All published articles of this journal are available on ScienceDirect.
Recovery of Range of Motion and Decrease in Pain after Progression of Supraspinatus Tendon Tear: A Case Report
Abstract
Rotator cuff disease is one of the most prevalent shoulder disabilities especially in the elderly population. Tear progression is significantly greater in the symptomatic patients than in the asymptomatic ones. From these aspects, shoulder surgeons interpret surgical indications and counsel patients regarding the risk of non-operative treatments. However, there were a few reports that pain and duration of symptoms were not strongly associated with severity of rotator cuff tears, and non-operative management with physical therapy was effective. There have remained controversies for the treatment of rotator cuff tears.
A 59-year-old man with a sedentary work life experienced right shoulder pain with abduction at night. However, the pain kept worsening after two months, and he finally visited our clinic three months after the onset of pain. Magnetic resonance imaging in the coronal and axial planes showed effusion around the subacromial and subcoracoid bursae and joint-side tear of the supraspinatus tendon. A range of motion in the right shoulder was severely restricted at the initial visit of our clinic. After sufficient rehabilitation, the symptoms were not changed and an arthroscopic rotator cuff repair was scheduled. However, during waiting for surgery, he felt something popped in the right shoulder while wearing a jacket. Immediately after this, pain during motion and at night decreased, and he experienced no difficulty with activities of daily living and the surgery was cancelled. This is the first case with a recovery of range of motion and a decrease in pain after progression of a supraspinatus tendon tear.
1. INTRODUCTION
Rotator cuff disease is very common in the elderly population and it is one of the most prevalent shoulder disabilities. Its prevalence varies widely with population characteristics; however, increasing age is associated with rotator cuff pathology [1, 2]. Because high-quality evidence is not available to help guide treatment of patients with rotator cuff pathologies [3], there remains considerable controversy among shoulder surgeons regarding optimal management of rotator cuff disease with significant variations [4]. Many orthopaedic surgeons would agree that rotator cuff disease is influenced by biologic factors and mechanical stress [5]; however, genetic factors are also strongly associated with its development [6-8], which could make it difficult for surgeons to come to a consensus on its management.
A longitudinal study for three years on 50 patients with asymptomatic rotor cuff tears revealed that 36% (18/50) developed symptoms, and tear progression was significantly greater in the symptomatic group than in the asymptomatic group [9]. Furthermore, the development of pain in patients with asymptomatic rotator cuff tears was associated with tear progression [10]. Tear enlargement occurred in more severe types and there was development of pain in a time-dependent manner [11]. Considering these aspects, shoulder surgeons interpret surgical indications and counsel patients regarding the risk of non-operative treatment [5]. However, the Multicenter Orthopaedic Outcomes Network Shoulder Group reported that pain and duration of symptoms were not strongly associated with severity of rotator cuff tears [12, 13] and that non-operative management with physical therapy was effective, with 75% of patients experiencing relief for up to two years [14]. Function and pain are not always associated with rotator cuff tears, and other approaches should be considered to provide better treatment to patients with shoulder problems.
This is the first case report regarding recovery of range of motion and decrease in pain after progression of a supraspinatus tendon tear.
2. REPORT OF THE CASE
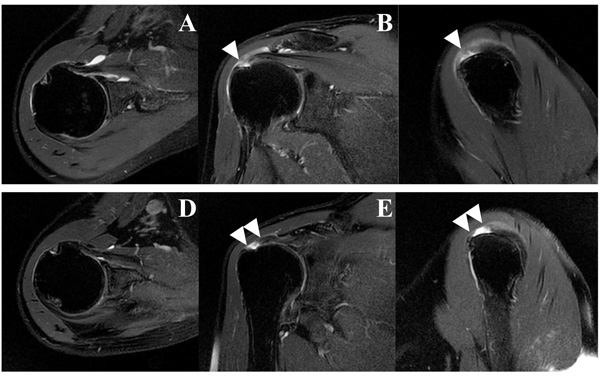
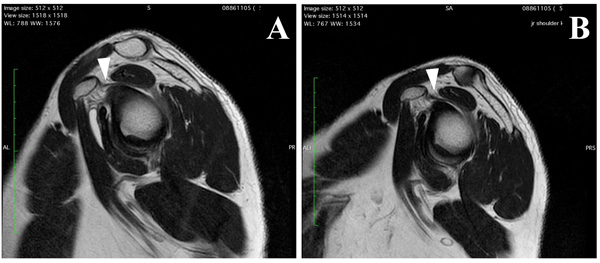
A 59-year-old man with a sedentary work life experienced right shoulder pain with abduction at night. He had no past history of systemic disease or symptoms. He visited a hospital complaining of difficulty in using the arm and in wearing trousers. He was prescribed non-steroidal anti-inflammatory drugs and was administered an injection of hyaluronic acid into the glenohumeral joint. However, the pain kept worsening after two months, and he finally visited our clinic three months after the onset of pain. X-ray films taken on his initial visit to our clinic appeared normal, but Magnetic Resonance Imaging (MRI, T2 weighted image) in the coronal and axial planes showed effusion around the subacromial and subcoracoid bursae and joint-side tear of the supraspinatus (SSP) tendon (Fig. 1A-C). However, a sagittal MRI (T1 weighted image) revealed no thickening of the coracohumeral ligament (CHL) and obliteration of the subcoracoid fat triangle (Fig. 2A). Range Of Motion (ROM) in the right shoulder was severely restricted on his initial visit to our clinic Table 1.
