All published articles of this journal are available on ScienceDirect.
Migration of a Meniscal Repair Implant Mimicking Meniscal Injury
Abstract
Complications after arthroscopic meniscal suture repair have been reported. Migration of a meniscal repair implant mimicking meniscal injury is rare. A 28-year-old female had undergone Anterior Cruciate Ligament (ACL) reconstruction at another hospital 12 years ago . The remaining instability after ACL reconstruction resulted in medial meniscal damage, wear and narrowing in the posterior third. The H-fix that was used in the meniscal repair became detached, exposing the inside of the knee joint. Meniscal repair is a successful procedure in conjunction with ACL reconstruction. However, when knee instability after ACL reconstruction remains, the choice of meniscal repair implants may lead to potential complications even after long-term clinical follow-up.
1. INTRODUCTION AND BACKGROUND
Meniscal repair is performed to prevent meniscal dysfunction and post-traumatic osteoarthritis. However, complications of meniscal suture repair, such as deep infection, repair failure, neurovascular injuries, arthrofibrosis and chondral injury, have been reported [1-5]. Migration of meniscal repair implants has also been reported. However, disturbance due to the migration of a meniscal repair implant mimicking meniscal injury is rare. We present a case of migration of one meniscal repair implant (H-fix, Mitek) 12 years postoperatively.
2. CASE
A 28-year-old female presented with left knee pain, crepitation, gait disturbance and a “giving way” sensation. She had undergone anterior cruciate ligament (ACL) reconstruction at another hospital 12 years back. After the surgery, she had occasional pain, but no giving way or locking sensation in her knee. Her history after the surgery was unremarkable.
Physical examination revealed swelling, effusion and medial joint line tenderness in the left knee. The range of motion was between 10° and 120°. McMurray tests for medial meniscus were positive. The results of posterior drawer tests, and varus and valgus stress tests were normal, but the Lachman test and anterior drawer test were positive. The patient had no patellofemoral symptoms. Magnetic resonance imaging (MRI) demonstrated a reconstructed ACL, medial meniscus tear, and effusion in the suprapatellar pouch (Figs. 1A, 1B).
Arthroscopy revealed a reconstructed ACL, the medial meniscus that was worn and narrowed in the posterior third and one meniscal suture implant (H-fix), which had been used to repair the medial meniscus (Figs. 2A, 2B). The chondral lesion of the femoral medial condyle and the tibial medial plateau were found at the weight-bearing portion. The implant was resected with a punch.
The knee symptoms disappeared immediately after surgery and the patient was able to resume daily activities in a half-year. The Lysholm knee score was 85.
3. DISCUSSION
Nonabsorbable sutures, meniscus arrows or staples and bioabsorbable implants are often used to repair meniscal tears. Good-to-excellent results can be expected from meniscal repair [6, 7]. On the other hand, reported complications after meniscal repair using the inside-out technique include infection, arthrofibrosis, nerve injury, vascular injury and chondral injury [1-5].
In the present case, the patient remembered that she had undergone ACL reconstruction at another hospital 12 years back, but not that meniscal repair had been performed. There was no incision scar from meniscal repair. Before surgery, we diagnosed her with medial meniscal injury associated with the failure of anterior cruciate reconstruction. The all-inside technique for meniscal repair has the advantage of not affecting structures around the knee joint. Complications after using biodegradable meniscus arrows have been reported [8-10], and subcutaneous migration of meniscal arrows has been well documented. Chondral injury due to migration inside the knee joint is also a serious complication. Serious complications are mostly observed after unhealed repair of the meniscus [11, 12].
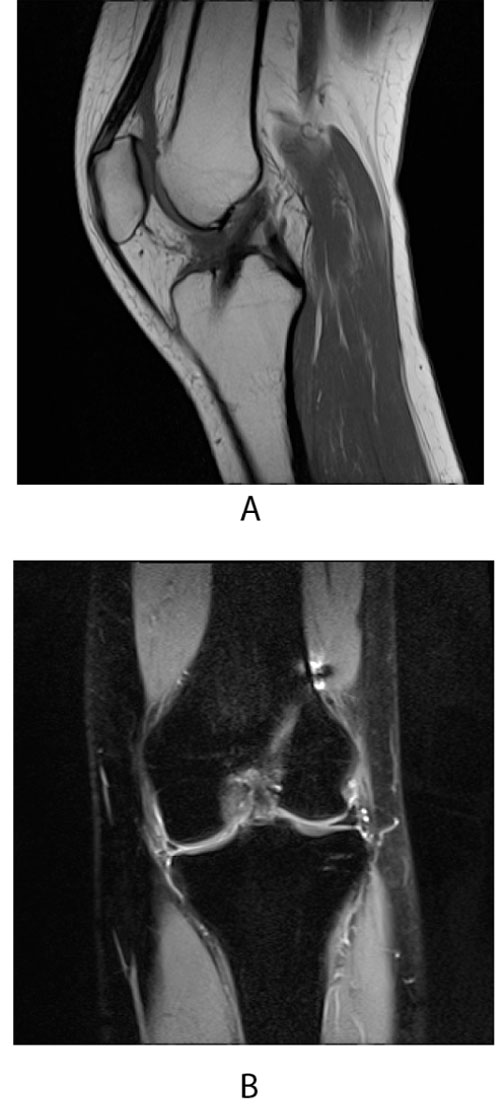
A Sagittal T1-weighted image reconstructed anterior cruciate ligament.
