All published articles of this journal are available on ScienceDirect.
Modular Versus Monoblock Hemiarthroplasty in Trauma: A 5-Year Retrospective Analysis of Radiographic and Clinical Outcomes
Abstract
Introduction:
Displaced intraarticular neck of femur fractures for low-demand patients are primarily managed with hemiarthroplasty. The optimal implant design for modularity is unclear. Globally and within Australia, the use of monoblock implants varies significantly by location; however, monoblock use is decreasing in Australia in favour of modular systems, with little evidence-based explanation. This study aimed to compare the radiological and clinical outcomes of monoblock and modular hemiarthroplasties.
Methods:
This retrospective cohort study involved patients who underwent hemiarthroplasty for neck-of-femur fractures between 2009 and 2013 at the Gold Coast University Hospital. Leg length and femoral offset were measured from post-operative pelvic radiographs. Revision and mortality rates were extracted from hospital medical records and Australian Joint Registry data.
Results:
A total of 249 patients were evaluated (112 with modular and 147 with monoblock implants). Patient demographics were comparable between the treatment groups; however, the monoblock group comprised significantly older persons. No between-group differences in leg length discrepancies were identified. Femoral offset was under-restored on average by 5.86mm (p<0.05) compared to the uninjured side within the monoblock group. Mortality rates were significantly higher in the monoblock group (23% vs 12%, P=0.026) at the 1-year mark. No significant between-group differences were found in 30-day mortality, length of stay, or revision rates.
Discussion:
Modular hemiarthroplasty was superior for restoring offset in our cohort, but no group differences were noted for leg length. While modular implants seemed better for restoring normal hip anatomy and were associated with a lower 1-year mortality rate, no other advantages were found.
1. INTRODUCTION
Hemiarthroplasty is the gold standard treatment for displaced intra-articular neck-of-femur (NOF) fractures in geriatric low-demand patients. Despite this, no consensus exists regarding the indications for different implant types. This discordance is reflected by the global survey reported by Bhandari et al. [1] and by the significant variance in the Australian National Joint Replacement Registry. In Western Australia, 97% of hemiarthroplasties use modular implants, while in Victoria, up to 30% of patients receive monoblock implants [2]. Despite this variability, the use of the monoblock has consistently decreased over the last 5 years in Australia [2]. Interestingly, there is little scientific evidence to explain this occurrence.
Conceptually, the modular hemiarthroplasty design pro-vides the surgeon with multiple options to restore leg length and femoral offset with a range of stem sizes, with different offset options, and head sizes that allow for minor adjustments during surgery. Reconstruction of the anatomic hip architecture is associated with positive clinical outcomes in patients receiving elective total hip arthroplasty [3, 4]. Although reported less in the literature, emerging evidence suggests similar outcomes for hemiarthroplasty for NOF fractures [5].
The literature is limited by inadequate sample sizes and implant design variations. Consequently, satisfactory com-parisons between implant types used in hemiarthroplasties and their relative performances in hip architecture restoration are scarce. Previous hemiarthroplasty research has centred on post-operative mortality and morbidity; however, modern research has focused on the restoration of radiological architecture and its clinical effect [5-7].
This study examined hemiarthroplasties performed for NOF fractures between 2009 and 2013. The primary objective of this study was to compare implant modularity and effects on leg length and femoral offset restoration. Our secondary objective was to compare the associated clinical outcomes of 30-day and 1-year mortality rate, length of in-hospital stay (LOS), and revision rates in each implant group. Our hypothesis was that modular hemiarthroplasty would provide superior hip architecture restoration while being associated with lower mortality rate and shorter LOS given the underlying selection bias of higher functioning patients within the implant group.
2. METHODS
We identified patients who underwent hemiarthroplasty between January 2009 and December 2013 from our electronic Operating theatre records system (ORMIS) at the Gold Coast University Hospital and Robina Hospital.
Only cases of primary hip hemiarthroplasty for traumatic NOF fractures were included. Any revision cases, pathological fractures, or those with a previous femoral fracture on the side of injury were excluded.
