All published articles of this journal are available on ScienceDirect.
Kinematic Differences between Two Types of Forward Elevations of the Shoulder Joint: Flexion and Reaching Elevation
Abstract
Background:
Extension of the elbow joint is maintained during shoulder flexion. In contrast, the arm starts from the flexed position of the elbow joint and the joint gradually extends during reaching elevation.
Objectives:
This study aimed to compare the kinematic elements and electromyographic (EMG) activities of the rotator cuff muscles between flexion and reaching elevation.
Methods:
The study included 10 healthy young men. (average age, 21.5 ± 3.4 years), and measurements were performed on their dominant arms. A three-dimensional motion analyzer was used to record the following elements during shoulder flexion and reaching elevation: the angles of glenohumeral joint elevation and scapular upward rotation, scapulohumeral rhythm, external rotation of the humerus, and glenohumeral plane shifting from the coronal plane. The EMG activities in the supraspinatus, infraspinatus, subscapularis, and teres minor were recorded simultaneously.
Results:
The plane of reaching elevation was retained at 60° from the coronal plane. The glenohumeral planes (P < 0 .01) and the external rotation angles of the humerus below 90° of elevation (P < 0.05) were significantly different between both the motions. The EMG activities in the supraspinatus (P < .01), infraspinatus (P < 0.05), and teres minor (P < 0.01) were significantly lower while reaching elevation than those during flexion.
Conclusion:
The motion plane at 60° from the coronal plane, movement of the humeral external rotation, and EMG activities of the rotator cuff muscles were different during reaching elevation and shoulder flexion.
1. INTRODUCTION
In clinical and research settings, physicians examine shoulder flexion (flexion) or abduction while maintaining full extension of the elbow in patients with shoulder disorders or trauma. In previous studies, flexion, scaption, and abduction of the shoulder joint have been kinematically analyzed in normal subjects and in patients with impingement syndrome, rotator cuff tears, or stiff shoulder [1-4]. However, reaching elevation in activities of daily living includes two elements of motion in reaching with hands for an object via the shortest distance; the elevation starts from the flexed position of the elbow joint and the joint then extends gradually (Fig. 1). This motion is frequently observed in daily living and sports activities, such as reaching for a cup, lifting a heavy item, and making a shot in basketball. Thus, the upper limb movement starts by drawing the hand toward the body and then extending the arm and hand toward the target. In the present study, the arm elevation on the sagittal plane from the flexed position of the elbow joint is defined as reaching elevation, and the arm lifting with the maintained extension of the joint is denoted as flexion.
Many researchers have calculated the scapulohumeral rhythm during flexion using various methods [1, 2, 5-10]. The scapulohumeral rhythm in healthy shoulders (3:1) was not significantly different between the dominant and non-dominant shoulders [5, 7, 10]. In pathological shoulder conditions such as rotator cuff tears, frozen shoulder, or reverse total shoulder arthroplasty, the scapulohumeral rhythm decreased because of greater scapular motion [1, 4, 9]. The humeral head of the normal shoulder always rotates during shoulder movement. Ludewig et al. [3] reported that the glenohumeral joint motion caused external rotation of the humerus with an increase in the elevation angle, and that the angle of humeral external rotation during abduction was larger than that during flexion. Moreover, the periscapular and rotator cuff muscles participate in and coordinate during shoulder elevation and external rotation of the humerus [10-18].
The periscapular and rotator cuff muscles engage in elevation of the shoulder joint. The former muscles move the scapula and the latter work to depress and stabilize the humeral head to the glenoid fossa. The rotator cuff muscles are considered to be the primary dynamic stabilizer of the glenohumeral joint. The contraction of the muscles generates a compression force between the glenoid fossa and the humeral head, establishing a fulcrum around the major shoulder muscles [12, 19]. The lower subscapularis and teres minor have significantly higher muscle activity during shoulder elevation, which might reflect their greater role as a humeral head depressor and stabilizer [10, 11].
If there are differences in the kinematic elements (the plane of elevation, scapular motion, scapulohumeral rhythm, and the angle of humeral external rotation) or in activities of the rotator cuff muscles during flexion and reaching elevation, clinicians and researchers could obtain more useful results from the evaluation and study of reaching elevation. No studies have compared the kinematic elements and electromyographic (EMG) activities of the rotator muscles during flexion and reaching elevation. In the present study, we hypothesized that the above-mentioned elements and muscle activities would be significantly different between flexion and reaching elevation. This study aimed to compare these parameters during the two different arm-lifting conditions.
