All published articles of this journal are available on ScienceDirect.
Brace Prescription for Adult Scoliosis - Literature Review
Abstract
Purpose:
The 2021 SOSORT guidelines stipulated that braces be prescribed for adult scoliosis with chronic pain and progressive curve. Yet, there have been no objective protocols relating to the prescription of the brace. Therefore, this review investigates if there are any objective criteria or generally agreed on protocols for brace prescription in adult scoliosis patients.
Methods:
Relevant papers were searched in PUBMED. Only articles that are in English and cover the clinical aspect of adult scoliosis bracing are included.
Results:
A total of twelve papers were identified. They include different adult scoliosis braces, ranging from elastic belts to rigid braces. The treatment protocol varied tremendously. No objective criteria were found concerning the prescription of a brace, daily wearing time, duration of the intervention, and weaning protocol. The brace treatment was primarily employed to manage low back pain.
Conclusion:
Our search showed no objective criteria and clear indications for bracing and no consensus concerning the prescription of braces, daily wearing time, and duration of the intervention for patients with adult scoliosis.
The authors proposed prescription of a brace be based on more objective radiological criteria and severity of low back pain. Brace prescription should depend on the flexibility of the curve and can range from accommodative to rigid braces of corrective design. “Corrective” brace has to be worn at least 14 hours daily for six months or until the low back pain subsides to the extent that permits daily activities with minimal discomfort. “Accommodative” brace can be worn when required.
1. INTRODUCTION
Adult scoliosis includes adult idiopathic scoliosis (IS) and degenerative lumbar scoliosis (DLS). Idiopathic scoliosis has its onset in childhood and adolescence, while degenerative lumbar scoliosis starts later in life, generally over 50. Thus, the prevalence of adult scoliosis is significantly higher than that of idiopathic scoliosis, particularly with increasing age, as the incidence of DLS increases with age [1, 2]. The reported prevalence of adult scoliosis ranges from 8.85% to 68% [3-5]. Fortunately, over 80% of the DLS patients have a mild curve of 10-20o [2].
Patients generally seek treatment for pain and disabilities rather than deformities [6]. Back pain is generally more common and severe in the thoracolumbar, lumbar, and lumbosacral curves than in the thoracic curve [7]. The thoracolumbar curve is treated surgically as the most common curve [8].
For symptomatic scoliosis patients, many different types of treatment have been studied. Unfortunately, dry needling, manipulation, and chiropractic treatment provide only short-term pain relief [9]. The temporary improvement is understandable, as the treatments address the pain instead of the underlying deranged spinal biomechanics. Adult scoliosis brace, which attempts to stabilize or improve the altered spinal biomechanics, has a better outcome but minimal evidence [9]. A recent systematic literature review concluded that many bracing studies on adult scoliosis patients are biased [10].
However, recent studies have shown that bracing provides pain relief and stabilizes postures [11-13]. Also, the 2011 SOSORT guidelines stipulated that braces be prescribed for adult scoliosis patients with chronic pain and progressive scoliosis curves [14].
Given the inconclusive evidence, clinicians sometimes have difficulty determining if a brace is indicated in adult scoliosis patients presented with low back pain. We thus undertake to review the literature to determine if there are any objective criteria upon which we can base when prescribing an adult scoliosis brace. We also investigate whether there is a generally agreed protocol for brace wear in adult scoliosis patients.
2. MATERIALS AND METHODS
Relevant papers were searched in PUBMED, using the Boolean search operators: (“adult scoliosis” OR “adult spinal deformity”) AND (“orthotic” OR “brace”), and the keywords “adult scoliosis” AND “radiological parameters.” All titles were then screened for relevancy. Papers not in English and irrelevant to the present investigation were excluded. Only those papers, including brace as treatment and studying the radiological parameters of adult scoliosis, were reviewed. Also, a manual search was undertaken from the references of the selected papers.
3. RESULTS
The search yielded 17 papers, of which 12 were regarded as appropriate. In addition, a manual search of the articles revealed other articles on scoliosis curve progression.