The experience of the operating surgeons varied from registrar to senior consultant. Implant choice was made according to surgeon preference. The standard anterolateral approach (Hardinge) to the hip was used for all cases. The choice of monoblock design was either theETS system (Stryker, Benoist Gerard, Saint Clair Cedex, France) or Thompson’s hemiarthroplasty system. Modular systems included the Spectron (Smith & Nephew, Tuttlingen, Germany) and Exeter V40 (Stryker Benoist Gerard, Saint Clair Cedex, France), with either a bipolar or a unipolar head.
Medical records were accessed via hospital paper charts and electronic medical record systems. In cases where the date of death was unclear or missing from hospital files, the Queensland Registry of Births, Deaths, and Marriages database was used to obtain mortality data. Revision rate data was collected from the Australian Orthopaedic National Joint Replacement Registry (AONJRR) and crosschecked with existing hospital records.
Radiographs had to meet the following previously described criteria for acceptability [8]: (i) anteroposterior pelvis view centred on the pubic symphysis and (ii) sacro-coccygeal joint longitudinally aligned with the pubic symphysis to within 1 cm. For the measurement of femoral offset, the lesser trochanter (LT) had to have a symmetrical size to account for equal femoral rotation. Radiographs were excluded if (i) contralateral fixation had resulted in malunion or had altered normal anatomy and (ii) there were missing post-operative radiographs (patient death prior to obtaining radiographs).
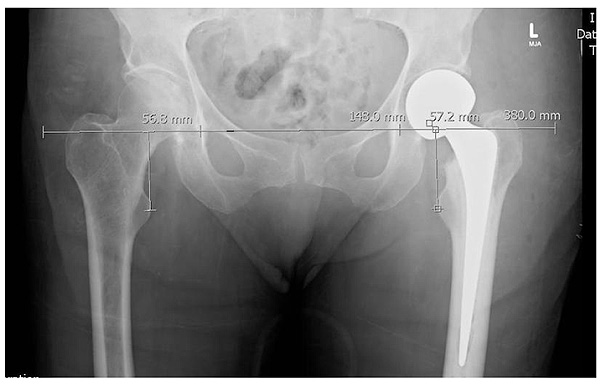
Radiological measurements of femoral offset and Leg Length Discrepancy (LLD) were individually measured and analysed using previously described techniques [3, 8]. The perpendicular distance between LTs and their corresponding position on the inter-teardrop line was measured for each film Fig. (1). All radiographic measurements were performed by one of three orthopaedic registrars.
Patient characteristics were described using means and standard deviations for continuous variables, and count and percentages were used for categorical variables.
| Parameters | Implant type | P-value | |
|---|---|---|---|
| - | Modular (112) | Monoblock (147) | |
| Mean age (years) | 84.35 | 78.00 | 0.0001 |
| Male (%) | 31.3 (35/112) | 31.3 (46/147) | 0.99 |
| ASA score (1–5) | 3 | 3 | 0.68 |
| Operative time (mins) | 113 | 115 | 0.70 |
| Side of surgery (% right) | 43 (48/112) | 50 (74/147) | 0.23 |
| Proportion of nursing home residents (%) | 24 (27/112) | 57 (84/147) | 0.08 |
Twenty-five patient radiographs were randomly selected for re-measurement for inter- and intra-rater analysis. Both inter- and intra-rater agreement were assessed using two methods: the intra-class correlation (ICC) coefficient and the Bland-Altman plots. Only in cases of poor agreement did we include the Bland-Altman plot. For ICC, we employed the one-way components of variance model and the guideline outlined by Cicchetti [9] was used to assess the level of agreement (ICC < 0.4. Poor; ICC 0.4–0.59, Fair; ICC 0.6–0.74, Good; and ICC > 0.75, Excellent).
