All published articles of this journal are available on ScienceDirect.
Clinical and Radiographic Features of Phalangeal Osteoid Osteoma
EDITORIAL
The purpose of this editorial is to perform an extensive review of the relevant international literature about the clinical and radiographic features of phalangeal osteoid osteomas of the hand or foot, to indicate the value of clinical suspicion for the early diagnosis since they commonly appear with atypical findings, and to present four illustrative cases, two adults and two children.
Osteoid osteoma is a benign osteoblastic tumor of unknown origin. It usually affects children, adolescents and young adults showing a strong male predominance. The tumor has a predilection for the metaphysis or diaphysis of long bones of the lower limbs but it may occur anywhere in the skeleton. It typically consists of a well-demarcated radiolucent rarefied area of bone-forming and prostaglandin-secreting nidus, occupying the midcortex, which is surrounded by an extensive fusiform reactive sclerotic host bone. Reactive sclerosis is usually more pronounced in children. The lesion may also be found in the medulla (spongiosa) of bone. In the cortical presentation, it may rarely occupy the endosteal or subperiosteal surface of the cortex. Intramedullary tumors are usually surrounded by a thin rim of reactive sclerosis and may frequently be periarticular or intraarticular, presenting with synovitis and joint effusion [1-10].
Approximately 10% of osteoid osteomas involve the hand. Of them, 6% occur in the phalanges, 2% in the metacarpals and 2% in the carpal bones. Cortical localization of the tumor is usually seen in the phalanges and metacarpals, while intramedullary lesions are usually encountered in the carpal bones [11-23]. In the fingers, the proximal phalanx is the most typically affected site, while lesions of the distal phalanx are rarely encountered. The index finger is the most commonly involved digit, while the thumb is the least affected one [24-41]. Phalangeal lesions of the foot account for about 2% of all cases [42-47].
In an accessible bone, swelling over an osteoid osteoma is a typical finding. In a phalangeal osteoid osteoma, swelling may be localized or generalized, resembling dactylitis or macrodactyly. Whenever the lesion affects the terminal phalanx, enlargement of the entire fingertip, producing clubbing, appears to be very likely [24, 41, 48-54]. The presentation of clubbing in a digit should raise the suspicion of a bone tumor, even when plain radiographs show only soft tissue swelling or vague radiographic changes [55]. Both the enlargement of the finger and the hypertrophy of the nail may be explained by the increased focal vascularity [49]. Osteoid osteomas localized in the subungual area have also been reported [56]. An accompanying erythema of the overlying skin may rarely be detected. Cases associated with either erythema or nail deformities may easily mislead the diagnosis [57-59].
Nocturnal pain and exquisite tenderness over the site of the nidus are the most constant clinical features of phalangeal osteoid osteomas of the hand or foot. Pain is unrelated to use or motion and it may precede the radiographic changes by many months [60]. The severity of pain may increase gradually, so that it may take months or even more than a year before a patient seeks medical advice. The pain is typically worse at night and is usually relieved by small doses of acetylsalicylic acid (aspirin) or nonsteroidal anti-inflammatory drugs (NSAIDs). The use of both may be gradually less effective in reducing pain to an acceptable level. On occasions, pain may not be worse at night or may not be relieved at all by these medications. The appearance of an atypical type of pain (dull, vague or diffuse) and the absolute lack of pain are exceptionally rare in non-phalangeal osteoid osteomas. Painless osteoid osteomas appear in the digits more frequently than in any other skeletal location [56, 61-64]. Vasomotor disturbances, namely increased skin temperature in the affected region, and profuse digital tip perspiration or intense autonomic phenomena, which may mimic peripheral nerve compression or reflex sympathetic dystrophy have also been reported [48].
A common diagnostic problem of juxtaarticular or intraarticular phalangeal osteoid osteomas is that they may present as monoarticular interphalangeal arthritis with decreased range of motion (ROM). This presentation may also misdirect the diagnosis of a phalangeal osteoid osteoma to monoarticular juvenile idiopathic arthritis [55, 65-68].