A review of the bracing studies showed that most braces were prescribed for adult scoliosis patients with thoracolumbar, lumbar, and double curves. The Cobb angle ranged from 10o to 91o [11-13], with a visual analog scale (VAS) of low back pain of not less than 6/10 [11, 15, 16]. Only one study included patients with the thoracic curve [17]. Most of the subjects had chronic low back pain.
Different types of braces have been used for the treatment. They ranged from the modified off-the-shelf elastic belt [16], a specific scoliosis soft brace (Peak Scoliosis Brace) [17, 18], Spinecor [19], to rigid braces [11-13, 20, 21]. Of interest is that the rigid braces prescribed employed different biomechanical principles. The Physiologic© brace is a sagittal alignment brace used to restore sagittal alignment in adult scoliosis patients. The sBrace [15], Vesinet TLSO [13], the Lyon brace [12, 21], and the ART brace [12] attempted to correct or accommodate scoliosis in three dimensions. However, no standards have been found concerning the prescription of the braces. The Peak Scoliosis brace, which is an off-the-shelf brace, was prescribed for adult scoliosis patients, with a mean Cobb angle of 61.9o [17], while rigid braces were prescribed for curves, with Cobb angle measuring 36—50o [11-13, 21] (Table 1).
| Scoliosis | Paper | Study | Age | No/Sex | Complaints | Brace | Prescription | Outcome | Remarks | ||
| LBP: VAS | Curve | VAS | Cobb | ||||||||
| Adult AIS | Marcotte 2010 [19] | Prosp | 18-69 | 26F; 4M |
- | - | Spinecor | 10-130 hrs/wk; 18-28 mths |
Improved 77% | - | - |
| Weiss et al. 2016 [20] | Case Report |
37 | 1F | Average: 5-7/10 Occasional episodes: 8-9/10 |
Double curve; Th 56o; LB 50o | Gensingen | 3-4 hrs daily; 3 days/wk 16 mths |
0/10 | Th/L: 55/32 | Ex | |
| Polastri and Romano 2017 [16] | Case Report | 40 | 1F | 8.5/10 | ThL and LB curves: 22o | Customized elastic brace | At-will; 24 mths |
2/10 | - | - | |
| de Mauroy et al. 2016 [12] | Prosp | 56 ±17 | 144F; 14M | - | ThL and LB: 39.7±17.4o |
Plaster cast + Lyon brace |
3 wks plaster; 6 mths Lyon brace 4 hrs/day; ≥5 yrs |
24% improved > 5o; 56% stable; 20% worsened >5o |
Ex; Cobb angle: NS Coronal Bal: S Sagittal Bal: NS |
||
| Han et al., 2020 [23] | Prosp | 24.3 | 17F; 1M | - | 29.3 o | All Line | 12 hrs/day; 12 wks | - | 24.0o | Sig reduction in Cobb angle | |
| DLS | Weiss and Dallmayer 2006 [22] | Case Report | 47 | 1F | 8000 steps medicated | LB: 55o; LB kyphosis: 30o |
Physiologic Brace | Daily: at-will 10 days |
Reduce by 1/5; 12000 steps | - | - |
| Adult AIS and DLS |
Weiss et al 2006 [24] | Prosp | 41±21 | 29F | 3.38/5 | 37 ± 22o | Physiologic Brace | >8 hrs/day (at will); av 7.5 mths |
2.69/5 | - | Poor compliance |
| Weiss and Werkmann 2009 [11] | Prosp | NA | 58F; 9M | 3.3/5 | 41 ± 22o (10-91 o) | Physiologic Brace | 20hr/day x 6 mths; case by case; 18 mths | 2.0/5 | - | Changes in pain measures: Sig | |
| Gallo 2014 [15] | Case Reports | C1: 65 C2: NA |
2F | C1: 8-9/10; C2: 8/10 |
NA | sBrace | At-will | C1: 3-4/10; C2: 2/10 |
- | - | |
| de Mauroy et al 2016 [21] | Prosp | 57±16 | 650F; 89M |
- | 36.0 ± 17.4o | Plaster cast + Lyon brace |
3 wks plaster; 6 mths Lyon brace; 15 yrs |
- | - | Non-adherent: 17% |
|
| Palazzo et al 2017 [13] | Retrosp | 61±8 | 38F | - | 49.6±17.7o; Progression rate: 1.28/yr |
Vesinet TLSO | ≥ 6 hrs/day; 5 yrs |
Progression rate: 0.21/yr | - | - | |
| Zaina et al 2018 [17] | Prosp | 68±11 | 20F | 7.15/10 | Av Cobb: 61.9o 55% ThL/LB; 30% Double curve; 15% Th |
Peak Scoliosis Brace | 2-4 hrs/day; 4 wks |
5.85/10 | - | - | |
Also, the daily wear of the brace varied tremendously with the studies, ranging from at-will [15, 22] to 12 [23] to 20 hours/day [11], and 24 hours/day [12]. The variation may be related to the severity of the structural curves and the intensity of pain. De Mauroy et al. [21] reasoned that the extended period of daily wear was necessary to elongate the contracted tissues.