To compare the monoblock and modular implants, we considered the two continuous outcomes: LLD and femoral offset. General linear modelling was used to calculate both parameters. Analysis of variance (ANOVA) was used to analyse operator experience level, crude LOS, and 30-day and 1-year mortality rates. P values of <0.05 were deemed to be of statistical significance. Finally, the log-rank test was used to determine if there was a difference in LOS between those undergoing the monoblock and modular procedures. All analysis was conducted using the R statistical package [10] and ICCs were generated using the R library, ICC [11]
Ethics approval was obtained from the Gold Coast University Hospital ethics committee.
3. RESULTS
3.1. Patient Demographic
A total of 259 patients were treated with hemiarthroplasty for displaced NOF fractures over the study period (147 patients received monoblock implants and 112 received modular implants). The mean age of patients was 80.7 years and 31.3% (81/259) were male. Monoblock had a statistically significant older group by 6.35 years on average (p< 0.05) Table 1 compared to the modular group. Operative time, surgery side (right versus left), and ASA (American Society of Anesthesiologists) scores were comparable between the groups. There was a non-significant difference in pre-operative residence, where 24% of the modular group, compared to 57% of the monoblock group, resided in nursing homes prior to fracture (Table 1).
Given the conventional rationale for using the more affordable monoblock implant for those with lower mobility demands, premorbid mobility levels were examined and graded based on their mobility aid use prior to surgery. Patients in the monoblock group required mobility aids more frequently Table S1, in agreement with our hypothesis and the increased age of the group.
3.2. Radiographic Results
A total of 244 anteroposterior pelvis radiographs were measured and analysed for LLDs. The average LLD in the monoblock and modular groups was 2.70 mm and 2.36 mm, respectively Table 2, with a tendency of the operated side to be longer than the contralateral side; however, this difference was non-significant (p=0.75).
Only 210 patients were included in the femoral offset analysis, as 34 radiographs were excluded because of asymmetrical femoral rotation. Femoral offset was consistently and significantly under-restored by approximately 5.86 mm in the monoblock group (p<0.001). The femoral offset difference in the modular group was non-significant (Table 4).
Inter- and intra-rater reliability were generally excellent (ICC>0.75) (Table S2). An exception was the inter-rater reliability of operated leg length which yielded an ICC=0.708, which was still in the 'good' range based on the scale proposed by Cichetti [9]. An assessment of the Bland-Altman plot Fig. S1 suggested that this lower level of agreement was attributable to a poor agreement for a single patient.
| - | Implant Type | P-value | |
|---|---|---|---|
| - | Monoblock | Modular | |
| LLD (mm), mean (sd) | 2.70 (7.89) | 2.36 (7.83) | 0.95 |
| - | Implant Type | P-value | |
|---|---|---|---|
| - | Modular | Monoblock | |
| 30-day mortality rate | 6.48% | 7.64% | 0.725 |
| 1-year mortality rate | 12.04% | 23.24% | 0.026 |
| Implant type | Femoral offset (mm) mean (sd) | P-value | |
|---|---|---|---|
| Operated side | Contralateral side | ||
| Monoblock | 37.15 (9.43) | 43.12 (9.08) | <0.05 |
| Modular | 41.47 (8.34) | 42.03 (7.63) | 0.62 |
3.3. Clinical Results
No significant difference was found between the cumulative percentage revision rates at the Gold Coast Hospital (p=0.826) (Fig. S2). Upon further analysing the revision rate data, two cases of dislocations were identified within the monoblock group due to infection, while none were present in the modular group this also did not reach statistical significance. However, a significant difference was found when revision rates were compared nationally for the modular and monoblock groups (p<0.001) (Fig. S2).
Only 245 patients were included in the mortality analysis, as the mortality status of 14 patients could not be confirmed. Within 30 days post-operatively, the monoblock group had a non-significantly higher mortality rate (7.48% vs 6.48%; p=0.725). However, when expanded to a 1-year period, the differences became significant (p=0.026), as the monoblock group (23.24%) had a considerably higher rate of mortality compared to the modular group (12.04%) (Table 3).
