REVIEW ARTICLE
General Principles of the Surgical Management of Juvenile Inflammatory Arthritis
Mark P. Figgie1, *, Barbara A. Kahn1, Jason L. Blevins1, Matthew P. Abdel2
Article Information
Identifiers and Pagination:
Year: 2020Volume: 14
First Page: 150
Last Page: 153
Publisher ID: TOORTHJ-14-150
DOI: 10.2174/1874325002014010150
Article History:
Received Date: 26/02/2020Revision Received Date: 01/07/2020
Acceptance Date: 24/08/2020
Electronic publication date: 25/11/2020
Collection year: 2020

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Surgical management of Juvenile Inflammatory Arthritis (JIA) presents many challenges for the patient, healthcare team and especially the orthopedic surgeon. Collaborative care efforts must be endorsed early on in order to facilitate maximal postoperative functional ability. Developmental levels, both physically and emotionally must be established preoperatively. It is important to determine bone age and growth plate closure to establish the best surgical intervention and avoid leg-length discrepancies later in life. Emotional maturity may impede the ability of the patient to manage pain or follow directions throughout the recuperative process. Surgical challenges require a team approach that includes rheumatologists who can manage disease modifying agents and the effects of discontinuing medications or planning surgery around dosing regimens in order to decrease immunosuppression. Managing multiple joint issues will require an expert team of occupational and physical therapists to prepare adaptive devices and rehabilitate patients who have significant functional limitations and decreased muscular strength. Because of an anticipated longer and more difficult recovery for JIA patients, case managers must engage in support systems and plan for postoperative care prior to surgery. Implant specific devices need to accommodate small bone structure, bone loss and complex deformities along with diaphyseal or epiphyseal dysplasia. Neurologic assessments will avoid cervical spine compromise during anesthesia administration. Bilateral procedures in the lower extremities should be considered whenever flexion contractures are present and should take place prior to upper extremity joint replacements. Restoring function to the hand and wrist takes priority over elbow and shoulder replacement, respectively. The key factors of appropriate surgical management in JIA patients are to decrease pain, restore function and avoid loss of ambulation at a young age. Extensive preoperative planning and communication with the patient, support system and healthcare team are warranted to address the complexities in this patient population.
1. INTRODUCTION
Surgical treatment of Juvenile Inflammatory Arthritis (JIA) is one of the most challenging conditions in musculoskeletal disorders. These patients often have complex deformities and issues surrounding future growth potential and leg length discrepancies, which must be considered in reconstructive planning. Many JIA patients may have a limited ability to comprehend the risks and potential future complications associated with these procedures due to their young age, making the timing of surgery critical. Several studies have shown that patients who are older at the time of surgical intervention have improved outcomes [1]. However, some patients require surgery at an earlier age in order to prevent significant loss of bone stock or functional ability [1, 2]. If a patient develops severe flexion contractures of the hips and becomes non-ambulatory for greater than three months, the urgency for surgery becomes escalated in order to restore the ability to ambulate. If the patient stops walking for over 3-6 months, it is extremely difficult to restore independent ambulation.
2. TIMING OF SURGERY
Patients often require surgery prior to growth plate closure, which presents a risk for the development of leg length discrepancies. Determination of bone age with the calculation of predicted leg length discrepancy should be accounted for in reconstructive templating and counseling. In some instances, there is hyperemia of the joint, resulting in overgrowth for a temporary time before the growth plates close. This may result in a longer leg on the affected side. Typically, the operative side is not shortened because it may result in weakness or instability of the hip. Projecting how much growth remains on the contralateral side is challenging. It is important to anticipate future surgical interventions that may be necessary on the opposite side and consider the development of flexion contractures of either leg, which may also confound the determination of leg length discrepancy.
Patient age at the time of surgery is important because of the patient’s future growth potential. Younger patients may have difficulty comprehending their surgery and rehabilitative requirements, and younger patients may have difficulty with managing pain leading to potentially poor outcomes.