2. MATERIALS AND METHODS
2.1. Participants
The study was approved by the institutional review board of the Koriyama Institute of Health Science, Fukushima (No. R015-06). Total 13 volunteers without a history of shoulder pain and injury, who did not use to participate in throwing sports, were included in this study after obtaining written informed consent from them. Before the experiment, the senior author examined muscle atrophy, scoliosis, scapula dyskinesia, range of motion, impingement, and instability tests and performed radiographic investigation of the bilateral shoulders of the 13 subjects. Among them, the 3 subjects who revealed scapula dyskinesia during elevation, restriction of abduction, or positive instability test were excluded. Ten participants who showed no abnormality in these tests and had normal radiographic findings were included. The average height, weight, and body mass index of 10 participants (10 men, average age 21.5 ± 3.4 years) were 1.72 ± 0.43 m, 65.8 ± 7.1 kg, and 21.6 ± 3.3. Furthermore, the right side was the dominant side in all the participants. The kinematic parameters and EMG activities were measured on their dominant arms.
2.2. Instrumentation of Three-Dimensional Motion Analysis
Computerized three-dimensional (3-D) motion analyzer (MAC 3D System., Motion Analysis Corp., Santa Rosa, CA, USA) was used to measure the angles of glenohumeral joint elevation, scapular upward rotation, scapulohumeral rhythm, external rotation of the humerus, and the angle of glenohumeral plane shifting from the coronal plane of the thorax in 15° increments from the starting position to maximum elevation. The system allowed to capture 200-Hz data from 10 synchronized infrared cameras placed around the participants and also allowed the capture of data at 50-Hz. We investigated the reproducibility of the system for the angle of arm elevation, scapulohumeral rhythm, and external rotation of the humerus was confirmed in three participants on different days before the experiment. Potential experimental error owing to skin slippage was estimated by measuring the distances between the bony landmarks and marker locations with skin palpation and radiographs of all the participants recorded at the starting position, 60°, 90°, 120°, and 150° of elevation. The distance between each marker, that is, on the acromial angle, the root of the scapular spine, anterior and posterior of the humeral head, the lateral and medial epicondyles, and the thoracic spine, and each marker’s level to the spine was measured using the radiographs to detect the appropriate position of the markers with the smallest amount of skin slippage [18]. Motion data were analyzed using KineAnalyzer system software (Kissei Comtec Co, Nagano, Japan).
2.3. EMG of the Rotator Cuff Muscles
EMG activities in the rotator cuff muscles (supraspinatus, infraspinatus, subscapularis, and teres minor) were recorded during synchronized 3-D motion analysis during flexion and reaching elevation. Intramuscular fine-wires were prepared using the method reported previously [20]. First, 2 sterile 50 µm-diameter wires coated with Teflon (Dupont, Wilmington, DE, USA) were inserted into the rotator cuff muscles’ belly with a 25-gage hypodermic needle. Ultrasonography (ALOKA, Hitachi Medical Co. Chiba, Japan) was used for insertion of the intramuscular fine-wire into the teres minor, supraspinatus, and infraspinatus except for the subscapularis [21]. After identifying the posterior border of the clavicle, the medial margin of the acromion, and the scapular spine, the electrode was inserted into the supraspinatus close to the scapular spine through the upper trapezius. The needle was contacted with the scapula and then withdrawn 3 mm. The fine-wires were inserted into the middle of the infraspinatus using the same procedure used for the supraspinatus. The subscapularis was approached from the medial border of the scapula. The subjects were made to take the lateral decubitus position, the medial border of the scapula was lifted, and a 25-gage hypodermic needle was inserted at the midpoint between the inferior angle and the scapular spine to reach the subscapular fossa. The fine-wire was inserted into the lower part of the subscapularis. Before the recorded measurement session, all the participants randomly flexed, abducted, and rotated their dominant arms internally and externally to confirm that the wires were appropriately inserted in the muscles.