Operator experience was also considered between the implant groups and surgeon experience between consultant, training registrar, and unaccredited registrar/principal house officer. 5 patients from the monoblocks were excluded from analysis due to incomplete documentation of the primary operator. No statistically significant differences (p=0.83) were found between the levels of operator experience within the two groups (Table S3).
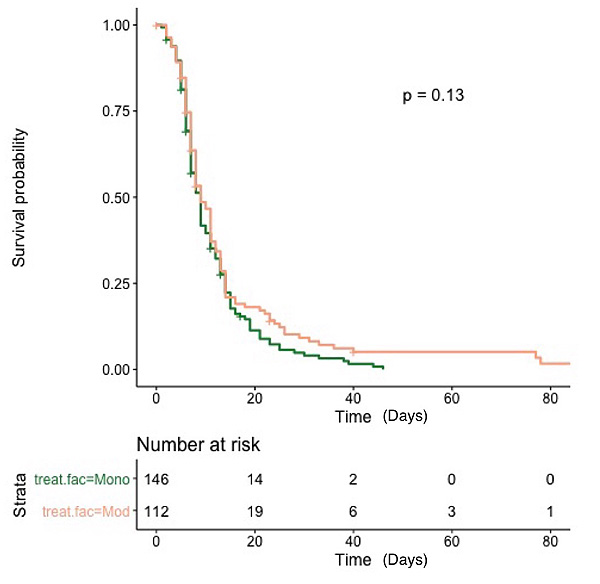
Other clinical outcomes examined in this study included LOS, additional inpatient rehabilitation, orthogeriatric admission usage, and the requirement of a higher level of care on discharge. For LOS, superficially, the modular group had a longer stay (14.35 days) compared to the monoblock group (10.6 days) (p=0.048) (Table 5). However, the log-rank test showed little evidence that LOS differed between the monoblock and modular group (X2LR = 2:3, df = 1, p = 0:13) (Fig. 2).
Similar rates of inpatient/rehabilitation services usage were noted for the modular (48.2%) and monoblock (46.2%; p=0.75) groups (Table 5). There was also no significant difference regarding the requirement for increased care on discharge for either implant group (p=0.48) (Table 5).
| - | Implant Type | P-value | |
|---|---|---|---|
| - | Monoblock | Modular | |
| Length of stay (days) | 10.6 | 14.35 | 0.048 |
| Requiring inpatient rehabilitation / orthogeriatric service (%) | 46.2 (68/147) | 48.2 (54/112) | 0.75 |
| Requiring higher level of care on discharge (%) | 25.8 (34/132) | 21.7 (23/106) | 0.47 |
4. DISCUSSION
With the incidence of NOF fractures increasing on a global scale, and with the ageing population [8] a greater focus is being placed on optimising surgical outcomes. With emerging literature suggesting the importance of restoring hip architecture and a lack of consensus regarding the optimal implant system, it has become crucial to evaluate the performance of these implants. To our knowledge, this is the only study in the literature that has compared radiological and clinical outcomes in a comprehensive variety of implant systems.
4.1. Radiographical Outcomes
Our initial hypothesis that results would be superior for modular implants was only true for femoral offset restoration. The monoblock consistently under-restored femoral offset and the modular implant produced significantly better results. This is due to the dimensional characteristics of the implant within the monoblock group. For example, Thompson’s hemiarthroplasty monoblock produces a limited femoral offset because of its truncated neck design, while the Exeter Trauma Stem monoblock produces a constant femoral offset of 40.00 mm. The mean anatomic femoral offset was 43.12 mm in the monoblock cohort (Table 4).
This finding seems important as femoral offset is directly related to the abductor musculature as it represents the biomechanical lever arm, and restoration is crucial to abductor function [3] and post-surgical outcomes. In total hip arthroplasty, inadequate offset has been associated with the Trendelenburg gait [13] and instability [14], while excess offset has been associated with perceived leg lengthening in early post-operative phases due to excessive abductor tension.
