All published articles of this journal are available on ScienceDirect.
Osteonecrosis of the Femoral Medial Condyle Due to Leg Length Discrepancy After A Traffic Accident
Abstract
Untreated leg length discrepancy can cause spontaneous osteonecrosis of the knee, which is associated with subchondral insufficiency fractures of the knee and progression or onset of osteoarthritis of the knee. Spontaneous osteonecrosis of the knee can be secondary to cartilage loss or additional subchondral changes. A 40-year-old female underwent opening-wedge high tibial osteotomy and osteochondral grafting for osteonecrosis of the femoral medial condyle and osteoarthritis of the knee caused by leg length discrepancy after a traffic accident. High tibial osteotomy and cartilage restoration are often considered for the treatment of knee osteonecrosis with cartilage damage in younger patients.
1. INTRODUCTION
Risk factors for osteoarthritis (OA) can be divided into person-level factors, such as age, sex, obesity, genetics, and race/ethnicity, and joint-level factors, including injury, malalignment, and abnormal loading of the joints [1, 2]. OA in relatively young patients is often due to secondary OA, which is a result of previous trauma. Spontaneous osteonecrosis of the knee is associated with subchondral insufficiency fractures of the knee and progression or onset of OA of the knee [3]. Patients who have osteonecrosis of the knee may be managed operatively or non-operatively based on symptoms and disease staging. Surgical treatment options include total knee arthroplasty (TKA), unicompartmental knee arthroplasty, and high tibial osteotomy (HTO). Regarding HTO, Harris reported that combined HTO and an arthroscopic procedure was better than isolated HTO for survival [4]. Kahlenberg reviewed previous studies suggesting the benefits of HTO with cartilage restoration [5]. We present a case of opening-wedge HTO and osteochondral grafting for osteonecrosis of the femoral medial condyle and OA of the knee caused by leg length discrepancy after a traffic accident.
2. CASE
A 40-year-old female presented with progressive left knee pain and gait disturbance. The patient had had a bilateral femoral fracture and left ankle fracture in a car accident, and undergone femoral osteosynthesis with intramedullary nails 16 years previously. After the treatment, she had had no symptoms in her left knee, but developed progressive pain in the left knee five years previously. She was diagnosed with OA and started receiving hyaluronic acid injections, but the treatment was ineffective and her left knee pain worsened. Therefore, she was referred to our department for surgery. Her past history and family history were unremarkable. Physical examination revealed swelling, effusion and medial joint line tenderness in the left knee. The range of motion was between 5° and 130°. McMurray tests for medial meniscus were positive. The knee-rating scale of the Hospital for Special Surgery (HSS) was 75. The Rosenberg view showed Kellgren-Lawrence OA grade 2. Weight-bearing long leg plain film radiography demonstrated a left-sided discrepancy of 10 mm and the anatomical lateral distal femoro-tibial angle (FTA) was 180° (Fig. 1). Magnetic resonance imaging (MRI) revealed degeneration of the medial meniscus, joint effusion, edematous area in the bone marrow of the left medial femoral condyle, and articular cartilage defect in the femoral medial cartilage (Fig. 2A and B).

B. Weight-bearing long leg plain film radiography demonstrated a left-sided discrepancy of 10 mm and the anatomical lateral distal femoro-tibial angle (FTA) was 180°.
