature, where the Lysholm improved significantly, relative to baseline, following AMIC procedure [30, 31]. In contrast to the Lysholm score, the KOOS score holds 42 items in five separately scored subscales [32]. The statistically and clinically significant improvement in KOOS that we noted is also in agreement with the results that were published in a recent meta-analysis [31].
While the results of all PROMs that we used are consistent with published literature concerning the repair of the chondral and osteochondral lesions in the knee, there is also a need to assess more objective measures with regard to the patient’s outcomes.
One aspect of motor function that may be important, especially as it relates to injury recurrence, is dynamic postural stability (DPS). The Star Excursion Balance Test (SEBT) was therefore selected to evaluate motor control strategies during a standardized motor task, as it functions as an index of DPS and has been frequently used to study motor control [26, 33] and shows excellent inter- and intra-rater reliability [34]. We noted no difference in SEBT measures when compared between operated and contralateral knees, which indicates that patients had achieved normal DPS. This may be relevant to the possibility of reinjury. Previous data have indicated that DPS may be predictive of ACL injuries [35], while other researchers have stated that a deficit in postural stability could be a risk factor in ankle sprains [36]. However, we cannot be sure whether the return to normal DPS is attributable to the surgical technique employed in these patients, their rehabilitation programme or even their baseline status.
The somatosensory system is essential to provide feedback for postural control and, subsequently, DPS [37]. As it pertains to cartilage lesions of the knee, it has been recently reported that articular cartilage lesions have a major influence on knee proprioception [19]. In that study, patients with confirmed articular cartilage lesions showed significantly worse scores in unilateral postural stabilometry than uninjured controls. As a notable point, the patients even exhibited a decreased proprioceptive control of the unaffected knee. This differs from our results but may be due to their patients being pre-operative, while ours were ≥3 years post-operative. As we did not have pre-operative DPS results, it would be purely speculative to state whether our patients regained DPS; however, this may be a clinically relevant topic for future study.
Among our patient cohort, we did not see a difference in the composite reach distance or the anterior reach distance when we compared the index versus the contralateral knees. It had been previously reported, among a prospective cohort, that patients who exhibited an anterior right/left reach distance difference greater than 4 cm were 2.5 times more likely to sustain a lower extremity injury, while those with a composite reach distance of less than 94.0% of their limb length were 6.5 times more likely to have a lower extremity injury [14]. As a cohort, the mean side-to-side difference was 3.8 cm, while some patients exceeded this threshold, as depicted in Fig. (3). Likewise, it was reported that a composite reach index of less than 94% leg length was associated with an elevated risk of re-injury [14], and while there were several of our patients who met this criterion, none had reported a re-injury at the time of follow-up.
The principal drawback to our research is that we did not have values for DPS prior to surgery. Another limitation to this study is the extent to which the findings can be generalized beyond the cases studied. The number here is too limited for broad generalization, however, this be seen as a fruitful avenue for future research under the same theme.
CONCLUSION
Our data represents, to the best of our knowledge, the first study reporting results of dynamic postural stability following cartilage repair in the knee. These results show that besides a positive clinical outcome, the AMIC technique enables normal dynamic postural stability when compared to the contralateral, unoperated limbs.
LIST OF ABBREVIATIONS
| DPS | = Dynamic Postural Stability |
| VAS | = Visual Analogue Scale |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the institutional ethical committee (AZ 15-349).
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the basis of this research. All the humans used were in accordance with the Helsinki Declaration of 1975.
CONSENT FOR PUBLICATION
Informed consent was obtained from all individuals and participation was voluntary.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the results and findings of this study are available within the article.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
We would like to thank Takanobu Oshima for his editorial assistance.


