All published articles of this journal are available on ScienceDirect.
Traumatic Heel Pad Avulsion in a Pediatric Patient
Abstract
Introduction:
Heel pad injuries can have devastating and debilitating consequences. All efforts to primarily reapproximate the heel pad should be undertaken. Reconstruction of the heel pad can often require multiple complex surgeries including microvascular flaps and tissue transfers. There is a paucity of successful techniques for primary repair in the literature.
Case Presentation:
In this case report, we describe the successful use of polydioxanone suture with sterile buttons for the repair of the heel pad in a pediatric patient. An 8-year-old male was struck by a vehicle, sustaining a full-thickness heel pad avulsion injury measuring approximately 16-cm in length. The soft tissue was sharply debrided and repaired primarily to the calcaneal periosteum using #1 polydioxanone suture with external suture buttons, and an incisional wound VAC was applied. He was placed into a long-leg bent knee cast and kept non-weight bearing for a total of 6 weeks, at which time the suture and buttons were removed and he was progressed to weight bearing as tolerated in a walking boot. At the 6-month follow-up examination, the heel pad was viable and well-fixed; the patient reported no pain and was not limited in any chosen activities.
Conclusion:
This construct was shown to provide effective fixation while mitigating reported concerns of tissue necrosis caused by suture repair. At 1 year from injury, the patient’s mother noted a slight limp with running but not with walking. He reported no pain at any time, and his Oxford Ankle-Foot Questionnaire for Children score was 58, indicating excellent patient-reported outcome following his procedures.
1. INTRODUCTION AND BACKGROUND
Traumatic injury to the heel pad can be devastating and potentially limb-threatening. The structure of the heel pad has uniquely evolved to accommodate its primary function: load-bearing. Approximately 50% of an individual’s weight is transmitted through this area during the gait cycle [1]. As a result, the heel’s structure has developed into a complex array, or “honeycomb,” of vascular septae, which encloses closely packed compartments of fat [2]. The septate nature of the pad allows for significant resistance to shear and frictional forces in a similar fashion to that of fingertips [3]. The heel pad is difficult to reconstruct or substitute, in part, because of its unique structure and the significant mechanical demands placed on this area. All efforts should be undertaken to primarily repair the heel pad in the case of partial avulsion with intact sensation and adequate vascular supply [2, 3].
There are a variety of techniques described in the literature for flap reconstruction of the heal pad; however, successful primary repair techniques are significantly fewer in number. Mohammad et al published a case series of 4 patients describing the use of multiple Kirschner wires for stabilization of the avulsed heal pad, which resulted in successful healing with good patient outcomes [2]. The use of sutures to repair and stabilize the avulsed heel pad back to the calcaneus is often discounted as a viable option due to a lack of strength of the construct and associated increased pressure on wounds and the skin, possibly leading to wound breakdown and necrosis [2, 4, 5]. This report describes the successful repair of the heel pad of a pediatric patient and is the first report in the literature, to our knowledge, of a method using only suture and suture buttons.
2. CASE REPORT
An 8-year-old African American male was brought to the Pediatric Emergency Department after being struck by a motor vehicle. Physical examination revealed a deformity to the right lower extremity at the middle portion of the leg and significant soft tissue injuries involving both the mid-portion of the leg and the heel pad. Radiographs of the right lower extremity demonstrated a transverse, displaced midshaft tibia fracture and a nondisplaced transverse calcaneus fracture (Fig. 1). The patient had sustained a Gustilo Anderson Type II tibial shaft fracture, a Gustilo Anderson Type III calcaneus fracture, and a full-thickness heel pad avulsion of the right foot measuring approximately 16 centimeters in total length (Fig. 2).