While the effects of hemiarthroplasty have been unclear until recently, there is evidence to suggest its importance. Buecking et al. published a prospective study of 126 patients who underwent hemiarthroplasty for NOF fractures and found a positive correlation between the restoration of femoral offset and both Harris hip scores and activities of daily living outcome scores 12 months after surgery [5]. An earlier study by Hartel et al. [6] found that the anatomic restoration of femoral offset or leg length had no influence on functional outcomes. When the two studies are compared, the validity of Hartel’s findings are called into question. Because of the retrospective design of the Hartel study, they used the ‘median time for mobilisation to hallway’ and days spent in rehabilitation as the primary outcome measures. In contrast, the Buecking study had a prospective design and used validated hip specific scores as the primary outcome measure. With contemporary evidence making a case for the accurate restoration of femoral offset for optimum outcomes, under-restoration of femoral offset may lead to inferior outcomes - this may explain the declining use of monoblocks across Australia [2].
However, this does not exclude the use of all monoblock designs, as the problem may lie within the stem design itself. In our study, the mean anatomical femoral offset across both cohorts was 42.6 mm, which was similar to the findings of Buecking et al and other anatomical studies [15, 16]. We propose that a monoblock system that takes this value into consideration in its stem design, will be more accurate for restoring femoral offset and improving functional outcomes compared to older monoblock systems such as Thompson’s hemiarthroplasty prosthesis.
Post-hip arthroplasty LLD is a significant parameter affecting gait patterns [16], dislocation rates, and sciatic nerve function [17], with significant LLD also increasing pulmonary, cardiac, and neuromuscular loading during mobilisation [16]. Given that the target population for hemiarthroplasty are geriatric patients with multiple cardiopulmonary comorbidities and the treatment goal is the restoration of pre-morbid mobility, leg-length control becomes an important technical requirement.
We found no statistically significant difference in LLD between the modular and monoblock groups. This is likely due to the Stryker ETS comprising for 42% of the monoblock group. As the ETS is a slim, collarless, cemented stem that does not rely on the level of the neck-cut to dictate implant placement; this would allow for adjustment during cementation to obtain correct leg lengths
4.2. Clinical Outcomes
When analysing the clinical outcomes of this particular subsect of patients, we recognise the typical NOF patients who receive hemiarthroplasties commonly have dementia, are predominantly nursing home patients and are minimally ambulant; due to these factors, most hospital in Australia including our institution, do not routinely follow up these patients. Thus, we have chosen to focus on analysing revision rates, mortality rates and LOS instead of functional scores as these are well documented and objective clinical indicators when assessing a surgical intervention in this particular subsect of patients.
No differences in revision rate were identified by the Australian National Joint Registry between monoblock and modular NOF fracture hemiarthroplasties performed at the Gold Coast Hospital (Fig. S2). The two cases of dislocations that were present within the monoblock group were due to prosthetic infection, which is unlikely to be impacted by implant modularity. These findings were reaffirmed by Rogmark et al. in a Swedish Registry study [12]. where they demonstrated cemented monoblock designs did not increase revision rates or dislocation rates compared to modular groups [17].
Within our cohort, although the 30-day rate was not significantly different between both implant groups, a significant difference in the 1-year mortality rate was noted. This is, however, unlikely to be due to implant selection but is rather the consequence of an inherent selection bias amongst the two treatment groups as the monoblock group was, on average, 83.45 years old, 6.35 years older than the modular group.
| - | Thompsons | ETS | Modular Spectron | Modular Exeter |
|---|---|---|---|---|
| Cost ($AUD) | 411.23 | 540.00 | 2549.00 | 3312.00 |
LOS was also analysed. While looking at the crude data, the monoblock unexpectedly had a shorter LOS compared to the modular group (Table 5). This was contrary to our hypothesis, given that the patients in the monoblock group were older and were conventionally those with lower physical function. Upon closer inspection, this result was confounded, firstly, by a statistical outlier within the modular group, which included a patient who had a 201-day admission due to multiple relapsing medical issues, involving care under several medical treatment teams. Secondly, given that LOS is a time-to-event variable, statistically, it would be susceptible to right-skewing or censoring. Thus, an in-hospital death may be statistically misinterpreted as a successful discharge. To address this issue, a log-rank test was performed to account for censoring, while the statistical outlier patient was removed from the analysis, as their prolonged admission was not orthopaedically related. The Log-Rank test indicates little evidence that the length of stay experience differed between those under going the monoblock and modular procedures.