Conventional radiographs remain the most important imaging study of the suspected lesion. Plain radiograps may demonstrate the typical finding of a phalangeal osteoid osteoma, which is a radiolucent nidus, usually less than 1 cm at its greatest dimension, localized within the cortex. Nidus identification is of decisive importance for diagnosis and treatment. Surrounding dense sclerosis or extensive periosteal reaction may overshadow the nidus, indicating the diagnosis of an obscure phalangeal osteoid osteoma [55, 69-71]. Such cases may be confused with malignancy [72]. One theory to account for the discrepancy in findings between studies is the possibility that the nidus simply becomes more visible with time [37, 55]. With time, the nidus matures and becomes calcified and more radiopaque. Ossification of the nidus usually starts from the center, producing a central zone of density surrounded by a ringlike band of radiolucent zone (ring sequestrum sign or annular sequestrum of Jaffe) [2, 73, 74]. The radiographic sign of sclerosis may take many years after excision of the nidus to subside, but eventually, it does [75]. Unlike osteoid osteomas of the long bones that show clear demarcation between the nidus and the reactive bone, phalangeal lesions may not be well defined [24, 33, 50, 55]. A relative absence of dense reactive bone surrounding the nidus is a common radiographic appearance of a cortical phalangeal lesion [37, 50, 51, 55, 76]. Cases with relative absence of sclerosis are more likely to indicate a diagnosis of subacute osteomyelitis [77]. Local osteopenia from disuse and the intraarticular location of the lesion have been proposed as potential causes for the lack of reactive sclerosis [33, 76]. Periosteal reaction may be evident in 65% of cases. The lack of periosteal reaction may be due to the close proximity of the tumor to the interphalangeal joint [37], while in lesions localized to the distal phalanges may be due to the poorly developed periosteum in the region [55]. The presence of thickened Sharpey’s fibres may also explain the absence of periosteal reaction associated with osteoid osteomas in the distal phalanges [59, 78]. Phalangeal osteoid osteoma with a double-nidus has also been reported [79].
The diagnosis of intramedullary, subperiosteal or periarticular [73, 80-90] phalangeal osteoid osteomas is particularly difficult since both the clinical symptoms and the radiographic findings may be minimal, absent or unspecific. Intramedullary osteoid osteomas are usually well-circumscribed, the reactive bone surrounding the nidus is less pronounced and the nidus may be partially or completely calcified. Subperiosteal or exostotic osteoid osteoma is the rarest type and usually presents as a soft tissue mass adjacent to or eroding the bony cortex. Reactive sclerosis is much more pronounced than in intramedullary and periarticular lesions [30, 81, 83].
Conventional tomography may serve as a valued adjunct to plain radiography. A 3-phase Technetium-99m MDP bone scan is of considerable value since it demonstrates the intense focal increase in uptake by the nidus. Once the lesion has been localized by bone scan, cross sectional and three-dimensional imaging with Computed Tomography (CT) is usually used. Magnetic Resonance Imaging (MRI) will demonstrate the soft tissue and bone marrow edema but is rarely needed, because CT both better demonstrates the nidus and aids in differentiating between the nidus and reactive bone. The use of angiography may also result in improved recognition of the nidus [75, 91-94]. Atypical histological features may also be often encountered in phalangeal osteoid osteomas in both children and adults, such as ill demarcation between the nidus and reactive bone, and absence of dense reactive bone surrounding the nidus [55, 95-102].
The main differential diagnosis in a patient with a painful fingertip swelling may include whitlow or paronychia, osteomyelitis, glomus tumour, subungual exostosis, osteochondroma, enchondroma, osteoid osteoma, and arthritis [29, 50, 55, 56, 59], In addition, in cases with a painful nontraumatic swelling of the proximal or middle phalanx differential diagnosis includes soft tissue lesions, bone abscess and osteomyelitis of acute or chronic sclerosing types, monoarticular rheumatoid arthritis, enostosis (bone island), stress fracture, benign bone tumors, and malignancy [23, 30, 78, 79, 103, 104].
There has been no report of malignant transformation of this neoplasm so far. A complication of phalangeal osteoid osteoma, which has rarely been reported, is premature physeal fusion [49, 105, 106]. In a two children report, in the one of them local damage to the phalangeal physeal plate by the lesion could be excluded [107]. Therefore, other etiological factors were considered, such as the local increase in vascularity or the regional osteoporosis [108], in a similar way that they were encountered in epiphyses around the knee in treated tuberculosis of the hip [109]. Distant recurrence of the tumor is extremely rare with only one reported case [110]. Local recurrence of the clinical symptoms and a new nidus will form following inadequate treatment [91, 111, 112]. Cases localized in a juxtacortical area of the articular surface that necessitate removal of an articular area are more prone to complications [75].
Four patients with a histologically proven phalangeal osteoid osteoma of a finger or toe are presented. The clinical findings were assessed for localized or generalized swelling, for the presence/type of pain and for interphalangeal arthritis associated with decreased ROM. The evaluated radiographic features were identification of a radiolucent nidus, internal matrix within the nidus, sclerosis surrounding the nidus, periosteal reaction, periosteal/cortical sclerosis, and cortical erosion.