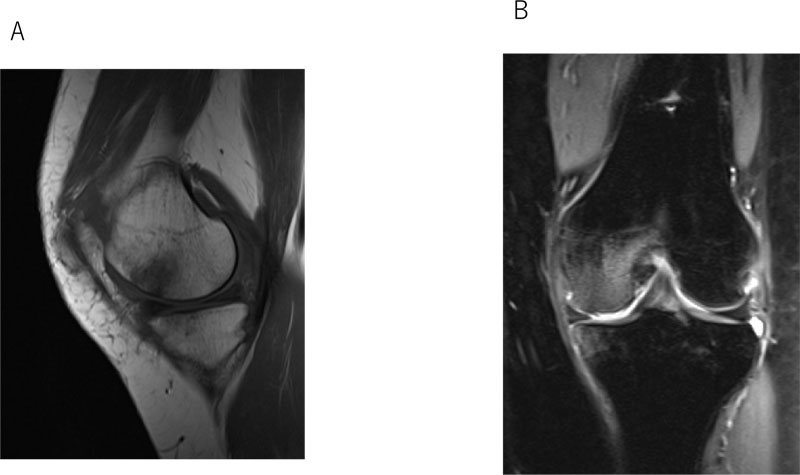
A. T1-weighted image, sagittal view.
B. T2-weighted, fat suppression image, coronal view.
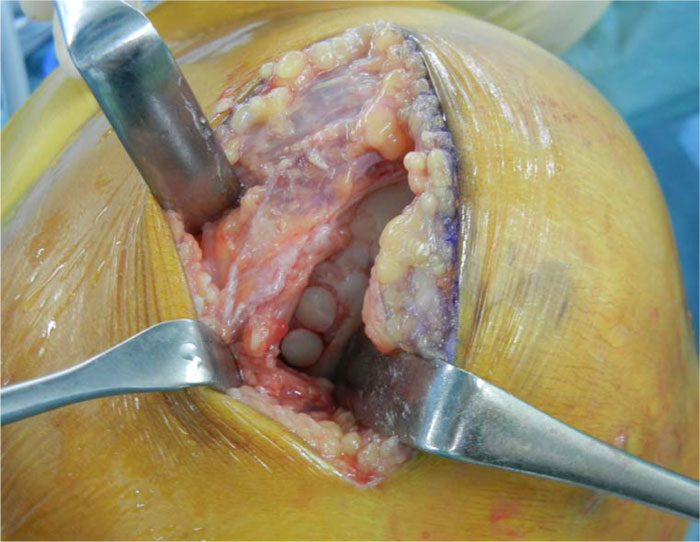
We diagnosed her with osteonecrosis of the femoral medial condyle and osteoarthritis of the knee. We considered autologous chondrocyte implantation (ACI) and HTO as surgical treatment. After the intradermal allergy test against atelocollagen, arthroscopic assessment and harvesting of autologous cartilage were performed. However, the allergy test varied from negative to positive after two weeks and ACI was discontinued. Opening-wedge HTO and osteochondral grafting were then performed. We harvested two 6.5-mm osteochondral plugs from the medial superior condyle of the left femur and the superior lateral condyle of the right femur, and transplanted the plugs into the lesion (Fig. 3). Opening-wedge HTO was performed using TomoFix Japanese and synthetic bone substitute (Fig. 4A and B).
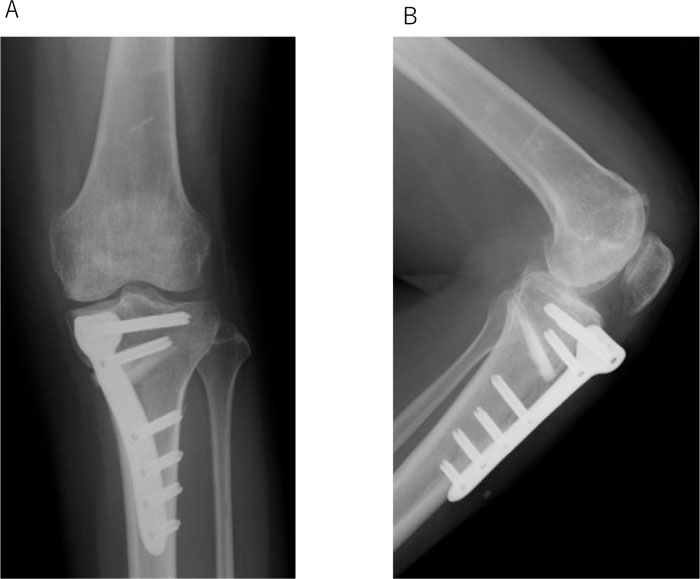
A. A-P view.
B. Lateral view.
A knee brace was put on the right leg for 1 week. Range of motion (ROM) exercise was started 1 week after the surgery. The patient was kept from weight bearing for 4 weeks. Full weight bearing was allowed at 6 weeks.
One and a half years after the surgery, she had almost no symptoms in her left knee. The ROM was from 0° to 145° and the HSS score was 98.