B Coronal T2-weighted image medial meniscal tear.
Long-term outcomes after meniscal repair in patients undergoing concurrent ACL reconstruction are limited to small single-center series, with failure rates ranging from 0-29% at a minimum 5-year follow-up [13-15]. A systematic review calculated the failure rate of meniscal repair in ACL-reconstructed knees to be 26.9% at 5 years [16]. A few studies suggested that ACL reconstruction produces protective effects for meniscal repair [17-19]. On the other hand, Nepple reported that the failure rate increased in combined ACL reconstruction and meniscal repair groups compared with meniscal repair in stable knees [16]. In the present case, the remaining instability after ACL reconstruction might result in medial meniscal damage and wear from the arthroscopic findings.
Thus, the following scenario should be considered: ACL reconstruction and medial meniscal repair were performed 12 years back . The remaining instability after ACL reconstruction resulted in medial meniscal damage, wear and narrowing in the posterior third. Then, the H-fix that was used in the meniscal repair became detached, leading to left knee pain and crepitation.
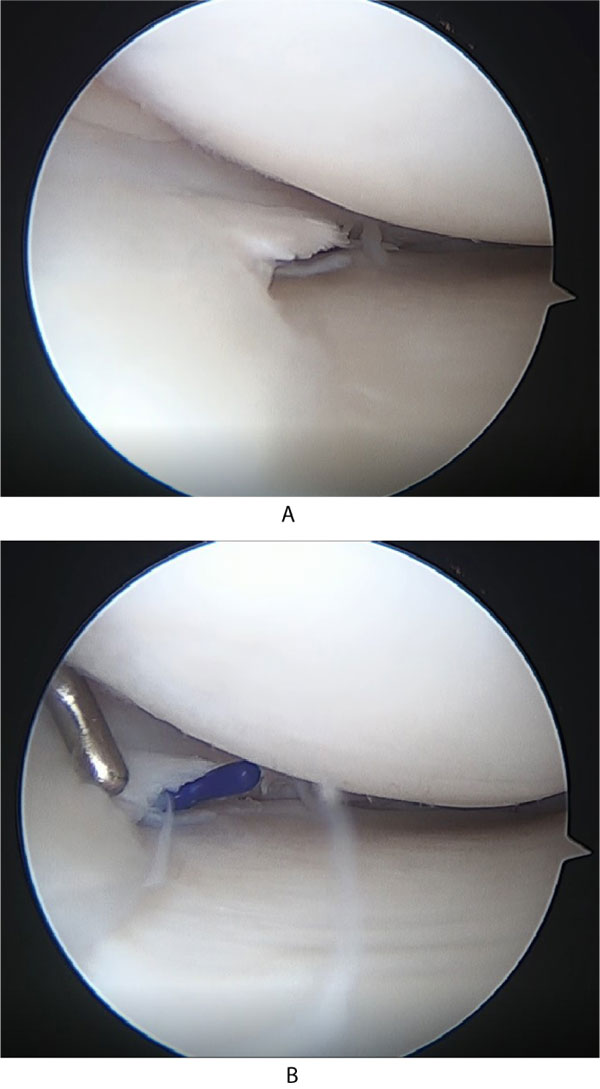
A Medial meniscus before probing.
B H-fix under the medial meniscus.
CONCLUSION
The all-inside meniscal repair technique is a reliable treatment option. The choice of meniscal repair implants may lead to potential complications even in long-term clinical follow-up after ACL reconstruction and combined meniscal repair.
LIST OF ABBREVIATIONS
| ACL | = Anterior Cruciate Ligament |
| MRI | = Magnetic Resonance Imaging |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
STANDARD OF REPORTING
PRISMA Guideline and methodology were followed.
CONSENT FOR PUBLICATION
We have obtained consent to publish from the patient.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