Further, the duration of the intervention is not uniform. Palazzo et al. [13] and de Mauroy et al. [21] did not describe the length of treatment; they followed up the patients for more than 5 and 15 years, respectively. Weiss and Werkmann [11] reported assessing the patient again 18 months after the initial brace wear.
There were no studies on in-brace correction in adult scoliosis. The outcome measured was on reduction of progression rate [12, 13] and pain intensity, which are the most common and easiest measures of brace success [11, 15, 17]. De Mauroy et al. [12] showed that the Lyon brace improved 24% of the curves by ≥5o, stabilized 56% of the curves, and worsened 20% by ≥5o in 158 patients with adult scoliosis. Similarly, Palazzo et al. [13] reported that brace treatment reduced the progression of adult scoliosis curves from 1.28o to 0.21o per year.
4. DISCUSSION
The studies have shown that rigid and soft braces reduce low back pain, and rigid brace contains curve progression in adult scoliosis patients. The indications are consistent with the SOSORT guidelines, which stipulated the brace prescription when back pain and curve progression are maximal in adult scoliosis patients [14]. A brace is indicated for patients whose low back pain did not respond to conventional treatments [11, 12, 21]. It is also used to stabilize adult scoliosis [12, 21] and reduce the curve progression rate [13]. In a retrospective cohort study that involved 38 female patients, a spinal brace reduces the curve progression rate from 1.28o to 0.21 o per year [13].
The daily brace wearing hours vary with studies, from “at-will” [15] to 24-hours [12, 21]. In addition, the wear duration ranges from 7.5 months [24] to 15 years [21]. The studies, however, did not describe the weaning protocols.
Overall, the studies did not specify any objective criteria for brace prescription for adult scoliosis patients. Therefore, there are no generally agreed-on prescription protocols for braces for adult scoliosis patients. We thus attempt to propose a protocol for adult scoliosis bracing based on more objective radiological parameters.
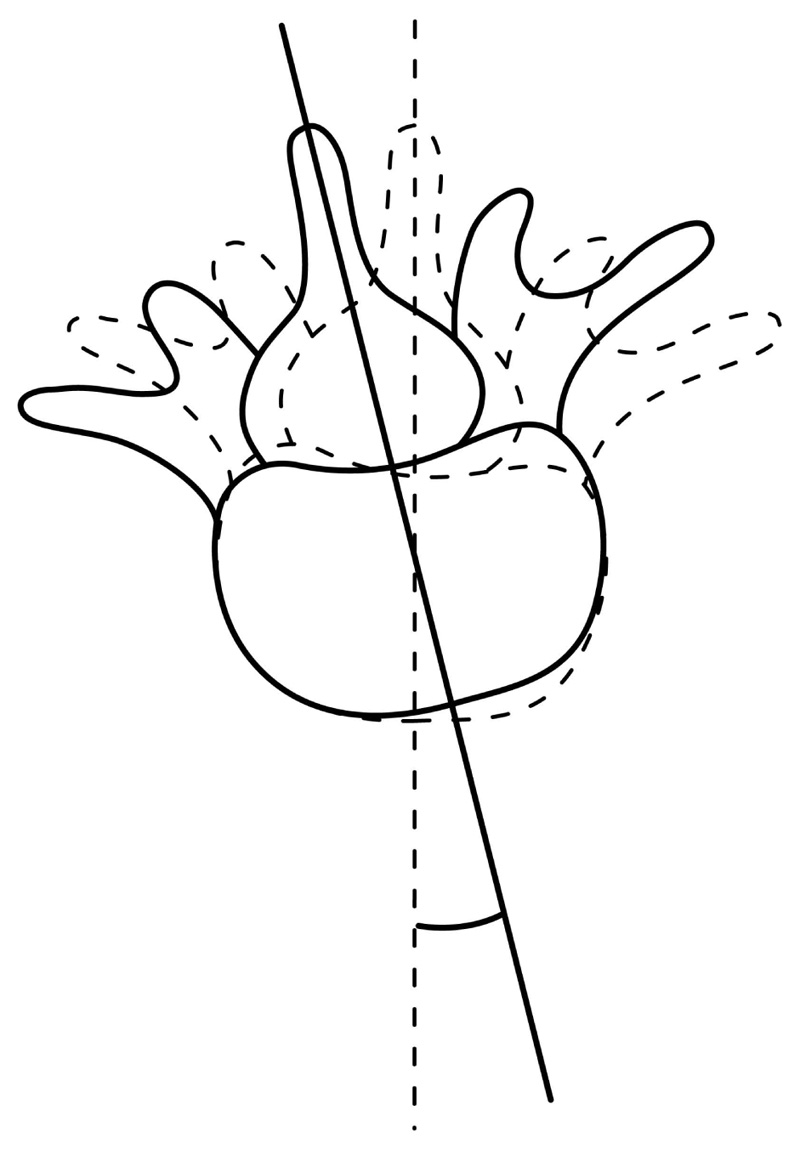