3. PRE-OPERATIVE PLANNING
The care of the patient with JIA requires collaboration between the pediatric rheumatologist, orthopaedic surgeon, anesthesiologist, physical and occupational therapists, and case manager along with psychological support to help the patient deal with the difficulties coping with their disease [3]. The rheumatologist and surgeon must work together to determine what procedure is appropriate and how to optimize timing to avoid flares. The handling of perioperative medications is extremely important for these patients. The orthopedic surgeon needs to be experienced with the disease process and surgical challenges of JIA. Surgeons should be capable of a wide range of procedures including arthroscopy, arthroplasty, and arthrodesis, to manage the variety of joint pathologies that these patients commonly present with in the office. An anesthesiologist who is experienced with regional anesthesia is critical. It is best to avoid general anesthesia when possible due to the potential for cervical instability or difficulties in patients who may have an ankylosed cervical spine. These cases may require fiberoptic intubation. As such, regional anesthesia is preferable in the majority of these cases.
Occupational and physical therapists should evaluate the patients preoperatively in order to determine ambulatory status, provide a rehabilitation program, and to determine what equipment and devices may be needed postoperatively. Devices such as platform walkers, appropriate sized canes, walkers, and Continuous Passive Motion (CPM) machines need to be customized preoperatively. Upper extremity capabilities should be determined prior to lower extremity surgery to make sure that they have the grip strength and capability to handle assistive devices postoperatively. In many instances, device modifications are required to allow the patient to use assistive devices such as a cane or walker postoperatively. The case manager is important in evaluating the patient’s home situation and assists in determining the patient’s postoperative rehabilitation plan. Many of these patients require extensive postoperative rehabilitation, which should be organized prior to surgery. In patients who undergo bilateral total hip arthroplasties (THAs) and bilateral total knee arthroplasties (TKAs) in the same hospital stay, long-term care is critical to get the patient ambulatory again. Patients often struggle with the chronicity of their disease and may become depressed or lose motivation. In these instances, the intervention of a psychiatrist or psychologist can help them cope with their disease.
The decision to proceed with surgery should be based on the patient’s pain, function, bone loss, and progressive deformity. Loss of ambulation hastens the decision to proceed with surgical intervention. The extensive bone loss should be avoided as it may compromise the fixation of the implant and jeopardize the outcome of the joint replacement procedure. Significant flexion contractures should be corrected whenever possible in order to maximize the patient’s functional abilities.
Preoperative planning is critical in patients with JIA. In many instances, standard off-the-shelf implants will not fit properly due to small bone size and complex deformity. In the shoulder and elbow, standard size implants may not fit, which may compromise the fit and require a custom implant. In the hip, patients commonly present with extensive femoral neck anteversion, which cannot be corrected with standard implants. Either modular or custom designed implants may be required to ensure a proper fit. In the knee, extensive flexion contractures, external tibial rotation, and valgus deformities can be difficult to correct. Patients often have trumpet shaped femurs and tibias with wide medial-lateral and small anteroposterior dimensions. Custom implants may be required for proper fit resulting in higher costs due to the requirement of customized implants. In most instances, CT scans are critical in helping plan the sizing and positioning of the implants [4]. A skilled biomechanics engineer is required to help design and develop custom implants for these patients.
Thorough evaluation of the patient is required for a successful surgery. The patient’s surgical and medical history is important and the physical examination should be from head to toe with strength and range of motion assessments. Any signs of vascular insufficiency or potential infection need to be addressed preoperatively. A detailed neurologic exam is necessary to evaluate the patient’s cervical spine, as many of these patients have cervical spine involvement with ankylosis at several levels. We recommend flexion-extension cervical spine radiographs prior to any surgical intervention and consider an MRI if there are abnormalities noted on the cervical spine X-rays.
4. GENERAL PRINCIPLES
General principles of surgical treatment of JIA patients include maintaining the patient’s function (especially ambulatory abilities), establishing equal leg lengths, and correcting deformities. When indicated, bilateral procedures are often performed in the hips and knees in order to correct flexion deformities during the same surgery. Lower extremity surgery usually takes priority over upper extremity surgery in order to maintain ambulation. In addition, it is reasonable to avoid placing demands on the shoulder or elbow arthroplasty when patients need assistive devices after hip or knee surgery. We also try to combine surgical procedures whenever possible, to minimize the number of times a patient has to come to the hospital.