Raw EMG signals were recorded with the EMG system EMG-100C (BIOPAC Systems Inc., CA, USA), synchronized with the 3-D motion analysis system. All the EMG data were band-pass filtered at 10–3000 HZ, sampled at 1000 Hz, full-wave rectified, smoothed (100 ms root mean square), and analyzed with the Bimutus 2 analysis software (Kissei Comtec Co, Nagano, Japan) [22]. EMG was recorded in two ways: with maximal voluntary isometric contraction (MVIC) at 90° of flexion of the shoulder joint and at 90° of reaching elevation with 60° flexion of the elbow joint during three 5-seconds, and the average of the three trails per one second was taken as EMGmax that was used as a reference value for EMG amplitude normalization. EMG data for each 15° increment of integrated EMG (IEMG) of all muscles were obtained and the %IEMG for each 15° increment for 1 second was calculated based on the average figures for each second for each 100% MVIC for all the participants. The %IEMG of each muscle for each 15° increment was compared between flexion and reaching elevation.
2.4. Procedures
The participants stood with their thoracic spine, both arms, pelvis, and knees exposed. Reflective markers were placed on the acromial angle, the root of the scapular spine, the anterior and posterior of the humeral head, the lateral and medial epicondyles of the humerus, the styloid process of the radius, distal ulna, the spinous processes of the 7th cervical spine, 7th thoracic spine, and 5th lumber spine, the top and the xyphoid process of the sternum, and bilateral anterosuperior and posterosuperior spines of the pelvis. Before measurements, the participants were made to undergo several practice trials to ensure that they could complete the task in 5 seconds. All the participants performed flexion and reaching elevation to aim for a set object with the hand three times. Movement of reaching elevation started the position of the arm at the side (Fig. 1a), flexed the elbow joint (Fig. 1b), flexed the shoulder joint with flexion of the elbow joint (Fig. 1c), and reached maximum elevation (Fig. 1d).
The axis of the humerus was designated as the line connecting the midpoint of the anterior and posterior makers of the humeral head with the midpoint of the lateral and medial epicondyles. The line drawn between the root of the scapular spine and the acromial angle was defined as the line of the scapular spine. All the motions started from the neutral zero starting position and the starting angles of the dominant arm and scapular spine were set at 0° [10]. During the recording of the angles of glenohumeral elevation, humerothoracic elevation, scapular upward rotation, and external rotation of the humerus were simultaneously determined for each 15° increment from 0° to 150° of humerothoracic elevation. Each angle was automatically corrected from the numeric value of the 3-D leaning of the thoracic spine. The angles of glenohumeral elevation were divided by those of scapular upward rotation to calculate the scapulohumeral rhythm. The angle of humeral external rotation was measured as the rotation angle of the triangular plane, composed of the lateral and medial epicondyles, and the midpoint of the humeral head.
2.5. Data Analyses
The repeatability of the trials during the tasks performed with 2 types of arm lifting, scapular upward rotation, scapulohumeral rhythm, and the angle of external humeral rotation during flexion and reaching elevation was calculated using intraclass correlation coefficients (ICC [1, 1] and ICC [1, 3]). The Shapiro-Wilk test was conducted to determine whether the data followed a normal distribution pattern. Normally distributed data were analyzed with repeated-measures analysis of variance, and multiple comparisons (Tukey’s range test) were adjusted for multiplicity using a simulation-based method, yielding corrected p-values and 95% confidence intervals. The Wilcoxson signed-rank test was used to evaluate the data that were not disturbed normally. Parametric or non-parametric statistical analyses were applied for comparison with respect to the angles of glenohumeral elevation, scapular upward rotation, scapulohumeral rhythm, external humeral rotation, and %IEMG of each muscle for each 15° increment between flexion and reaching elevation. All the data are presented as mean ± standard deviation (range) values. All statistical analyses were performed using IBM SPSS Statistics 22.0 J software (IBM Japan, Tokyo, Japan) and statistical significance was defined as P < 0.05.
3. RESULTS
3.1. Repeatability and Parametric or Non-Parametric Analysis
System measurement error showed that the static accurate length measurements were < 0.05 mm, dynamic measurements were < 0.28 mm, static accurate angular measurements were < 0.09°, and dynamic accuracy was < 0.47°. The error due to skin slippage of the markers was 1.4 ± 1.0 cm for the root of the scapular spine, 0.7 ± 0.6 cm for the acromial angle, 1.2 ± 0.9 cm for the anterior maker of the humeral head, and 1.0 ± 0.6 cm for the posterior maker as measured using radiography. Further, the marker of both the epicondyles ranged within 0.5 cm with surface palpation. The ICCs [1, 1] for the angles of humerothoracic elevation, scapulothoracic upward rotation, scapulohumeral rhythm, and external rotation of the humeral head during flexion were in the range of 0.99‒1.0, 0.98‒0.99, 0.44‒0.96, and 0.99‒1.0, respectively. The ICCs [1, 3] for the angles of glenohumeral elevation, scapular upward rotation, scapulohumeral rhythm, and external rotation of the humerus during reaching elevation were in the range of 0.97‒ 1.0, 0.96‒1.0, 0.56‒0.99, and 0.80‒0.99, respectively. The angles except the scapulohumeral rhythm were categorized as almost perfect [23]. The EMG reliability of each muscle did not show significant differences (P = 0.19‒0.86).