3. DISCUSSION
Bone marrow lesions (BML) around the knee are present in traumatic contusion and fractures, osteoarthritis, spontaneous insufficiency fractures and osteonecrosis. Since Ahlback reported osteonecrosis of the knee, it has been classified into three categories: spontaneous osteonecrosis of the knee, avascular necrosis and post-arthroscopic osteonecrosis [6]. Post-arthroscopic osteonecrosis may develop after meniscectomy, cartilage debridement, or radiofrequency surgery. Avascular necrosis can be secondary to corticosteroid use, radiation, alcohol abuse, systemic diseases, or chemotherapy. This patient had no history of trauma in her left knee or risk factors for osteonecrosis. She exhibited pain in the medial compartment without a history of trauma to her knee or risk factors. Leg length discrepancy is very common, occurring in up to 70% of the population [7]. Few studies have looked directly at the association between leg length discrepancy and knee osteoarthritis [8, 9]. Harvey reported that leg length discrepancy of more than 10 mm was associated with prevalent, incident symptomatic and progressive knee osteoarthritis [10]. Therefore, we thought leg length discrepancy might be associated with the progression or onset of OA of the knee and subchondral insufficiency fractures of the knee. Spontaneous osteonecrosis of the knee has been associated with subchondral insufficiency fractures of the knee. Marcacci reported that the clinical course and earliest stage of spontaneous osteonecrosis of the knee can be unpredictable, and do not necessarily progress in all patients. In the acute stage, there is a marked, ill-defined, edema-like signal that is more extensive than the pattern secondary to cartilage loss. The lack of additional changes other than BML is 100% predictive of reversibility. The presence of a subchondral area of low signal at >4-mm thick strongly predicts irreversibility [3]. As there was a lack of additional subchondral changes other than BML without an articular cartilage defect in the femoral medial cartilage in this case, we performed HTO in combination with cartilage surgery.
Several studies found that HTO in isolation may delay the progression of knee recovery. However, cartilage regeneration is typically only scattered and offers partial coverage [11-13]. The benefits of an additional arthroscopic procedure during HTO remain unclear [8-10]. Cartilage restoration in combination with HTO has been associated with improved cartilage formation in advanced OA [14-16]. Harris reported that a combined HTO and arthroscopic procedure is better than isolated HTO for survival. However, there are numerous differences in surgical techniques, follow-up periods, inclusion criteria and severity of medial compartment osteoarthritis among studies [3]. Kahlenberg found that HTO with cartilage restoration procedures provides a reliable improvement in functional status in the medium- to long-term period after surgery and has the potential to delay or prevent the need for knee arthroplasty surgery [5]. As TKA after HTO may be technically more challenging, its results may be inferior to those of the primary TKA.
Concerning cartilage restoration, in this case, we performed osteochondral grafting because the allergy test for ACI was positive. Osteochondral grafting can lead to articular cartilage repair to a certain degree. In the short-, medium-, and long-term periods, osteochondral grafting results in a better clinical outcome than the microfracture method for articular cartilage defects of the distal femur of the knee [17, 18]. ACI is the only effective treatment that enables chondral restoration for severe chondral defects. One advantage is that restoration is feasible using hyaline cartilage-like tissue, which is similar to articular cartilage [19, 20].
CONCLUSION
Leg length discrepancy can cause spontaneous osteonecrosis of the knee, which is associated with subchondral insufficiency fractures of the knee and the progression or onset of OA of the knee. HTO in combination with cartilage surgery, may be a well-tolerated, safe and effective treatment for advanced medial compartment OA. This may be a suitable option for relatively young patients for whom other surgical interventions, including TKA, are not indicated.
LIST OF ABBREVIATIONS
| OA | = Osteoarthritis |
| TKA | = Total Knee Arthroplasty, |
| HTO | = High Tibial Osteotomy |
| HSS | = Knee-rating Scale of Hospital for Special Surgery |
| FTA | = Femoro-Tibial Angle |
| MRI | = Magnetic Resonance Imaging |
| ACI | = Autologous Chondrocyte Implantation |
| BML | = Bone Marrow Lesions |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
We have obtained consent to publish from the patient.
STANDARD OF REPORTING
CARE guideline and methodology were followed.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