Establishing a functional hand and wrist should be considered before addressing the elbow and shoulder. A stable well aligned wrist should be established before the Metacarpal Phalangeal Joints (MCPs) and fingers are addressed. A flexion deformity at the wrist or ulnar deviation will put deforming forces on the MCPs and change the functional length of the tendons. Correction of the wrist will decrease the deforming forces on the MCPs and allow for a better outcome. There is disagreement as to whether or not to address the elbow or the shoulder first. The literature suggests that patients get a better functional outcome with the elbow than they do with the shoulder [5, 6]. This is because the biceps and triceps are usually in better condition than the rotator cuff of the shoulder. In our series, patients got better functional improvement with an elbow arthroplasty and sometimes decided not to proceed with the shoulder as a result. The one caveat is when the shoulder is so restricted in the rotation that patients will attempt to rotate through the elbow, which may cause early failure of the elbow arthroplasty. In these instances, the shoulder should either be replaced first or soon after the elbow arthroplasty is performed. Having a functional hand provides motivation for rehabilitating the shoulder and the elbow. We often will do the non-dominant side first so that the patient can continue to use the dominant side for activities of daily living. Patients then have the motivation to use the non-dominant side during the rehabilitation of the dominant side.
In the lower extremity, the first goal is to establish a pain-free plantigrade foot. If the hips and knees are replaced prior to achieving a plantigrade foot, ambulation will be compromised. Abnormal forces are put on the knee if the foot is in equinus by either forcing the knee into hyperextension or compensating with a matching knee flexion deformity. JIA patients often have a cavovarus hindfoot and in some instances it may be difficult to correct if the knee is in considerable valgus or varus. In these instances, we often perform the TKA followed closely by a hindfoot correction. Once the knee is well aligned, it is easier to correct the hindfoot deformity and it is more likely to heal in a properly aligned position without further deforming forces from the knee. In cases where the knee and the hip are both involved, we prefer to address the hips before the knees in order to allow for improved hip range of motion. It is difficult to rehabilitate the knee if the hip does not extend. If patients have flexion contractures of the hips, they will often get matching flexion contractures of the knees when they try to ambulate. If both hips are involved we try to correct both hips in the same surgery. In cases where both knees are also involved, we will often address the knees within a week of addressing the hips. There is a case report of doing all four joints in one surgery, but we feel it is better tolerated to do both hips followed by both knees a week to 10 days later [7].
4.1. Case Example
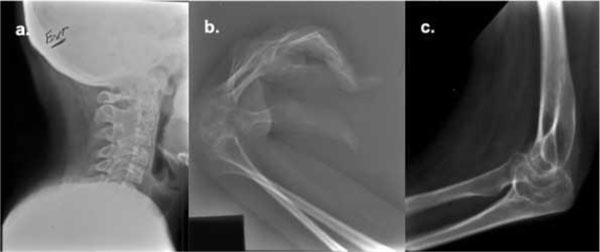
A 17-year-old female with JIA presented with an inability to walk and perform activities of daily living. Her parents had divorced as a result of conflicts over her care and she had not ambulated for the last three years. She had ankylosis of her cervical spine and both elbows in addition to fixed flexion deformities of both wrists, both hips, and both knees (Figs. 1 and 2). She also had equinovarus deformities of both feet (Fig. 2c). Our first goal was to reestablish a range of motion of the elbows and correct her feet. She underwent a right custom non-cemented total elbow arthroplasty (Fig. 3c) and left hindfoot osteotomy to bring her into plantigrade alignment. One week later, we performed a left total elbow arthroplasty and a right hindfoot osteotomy. Once the hindfeet had healed, she underwent staged bilateral total hip arthroplasties and bilateral total knee arthroplasties one week apart (Fig. 3a-b). Postoperatively, she had a prolonged recovery and required the tilt table in order to stand. She required several months of rehabilitation but ultimately became an independent ambulator and graduated from high school and college and was able to live independently. This case illustrates how proper planning and surgical staging can lead to a satisfactory outcome in these challenging cases.
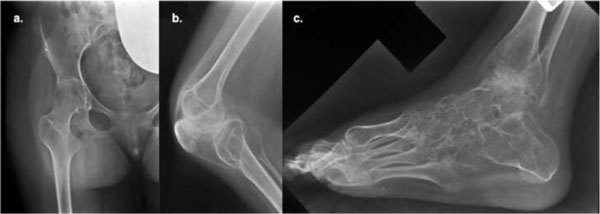 |
Fig. (2). Preoperative radiographs including an anteroposterior view of the right hip (a), lateral view of the right knee (b), and lateral view of the right foot (c). |
LIST OF ABBREVIATIONS
| (JIA) | = Juvenile Inflammatory Arthritis |
| (CPM) | = Continuous Passive Motion |
| (THA) | = Total Hip Arthroplasty |
| (TKA) | = Total Knee Arthroplasty |
| (MCP) | = Metacarpal Phalangeal Joints |
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.