The Shapiro-Wilk test revealed that the angles of glenohumeral elevation (P = 0.22‒0.87), scapular upward rotation (p = 0.28‒0.78), and external rotation of the humerus (P = 0.23‒0.88) for each 15° increment during flexion were parametric. Although the result of reaching elevation was similar to those obtained for flexion, the scapulohumeral rhythm (P = 0.00-0.01 and 0.00-0.05, respectively) and %IEMG of each muscle during flexion and reaching elevation were non-parametric.
3.2. Glenohumeral Angle, Scapular Upward Rotation Angle and Scapulohumeral Rhythm
The glenohumeral and scapular angles during both types of arm lifting are shown in Fig. (2). The average angle of maximum elevation at the glenohumeral joint was 112° ± 7° for flexion and 106° ± 4° for reaching elevation. The angles of the glenohumeral joint in each 15° increment did not show a significant difference between flexion and reaching elevation throughout the 150° range of humerothoracic elevation (P = 0.07‒.56).
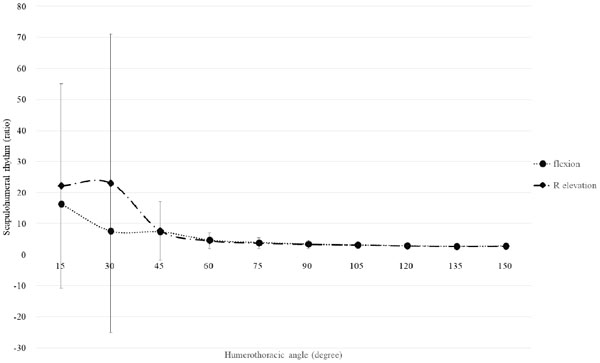
The maximum angle of scapular upward rotation was 39° ± 6°during flexion and 40° ± 3° during reaching elevation (Fig. 2). The angle of scapular upward rotation during flexion and reaching elevation did not show a significant difference in each 15°increment (P = 0.09 ‒ 0.83). The scapulohumeral rhythm during flexion ranged from 2.8‒10.9 (average = 3.1 ± 2.7), and varied from 2.4‒6.1 (average = 3.0 ± 1.1) during reaching elevation (Fig. 3). There was no statistically significant difference in the scapulohumeral rhythm between both types of arm lifting (P = 0.22‒0.88).
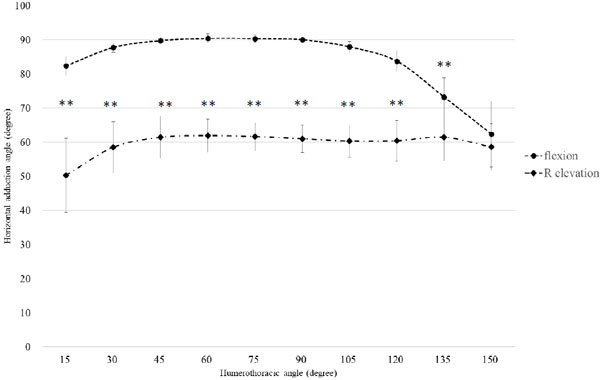
3.3. Plane of Flexion and Reaching Elevation and Angles of the Elbow Joint
The horizontal adduction angle of the flexion plane started from 83°, remained at 90°, and declined to 62° at maximum elevation. The angle of reaching elevation initiated at 50° and it retained at 60° until maximum elevation (Fig. 4). Moreover, horizontal adduction angles between flexion and reaching elevation showed statistically significant differences, except for maximum elevation (P = 0.001‒0.034). The average angle of the elbow joint during flexion was almost constant (7° ± 3°). However, the angle during reaching elevation changed as follows: 73° at 15° of elevation, that increased up to 104° at 60° of elevation, and gradually decreased to 5° at maximum elevation.