There were two adult male patients, 21 (patient 1) and 23 (patient 2) years of age, respectively in Figs. (1 and 2). Two children, a 12-year-old boy (patient 3) and a 13-year-old girl (patient 4) were also identified (Figs. 3 and 4). In the two adult patients, the tumor involved the thumb and middle finger, respectively. In the two children, the great toe and the index finger were involved, respectively. The tumor was localized in the distal portion of the proximal phalanx in all cases. Swelling, pain and local tenderness were the presenting symptoms. Swelling was localized in 3 patients and generalized, in the form of dactylitis, only in patient 1. The cardinal feature of night pain as well as local tenderness over the nidus was evident in all cases. However, complete relief of pain with the use of aspirin or other NSAIDs was noted only in patient 1. No erythema or local increase in temperature was detected in any of the patients. The adjacent proximal interphalangeal joint was very tender and had limited ROM in all cases. Precise localization of the nidus was determined in patients 1, 2 and 3 with conventional radiography and in patient 4 with MRI. An intracortical localization of the nidus was noted in patients 2 and 3, while an intramedullary one was noted in patients 1 and 4. A distinctive area of sclerosis surrounding the lytic lesion was seen only in the adult patients. Minimal and absent sclerosis were evident in patients 3 and 4, respectively. Internal sclerosing matrix within the nidus and the ring sequestrum sign were evident on the radiographs in the adult patients, while in patients 3 and 4, both findings were delineated with the use of CT and MRI, respectively. Cortical/periosteal sclerosis was present in patients 1, 2 and 4. Cortical erosion as well as local osteopenia was not identified in any of the patients.
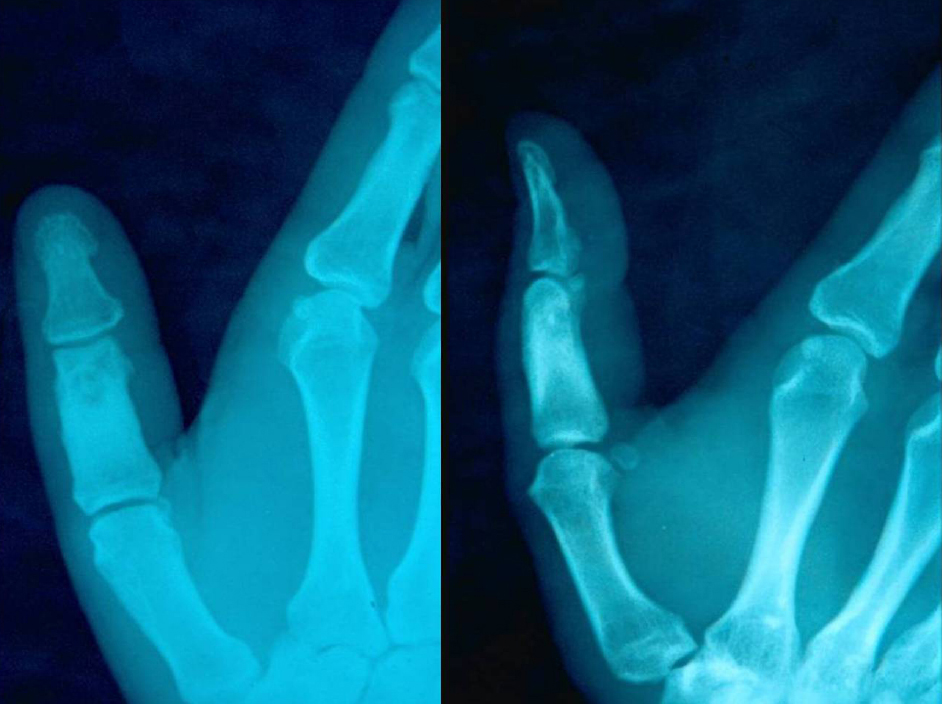



The clinical and the radiographic findings in both adult patients indicated the diagnosis of a phalangeal osteoid osteoma. However, the clinical and radiographic evaluation in both children yielded nonspecific results. Thus, the diagnosis of osteomyelitis could not be excluded in patient 3, while in patient 4 the findings were not sufficient to make a differential diagnosis from osteomyelitis or malignancy.
CONCLUSION
It has strongly been emphasized in the literature that phalangeal osteoid osteoma may commonly present with atypical clinical and/or radiographic findings in both adults and children. In such cases, clinical suspicion remains the most sensitive indicator for diagnosis. Furthermore, imaging evaluation including conventional tomography, bone scintigraphy, CT, which has the highest specificity, and MRI is mandatory in patients presenting with atypical or no radiographic findings as well as in patients with atypical clinical findings, such as a phalangeal painless swelling, clubbing of the fingertip, dactylitis or macrodactyly, and monoarticular interphalangeal arthritis. Awareness of the potential atypical clinical and/or radiographic characteristics of the phalangeal osteoid osteoma of the hand or foot may lead to earlier diagnosis and treatment in both adults and children.
FUNDING
None.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