Many radiological parameters have been found to associate with low back pain. Low back pain is more frequently associated with double scoliosis, thoracolumbar and lumbar curves, and less often with the thoracic curve. Lumbar rotatory olisthesis over 5mm [25, 26], thoracolumbar or lumbar curve over 30o, apical lumbar vertebral rotation over 33%, and a low intercristal line [27] are associated with more frequent low back pain and radiculopathy. Recently, Ferrero et al. [28] showed that DLS patients with axial intervertebral rotation (AIR) at apex over 10o had significantly worse Oswestry Disability index (ODI) and more low back pain. The association is understandable as the AIR in the upper and lower junctions of the scoliosis curve subject the curve to torque (Fig. 1), increasing lateral scoliotic deviation [28].
Sagittal radiological parameters have also been found to correlate with disability. A pelvic tilt >22o and pelvic incidence-lumbar lordosis >10o are associated with disability [29], suggesting pelvic retroversion. The sagittal vertical axis (SVA), which is the distance between a plumb line dropped from C7 to the sacrum's posterosuperior angle, is also associated with clinical symptoms; the threshold relating to clinical symptoms is variably reported to be 43mm [29] and 70mm [30]. The increased SVA indicates a truncal forward shift relative to the pelvis to increase the size of the spinal canal and reduce neurologic insult, especially in the presence of degenerative spondylolisthesis [31]. Yet, it is of note that SVA can be diminished by pelvic retroversion. Thus, SVA and pelvic retroversion must be considered together [32]. T1 pelvic angle, which integrates the forward trunk inclination and the pelvis compensation, may be a better parameter than SVA [33]. It is less influenced by posture [33] and has been found to correlate strongly with the SVA, pelvic tilt, and pelvic incidence lumbar lordosis mismatch (PI-LL) [34].
Some of the above radiological parameters may correlate with curve progression. A lumbar rotatory olisthesis of more than 6mm, thoracolumbar or lumbar curve >30o, apical vertebral rotation >33%, and a low intercristal line signify a higher propensity for scoliosis curve progression [35-38]. A recent study showed that the magnitude of the Cobb angle and the level of the intercristal line bear no relationship to the risk of curve progression in patients with adult spinal deformity [39]. However, a truncal shift of 5mm to the left of the central sacral line (CSL) in the presence of a left thoracolumbar or lumbar curve is a risk factor for curve progression [40]. The curve progression is associated with a significant coronal shift of L1 from CSL [41].