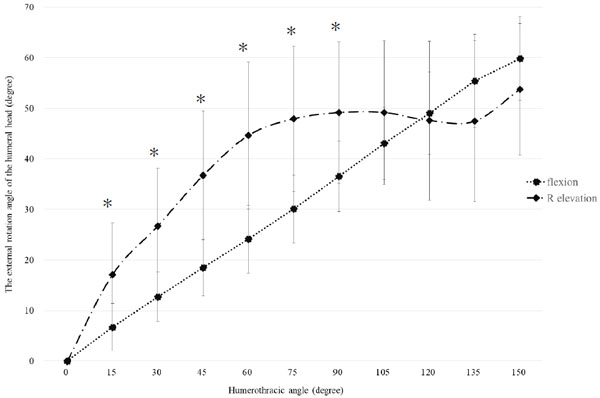
3.4. The Angle of Humeral External Rotation
The external rotation angles of the humerus were not similar between flexion and reaching elevation; the angles showed a linear increase during flexion and a curved increase during reaching elevation (Fig. 5). The maximum external rotation angles were 54° ± 13° for flexion and 60° ± 8° for reaching elevation, and statistically significant differences between flexion and reaching elevation were identified from 15° to 90° of the humerothoracic angle.
3.5. EMG Activities of the Rotator Cuff Muscles
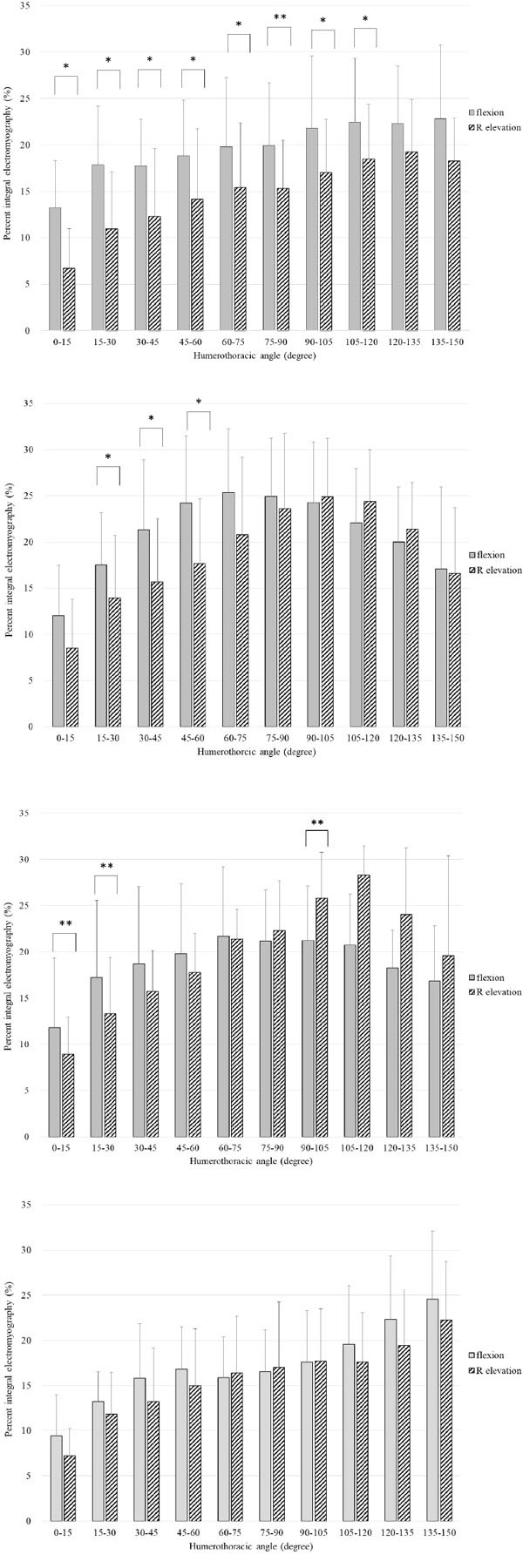
The %IEMGs of the rotator cuff muscles from 0° to 150° are shown in Figs. (6a-d). Higher activities that were statistically significant were noted between 15° and 45° for the supraspinatus and between 15° and 75° for the infraspinatus during flexion. However, there was no significant difference in %IEMG of the subscapularis between flexion and reaching elevation. In all the rotator cuff muscles, the %IEMGs during reaching elevation were lower than those during flexion below 60° of humerothoracic elevation.