Outside of the clinical factors, one of the key challenges of managing neck of femur fractures is the financial burden the condition places upon the global health system. Currently in Australia as of 2016 the average cost of an admission for the diagnosis of NOF is $16.578 [18]. One of the key differences in the two classes of implants is the significant cost difference Table 6 - given within our series we have unable to show a statistical difference between revision rate, LOS and 30-day mortality - there is a strong case advocating for the use of a monoblock counter-part as a cost-effective method to manage the minimally ambulant geriatric NOF patient.
4.3. Limitations
Our study has several limitations, primarily because of its retrospective design. This resulted in radiographs being excluded due to unsatisfactory patient positioning. We accepted that femoral offset measurements would be impacted via the femoral rotation. Buecking et al. [5] attempted to rectify this issue in their study by calculating a ‘rotationally corrected femoral offset’, which was derived as a function of the ratio between the implant’s true neck-shaft angle and the angle in which it appears on plain radiographs. However, Buecking’s cohort all had identical implants and, hence, the same neck-shaft angles. In comparison, this method may not have been applicable to our study given the cohort’s different choices of implants with heterogeneous neck-shaft angles, as revealing implant model information such as the neck-shaft angle would diminish blinding and consequently influence measurement bias.
Future investigations should be prospective. This will not only allow the improved standardisation of plain radiographs to measurement accuracy and statistical power, but also grant access to a broader range of clinical outcomes such as range of motion, clinical hip scores, or Visual Analogue Scale for pain scores, to further explore the relationship between hip architecture restoration associated with implant modularity.
CONCLUSION
Monoblock implants under-restored femoral offset, but not leg length, in NOF hemiarthroplasties. Within our cohort, there was no significant difference in LOS, 30-day mortality, discharge destination, or revision rates between both implant groups. Monoblock hemiarthroplasty is still a suitable alternative for the elderly undergoing hemiarthroplasty despite the overall decreased national usage within Australia, especially when implant costs are considered. Whilst there has been contemporary evidence associating under-restoration of femoral offset with inferior functional scores in patients undergoing hemiarthroplasty, it should not completely discredit the monoblock implant. To address this challenge, we recommend either using a monoblock stem with a set offset that approximates the average offset of the general population or to use a modular stem that allows a tailored offset.
LIST OF ABBREVIATIONS:
| NOF | = Neck of Femur |
| ETS | = Exeter Trauma Stem |
| LOS | = Length of Stay |
| LLD | = Leg length discrepancy |
| LT | = Lesser Trochanter |
| ASA | = American Society of Anesthesiologist |
| ICC | = Intra-class correlation |
| FO | = Femoral Offset |
AUTHORS' CONTRIBUTIONS
HK undertook significant involvement in manuscript construction and revisions, data collection and statistical analysis.
AMcB provided significant guidance with manuscript writing, manuscript revisions and study design.
AMcl provided significant effort in data collection and statistical analysis.
WO provided data collection template and manuscript editing. HKhan provided statistical analysis
PG provided senior mentorship and study design
All authors have read and approved the final manuscript
ETHICAL APPROVAL AND CONSENT TO PARTICIPATE
Ethics approval was obtained from the Gold Coast University Hospital ethics committee. Consent for data access for granted by the data custodian of Gold Coast university Hospital
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Not applicable
CONFLICT OF INTEREST
PG is a paid consultant for Amplitude, all other authors have no competing interests
ACKNOWLEDGEMENTS
Declared none.
SUPPLEMENTARY MATERIAL
Supplementary material is available on the publishers Website along with the published article.