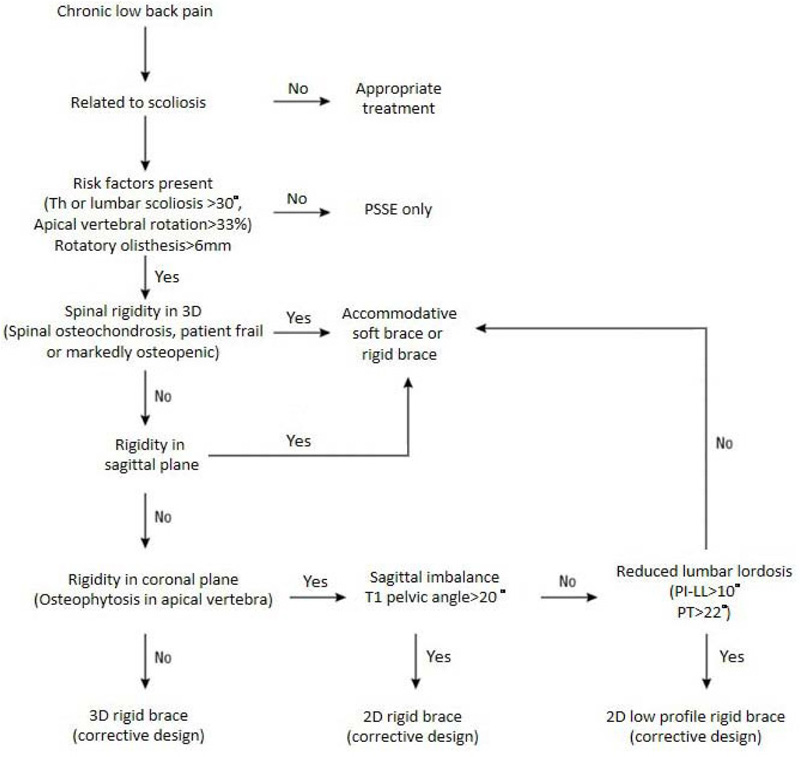
In many instances, patients do not have prior radiographs. Documentation of the rate of progression of the curve as a justification for bracing would thus be challenging, especially when adult IS patients have a long history of scoliosis, and progression over the years may not be linear [42, 43]. Therefore, it is proposed that adult scoliosis patients with sagittal imbalance, reduced lumbar lordosis, and radiological parameters associated with a higher risk of curve progression or low back pain are indicated for brace treatment (Fig. 2). It has to be noted that low back pain in a scoliotic patient does not equate that the pain must be related to scoliosis [44]. Before the brace prescription, a proper evaluation should ensure that the pain is secondary to the spinal deformity and not other causes.
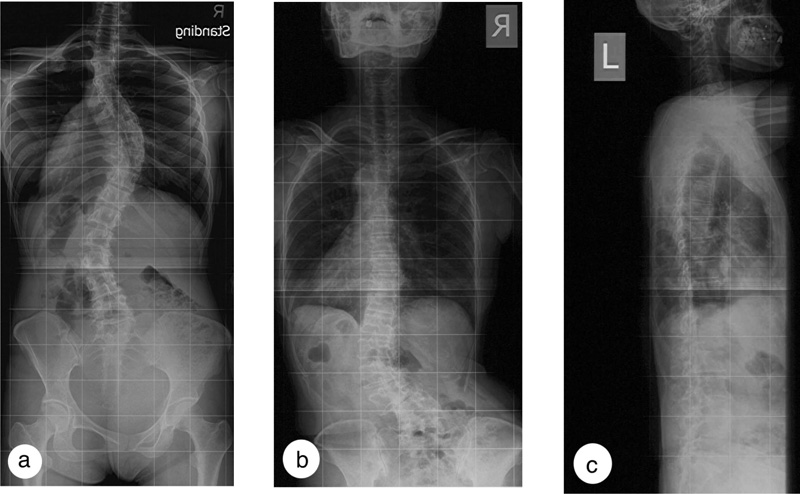
Whether the brace should be accommodative or corrective depends on the deformities and spinal rigidity and not on the patients’ body habitus. At present, it is clinically challenging to grade lumbar rigidity. The presence of marked arthritic or osteochondral changes suggests an increased spinal rigidity. An accommodative brace should be prescribed when the curve is rigid [17, 18] or in the presence of rotatory olisthesis to help stabilize the spine (Fig. 3). When the elastic brace cannot provide the needed support because of a mismatch of the spinal contour, a custom accommodative rigid brace may be prescribed to provide spinal support and limit motion, particularly in patients with more severe curves. Coupled movements in the lumbar spines are higher in DLS patients, particularly with larger curves, in most loading directions than in the lumbar spine with no scoliosis [45].