4. DISCUSSION
The most important finding of the present study is that flexion and reaching elevation are distinct motions, as demonstrated by the different glenohumeral planes despite similar starting and terminal positions of the hands. The glenohumeral plane in flexion was not completely consistent with the sagittal plane to the thorax, close to the glenohumeral plane of reaching elevation, especially at 150° of elevation. The glenohumeral plane of reaching elevation was 30° posterior to the sagittal plane of the thorax except for the initial 30° of elevation. In general, 3 planes of flexion, scaption, and abduction have been analyzed in many biomechanical studies. Reaching elevation is postulated as the fourth plane, and the plane is believed to be an ordinary and inherent movement by humans. The participants were students of the college of physical therapy; therefore, they could accurately understand the motions of flexion and reaching elevation, and their accuracy of movements could be more than those of ordinary people. They were conscious only of the position of their hands while performing the tasks; however, they did not realize the positions and motions of the elbow joint, glenohumeral joint, and scapula. Thus, we can only control the motion of the hand; however, the motions of the elbow, shoulder, and scapulothoracic joints are unconsciously controlled to follow the positions of the hands. The distinct elbow motions of flexion and reaching elevation are associated with different glenohumeral planes during the 2 types of arm lifting.
The second important finding was the presence of statistically significant differences in the external rotation angles of the humerus below 90° of humerothoracic elevation between the 2 types of arm lifting. The external rotation of the humerus is an essential motion of flexion, scaption, and abduction to avoid impingement between the greater tuberosity and the acromion. Previous in vitro studies have reported approximately 25°-55° of external rotation during these arm liftings [3, 24-28]. In addition, it has been clarified that the increasing patterns of external rotation angle varied among flexion, scaption, and abduction [3, 28]. The linear increase in the external rotation angle during flexion observed in the present study is consistent with a recent report [3]; however, to our knowledge, there has been no investigation of the external rotation of the humerus during reaching elevation. The curved increase in the angle during reaching elevation is similar to that during abduction [3, 28]. With the shifting of the plane of abduction toward the posterior side from that of flexion, external rotation of the humerus transforms from the linear to curved increment [3]. It is plausible that the external humeral rotation of reaching elevation exhibits a curved increment because the glenohumeral plane is 30° posterior to the sagittal plane of the thorax. In addition, the rotator cuff muscles, such as the infraspinatus and teres minor, that generate the force of external rotation of the humerus, engage in the initial phase of elevation. Loss of external rotation of the humerus. suggests rotator cuff tears or contracture of the shoulder joint, such as massive rotator cuff tears or thickness of the anterior capsule and inferior glenohumeral ligament. [29, 30]. Therefore, the evaluation of humeral external rotation is crucial in clinical practice.
Scapulohumeral rhythm is an essential parameter for determining normal and abnormal shoulder motion with rotator cuff tears or stiff shoulder [1, 4]. Recent studies have documented that the ratios of the scapulohumeral rhythms in normal shoulders are in the range of 2.0 - 2.4 for flexion, 1.8 - 3.4 for scaption, and 1.9 - 3.0 for abduction, except in the setting phase [3, 7, 8, 10]. The present study showed that the average scapulohumeral rhythm was 3.0 for flexion and 3.1 for reaching elevation; these findings are not completely consistent with those in the previous reports. This may be due to many factors, including skin slippage of the markers, differences in instrumentations, planes of analysis, measuring range, trunk positions, and participant characteristics. The angles of glenohumeral elevation, scapular upward rotation, and scapulohumeral rhythm were not significantly different between flexion and reaching elevation. It was noteworthy that the different planes in the 2 types of arm lifting did not influence the 3 kinetic factors; therefore, the principle of scapulohumeral rhythm was applicable to evaluate the movement of the shoulder complex.