| - | Initial | Final | |
|---|---|---|---|
| - | Lt | Rt | Rt |
| FE | 180 | 90 | 170 |
| ABD | 180 | 90 | 165 |
| 1st ER | 60 | 45 | 65 |
| 2nd ER | 90 | 75 | 90 |
| 2nd IR | 20 | -20 | 0 |
| HBB | T5 | L2 | T11 |
| HF | 145 | 145 | 150 |
| 3rd ER | 90 | 90 | 90 |
| 3rd IR | 15 | 0 | 0 |
The American Shoulder and Elbow Surgeons (ASES) score was 60, the University of California at Los Angeles (UCLA) shoulder rating score was 18, and the Constant shoulder score was 68. Based on these findings, a preoperative diagnosis of joint-side tear of the SSP along with shoulder stiffness was made. Although physiotherapy, including stretching of the muscles around the shoulder girdle, thorax, spine, trunk, and hip joints, was undertaken for a total of 6 weeks at our clinic, there was no relief of pain or restoration of ROM. Therefore, an arthroscopic rotator cuff repair was scheduled. While wearing a jacket at two months after the initial visit, he felt something popped in the right shoulder. Immediately after this, pain during motion and at night decreased, and he experienced no difficulty with activities of daily living. Five days after the incident, he visited our clinic. The ROM significantly improved to almost full range (Table 1) and the ASES, UCLA, and Constant scores improved to 100, 35, and 96, respectively. MRI revealed enlargement of the supraspinatus tear and decrease of effusion (Fig. 1D-F) without thickening of the CHL as well as the other joint capsule (Fig. 2B). Because he had no difficulty with activities of daily living, surgery was ruled out and careful follow-up was continued.
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
3. DISCUSSION
Based on conventional theory, the articular aspect of the anterior supraspinatus adjacent to the biceps tendon is the common location for degenerative tears [15, 16], propagating posteriorly into the supraspinatus and infraspinatus tendons [5]. However, analysis via ultrasonography of full-thickness tears revealed that an approximately 13- to 17-mm area posterior to the biceps tendon was most frequently involved and the most anterior aspect of the supraspinatus was involved only 30% [17]. The 15-mm area posterior to the biceps tendon lies at the junction of the supraspinatus and infraspinatus tendons [18] and correlates with the middle of the “rotator crescent”, with the thinner and avascular tissues being compared with the “rotator cable” [19]. This area and the articular aspect of the supraspinatus in this case corresponded well with these anatomical findings.
Severely restricted ROM in all planes is a feature of frozen shoulder. A thickened CHL at the rotator cuff interval has been recognized to be one of the most specific manifestations of frozen shoulder and the primary restraint against external rotation [20]. Furthermore, thickening of other parts of the joint capsule, including the inferior glenohumeral ligament, also restricts ROM in frozen shoulder. However, in this case, there were no specific findings on MRI with regard to thickening of the CHL, as well as the other joint capsule, and restriction of ROM was mainly with forward flexion and abduction, accompanied by pain. Impending rupture of the supraspinatus tendon at the bursal side was one of the most probable causes for pain. Furthermore, the restriction of ROM is supposed to be due to adhesion in the subacromial space, usually around the coracoacromial ligament, which is close to the site of the tendon tear. Together with the tendon rupture and release of adhesion in this case, decrease in pain and recovery of ROM could occur simultaneously.
Postural abnormality is a strong predictor for rotator cuff tears and pain in the past, as opposed to pain currently being experienced, according to population-based studies [1]. Poor posture has been directly linked to a decrease in the subacromial space [21] and scapular kinematics [22] with increasing internal rotation of the shoulder [23, 24]. Postural correction is a very easy approach to recover ROM in the shoulder, but it failed in this case. Other mechanisms to alter the center of rotation of the glenohumeral joint should be considered. Although poor posture is caused by the natural process of aging, it could cause adhesion between the coracoacromial ligament and the rotator cuff tendons, especially the SSP tendon, due to increasing pressure and decreasing mobility in elderly people. Adhesion around the coracoacromial ligament is usually observed during arthroscopic rotator cuff repair and its release is necessary to regain ROM and could be an important factor [26]. A stretching strain of the adhesion could cause pain. Furthermore, the internal rotation of the scapula decreases blood flow in the anterior humeral circumflex artery [25], which can influence rotator cuff tendon pathologies. Anterosuperior migration of the humeral head due to poor posture can increase the tension in the rotator cuff tendons, especially at the joint-side and its tensile strain could cause pain. These complex scenarios could explain rotator cuff pathologies and pain in the general population [1]. It is quite important to investigate these phenomena with longitudinal studies in the general population, but this case could have an implication on some of the above mentioned aspects. Careful follow-up is being further continued for evaluating changes in the size of the tendon tear and symptoms. Rotator cuff tears are not the only source of pain and retaining the center of rotation of the glenohumeral joint, including physiotherapy and releasing the adhesions, is an important therapeutic option.
LIST OF ABBREVIATIONS
| ASES | = American Shoulder and Elbow Surgeons |
| CHL | = Coracohumeral Ligament |
| MRI | = Magnetic Resonance Imaging |
| ROM | = Range of Motion |
| SSP | = Supraspinatus |
| UCLA | = University of California at Los Angeles |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
No animals/humans were used for studies that are the basis of this research.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