When the scoliotic deformity is rigid coronally but flexible in the sagittal plane, a rigid two-dimensional sagittal realignment brace may be prescribed to improve sagittal balance while accommodating deformities in the coronal and transverse planes. The sagittal spinal parameters worsen in patients with ASD with age; the change predominantly involves reducing lumbar lordosis, though the reduction is not statistically significant [39].
However, when the scoliosis curve is flexible, as in young adults and peri-menopausal patients, a 3D rigid brace with a corrective design may be prescribed.
The duration of daily wear depends on the severity of the symptoms and the extent of the spinal deformities. Weiss et al. [24] showed that brace wear 4-8 hours daily did not significantly improve low back pain. However, an increase in dose to 20 hours daily significantly improved the outcome [11]. De Mauroy et al. [12, 21] reported similar findings, who braced the patients for 24 hours per day in the first three weeks using a plaster cast and more than 4 hours daily after that. In the presence of radiological parameters indicative of curve progression, loss of lumbar lordosis, sagittal spinal imbalance, and increased risk of low back pain, the authors suggest wearing the brace during the daytime, for at least 14 hours a day, to reduce the axial deforming loading of body weight on the spine [46]. It has to be noted that the hours of wear were reported by patients and were not measured objectively by thermal or pressure sensors.
As in brace treatment of adolescent IS [47], daily core strengthening exercises should be prescribed to avoid deconditioning the lumbar paraspinal muscles and postural collapse during brace wear and after brace weaning, as sarcopenia is a risk factor in the progression of adult scoliosis. In addition, patients should learn diaphragmatic and de-rotational breathing to strengthen the deep lumbar muscles, enhance spinal stability, and reduce vertebral rotation and torque from the scoliosis curve [48, 49]. Also, they have to perform exercises to improve the spine's sagittal alignment and adopt proper sitting postures to reduce lumbar intervertebral disc pressure [50]. Treatment should also be given for osteopenia or osteoporosis [51].
Weiss et al. [24] and de Mauroy et al. [12, 21] reported having patients wearing the brace for six months before weaning. Our clinical experience concurred with the findings; we propose that the corrective brace be worn for 14 hours per day for at least six months or until the low back pain reduces to a level the patient can engage in daily activity with minimal pain before weaning. The wear time can be reduced by two hours every two months until the patient wears the brace for only 8 hours a day. A lateral spinal radiograph is then taken to determine the sagittal parameters. When no improvement is evident, the patient should not further reduce the daily brace wear; further weaning should depend on the outcome of the clinical evaluation. In the presence of sagittal parameters improvement, the brace wear can be further reduced by two hours every two months until the brace is weaned off completely. The authors are not aware of any studies showing changes in sagittal alignment with braces. However, the importance of improving the sagittal spinal parameters was brought forward by Pizones et al. [52]. A study on adult scoliosis surgery showed that the surgery should restore the ideal Rousoully sagittal profile associated with decreased mechanical complications, especially in patients over 65 [52]. In addition, the brace should target restoring the spinopelvic relationship and zero out the compensatory mechanism, improving the lumbar lordosis and pelvic tilt [53]. On the other hand, the accommodative brace is proposed to be worn when required.
The proposed clinical guidelines for adult scoliosis brace have limitations [10]. They are empirical and are not evidence-based. More studies are required to establish the effectiveness and dosage of adult bracing to manage chronic low back pain in adult scoliosis patients. Subjects should preferably be more homogenous, as the response of adult IS patients to bracing may be very much different from that of DLS patients, and different curve types respond to bracing differently.
CONCLUSION
Our search showed no objective criteria or clear indications concerning the prescription of the types of braces, daily wearing time, and duration of the intervention for adult scoliosis. Therefore research is required to determine the effectiveness and protocols of bracing in managing adult scoliosis patients, particularly those with thoracolumbar curves.
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