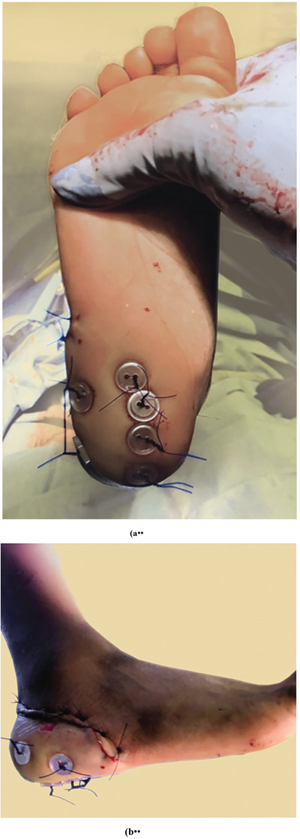
In the operating room, surgeons performed a sharp excisional debridement of the open wounds followed by thorough irrigation with sterile saline. The tibial shaft fracture was stabilized with two 3.5-millimeter intramedullary flexible rods. No internal fixation was necessary for the calcaneus fracture. Attention was then directed to the heel pad. After performing a thorough sharp debridement, 6 polydioxanone sutures (PDS #1) were placed in a loop fashion through the calcaneal fat pad and the calcaneus periosteum before being passed out of the skin. Additional PDS suture was used to approximate the skin edges of the laceration, and 2-0 nylon suture was used in a Donati-Allgower fashion to obtain complete closure. Following the closure of the traumatic wound, the PDS sutures securing the heel pad were passed through sterile surgical buttons and were tensioned across the heel pad in order to secure it in place (Figs. 3a, 3b). Careful attention was directed to providing sufficient tension for secure placement without excessive tension in order to prevent necrosis of the skin underlying the buttons. A negative pressure suction device set at 50 mmHg of continuous pressure was placed over the wounds, and a posterior splint was placed.

The patient remained in the hospital for an additional 6 days in order to maintain his negative pressure wound device. His hospital course was unremarkable; he progressed well in physical therapy with non-weight bearing restrictions on the operative extremity.
At 10 days postoperatively, the patient presented to the clinic for a soft tissue examination, which demonstrated healing of his traumatic lacerations and maintenance of his heel pad repair. He was placed into a long leg bent-knee cast and was instructed to remain non-weight bearing. At 4 weeks following injury, radiographs of the right tibia demonstrated anatomic alignment of the tibial fracture with early callus formation. At 6 weeks postoperatively, his heel pad remained viable and the suture and buttons were removed. A dry dressing was applied and the patient was allowed to transition into a cam boot and become weight bearing as tolerated. At the 6-month postoperative visit, the patient’s heel pad remained viable, fixed, and with intact sensation to light touch (Fig. 4) (Video S1). He was ambulating effectively with a reciprocal heel-toe gait and without any reported pain. He could also perform a 2-legged heel rise without discomfort (Video S2). He was then released to full activity as tolerated and instructed to follow-up as needed. At 1 year from injury, the patient’s mother noted a slight limp with running but not with walking. He reported no pain at any time, and his Oxford Ankle-Foot Questionnaire for Children score was 58, indicating excellent patient-reported outcome following his procedures.
3. DISCUSSION
Trauma to the heel pad can be a limb-threatening injury. The soft tissue of the heel pad has evolved to form a complex “honeycomb” structure, which allows for accommodation to the significant mechanical forces transmitted through the area [3, 4]. This, in addition to the complex vascular network transmitted through these septae, results in an area that is difficult to replicate with soft tissue transfer or flap reconstruction [1]. Although there are documented successful reconstructive flap techniques, care should be taken to evaluate the extent of soft tissue injury and neurovascular status with the goal of primary repair of the heel pad if at all possible [2]. There are few documented techniques regarding the repair of the heel pad with successful healing. Suture repair is often dismissed as a viable option in the literature due to theoretical decreased relative strength and increased pressure on the skin, which can lead to soft tissue necrosis and eventual infection or failure requiring further surgery [2, 4, 5]. As the calcaneal periosteum has a significant plexus of blood vessels, the thicker periosteum of adolescent patients can contribute to a greater potential for healing [3]. It also provides a strong anchor for primary suture repair as evidenced in this case. The sterile buttons used here provide an increased surface area at the suture-skin interface, allowing for a greater disbursement of force and a decreased risk of focal skin necrosis.
CONCLUSION
The primary repair technique used in this case was successful and allowed this patient to retain his native, sensate, and mechanically specialized heel pad with little to no morbidity. We believe this method is widely applicable in the case of incomplete avulsions similar to that of the Kirshner wire method described by Mohammed et al [2], at least in the case of pediatric patients. It remains to be seen whether this technique can be applied to the adult patient successfully; however, this would be a worthwhile point of study as this is a cost-conscious, simple technique that avoids the morbidity associated with microsurgical techniques.
ETHICS APPROVAL AND CONSENT TO PARTICIAPTE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Informed consent was obtained from the mother of the patient.
STANDARD OF REPORTING
CARE guidelines have been followed.
FUNDING
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
CONFLICT OF INTEREST
The authors have nothing to declare. The authors, or any member of their family, have not received any financial remuneration related to the subject of the article.
ACKNOWLEDGEMENTS
The authors would like to thank the Hughston Foundation for their assistance with medical illustrations, video, and manuscript editing.
SUPPLEMENTARY MATERIAL
Supplementary material is available on the publisher’s website along with the published article.