The third important finding was that all rotator cuff muscles were engaged throughout arm lifting and that the EMG activities of the supraspinatus, infraspinatus, and teres minor during reaching elevation were significantly lower than those during flexion. In all the rotator cuff muscles, %IEMGs of flexion were higher than those for reaching elevation below 60°of humerothoracic elevation. The activities of all rotator cuff muscles are reportedly necessary for arm elevation; in particular, the supraspinatus engages prior to the start of abduction, and the infraspinatus, teres minor, and subscapularis generally exhibit synchronous firing to stabilize the glenohumeral joint [9]. Rotator cuff tears occur frequently in the supraspinatus and infraspinatus tendons; therefore, reaching elevation is presumed to be an invulnerable elevation for the rotator cuff rather than flexion. Considering the significant difference between the 2 patterns of arm lifting, the distance from the glenohumeral joint to the center of gravity of the upper extremity is shorter for reaching elevation than for flexion. The shorter moment arm owing to flexion of the elbow joint contributes to lower activities of the rotator cuff muscles during reaching elevation. The EMG activities of the anterior and middle deltoid during flexion were significantly higher than those during reaching elevation (data did not show). Many researchers have indicated that the deltoid is the prime mover and the supraspinatus is the initiator [6, 17, 19] and that an essentially equal torque from the deltoid, supraspinatus, and infraspinatus complex contributes to flexion and scaption [16, 31]. Longer lever arm during flexion, rather than during reaching elevation, produces a higher magnitude of muscle firing, as observed in the present study.
It is noteworthy that the pattern of EMG activities, especially for the supraspinatus during flexion in the present study, is not consistent with most previous reports, wherein the EMG activities increased up to 90° and then gradually declined to maximum elevation [6, 14-17, 19]. However, Ito et al. [13], demonstrated a similar pattern of EMG activities for flexion as found in the present study. These differences may be attributed to the measurement conditions, such as various glenohumeral planes (flexion, scaption, and abduction), static or dynamic motion, unloaded or loaded motion, and locations of the inserted electrodes that were close to the scapular spine to avoid an injury of the suprascapular nerve. The patterns of EMG activities of the infraspinatus, teres minor, and subscapularis observed in the present study conversely coincide with those reported in the previous studies [6, 14-17, 19]. The EMG activities of the lower subscapularis that distinctively occur during shoulder flexion, abduction, and external rotation of the humerus, reflect increasing EMG activities throughout arm lifting to depress and stabilize the humeral head to the glenoid cavity [10].

Upper limb motion generally starts by drawing the hand toward the body and then extending the arm and hand toward the target. In the present study, reaching elevation, an important movement performed in daily living, is an efficient and invulnerable motion for shoulder muscles. Flexion, scaption, and abduction, maintaining extension of the elbow joint, are examined to evaluate shoulder function; however, they are not movements performed in daily living. The first clinical implication of this study is that reaching elevation can be easily examined in patients with shoulder disorders. The second is that reaching elevation is an appropriate rehabilitation program after rotator cuff repair because the movement engages less force in the rotator cuff muscles.
The present study has certain limitations. The first limitation is that the error of skin slippage cannot be completely excluded from the kinetic measurements. Recent studied have shown that surface sensors are an accurate way of measuring humeral external rotation and elevation plane [31, 32]. However, skin error in the transverse plane during arm lifting, but not during angular rotation, can be radiographically examined. A comparative study of dynamic magnetic resonance imaging, electromagnetic tracking device, and 3-D motion analysis with skin makers is necessary to detect the skin error. Secondly, the sample size of this study was relatively small, and the investigation was limited to sagittal plane elevation in the dominant arms. Third, to our knowledge, no previous studies have investigated reaching elevation; therefore, we could not compare the current results with previous reports. Finally, the wire electrodes in the rotator cuff muscles can be considered a limitation of this study, that is, the EMG activities determining in the muscles only reveal a small part of the activities occurring in the muscles.
CONCLUSION
This study investigated the biomechanical elements during flexion and reaching elevation using 3-D motion analysis with skin makers. Kinematic differences between both arm-lifting conditions were identified in the glenohumeral plane, pattern of humeral external rotation, and EMG activities of the rotator cuff muscles. Reaching elevation, an invulnerable motion of arm lifting is useful for evaluating the shoulder function and for physical therapy in patients with shoulder disorders.
ETHICS APPROVAL AND CONTENT TO PARTICIPATE
The study was approved by the Institutional Review Board of the Koriyama Institute of Health Science, Fukushima (No. R015-06).
HUMAN AND ANIMAL RIGHTS
No animals were used in this study. All human research procedures followed were performed in accordance with the ethical standards of the institutional and /or national research committee and with the Helsinki declaration.
CONSENT FOR PUBLICATION
Written informed consent was obtained from all participants.
AVAILIBILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTERST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


