RESEARCH ARTICLE
Distal Linear Metatarsal Osteotomy Combined with Akin Osteotomy for Hallux Valgus with Hallux Valgus Interphalangeus
Kazuki Kanazawa*, Ichiro Yoshimura, Tomonobu Hagio, Takuaki Yamamoto
Article Information
Identifiers and Pagination:
Year: 2019Volume: 13
First Page: 34
Last Page: 41
Publisher ID: TOORTHJ-13-34
DOI: 10.2174/1874325001913010034
Article History:
Received Date: 04/03/2018Revision Received Date: 07/1/2019
Acceptance Date: 16/1/2019
Electronic publication date: 31/1/2019
Collection year: 2019

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background:
Minimally invasive distal linear metatarsal osteotomy is commonly performed to correct mild-to-moderate hallux valgus. The technique is easy to perform, fast, and has a low complication rate with satisfactory clinical results. However, it has so far not been applied to hallux valgus with concomitant hallux valgus interphalangeus deformity.
Objective:
We aimed to investigate the short-term clinical results of distal linear metatarsal osteotomy combined with Akin osteotomy in hallux valgus with concomitant hallux valgus interphalangeus deformity.
Methods:
We retrospectively reviewed 10 patients (10 feet) who underwent surgery for hallux valgus with hallux valgus interphalangeus between 2012 and 2016. Akin osteotomy was performed and fixated with a screw/K-wire, followed by distal linear metatarsal osteotomy and K-wire fixation. Clinical evaluations pre- and postoperatively used the Japan Society for Surgery of the Foot (JSSF) scale and the Visual Analog Scale (VAS). Radiography pre-and postoperatively assessed the hallux valgus, hallux valgus interphalangeus, and the intermetatarsal angle.
Results:
The mean follow-up period was 20.2 months. Both the JSSF and VAS score improved significantly, from 64.5 to 90.0 and from 5.5 to 1.1, respectively. In all patients, bone healing was complete within four months with no osteonecrosis of the metatarsal head or malunion at the osteotomy site. The hallux valgus angle improved from 31.5° to 7.7°, the hallux valgus interphalangeus angle from 17.2° to 5.8°, and the intermetatarsal angle from 11.7° to 5.5°.
Conclusion:
Distal linear metatarsal osteotomy combined with Akin osteotomy safely and effectively corrects mild-to-moderate hallux valgus with hallux valgus interphalangeus deformity.
1. INTRODUCTION
Hallux Valgus (HV) is a common deformity of the forefoot. It is more prevalent in females and the elderly, and characterized by malposition of the first metatarsophalangeal joint caused by lateral deviation of the proximal phalanx of the great toe combined with medial deviation of the first metatarsal bone with bunion formation. Conservative treatments include properly fitting footwear, stretching, and the use of an orthosis. However, the value of conservative treatment has been questioned. If conservative treatment fails, surgical treatment may be considered. Over 150 different operation techniques have been described for the correction of HV [1]. Good clinical results have been reported with proximal metatarsal osteotomies, distal metatarsal osteotomies, and diaphyseal metatarsal osteotomies [2].
Minimally invasive surgery is becoming increasingly common. Distal linear metatarsal osteotomy (DLMO; modified Bösch technique) as a minimally invasive technique has been performed for the correction of mild-to-moderate HV [3-6]. DLMO has the advantages that it is technically easy to perform, has relatively short operating times, and low complication rates. The technique was developed for rapid recovery and better cosmetic appearance, and satisfactory clinical results have been reported to this end in previous studies [3-5, 7-9]. DLMO consists of fixation with a single K-wire that passes under the subcutaneous tissue to the distal end of the big toe. This approach has so far not been applied to cases of Hallux Valgus Interphalangeus (HVI) deformity occurring together with hallux valgus. HVI is defined as a lateral deviation of the distal phalanx of the big toe that exceeds 10° [10].
We decided to combine Akin osteotomy with DLMO (DLMO-A) to improve fixation for HV with concomitant HVI. The present study aimed to investigate the short-term clinical and radiological results of DLMO-A in the treatment of this combined deformity.
2. PATIENTS AND METHODS
2.1. Patients
This retrospective, descriptive study included 10 patients (10 feet) who had been diagnosed with both HV and HVI and were treated with DLMO-A between November 2012 and November 2016 at our institution. Of the 10 patients, nine were female and one was a male. The mean age at surgery was 59.8 years (range, 43–77 years), and the mean duration of follow-up was 20.2 months (range, 12–31 months). The inclusion criterion was painful primary mild-to-moderate HV with idiopathic HVI deformity (Fig. 1). The exclusion criteria were hallux rigidus and a history of previous surgery of the affected great toe. All patients received conservative treatment for at least three months before surgery.
This study was approved by the Research Ethics Com-mittee of Fukuoka University (2018M063), and all subjects provided informed consent before study inclusion.
Clinical and radiographic investigations were performed at the initial examination and at the final outpatient follow-up visit. With regard to clinical assessments, we evaluated the Japan Society for Surgery of the Foot (JSSF) score, the Visual Analog Scale (VAS) score, and recorded any postoperative complications. The JSSF score is a 100-point clinical score comprising the following three items: a pain score (40 points maximum), functionality (45 points maximum), and alignment (15 points maximum) [11]. The VAS score ranges from 0 to 10, with 0 representing no pain and 10 representing the worst pain imaginable. Additionally, the self-administered foot evaluation questionnaire (SAFE-Q) score [12, 13] was used. The SAFE-Q has the following five subscales: 1) pain and pain-related, 2) physical functioning and daily living, 3) social functioning, 4) shoe-related, and 5) general health and well-being. The subscales are scored from 0 to 100. With regard to radiographic assessments, we evaluated the HV Angle (HVA), first Intermetatarsal Angle (IMA), and HVI Angle (HVIA) in standing dorsoplantar and lateral radiographs (Fig. 2).
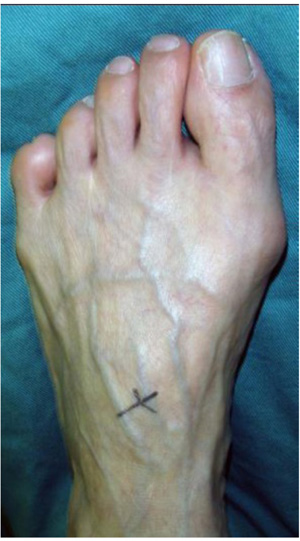 |
Fig. (1). Representative preoperative image of hallux valgus with hallux valgus interphalangeus deformity (case 4). |
2.2. Operative Technique
In all patients, surgery was performed in the supine position under epidural anesthesia with intravenous sedation, a pneumatic ankle tourniquet (pressure set to 250 mmHg), and an image intensifier. Akin closing wedge osteotomy was per-formed at the middle of the proximal phalangeal shaft through a 1.5 cm dorsal skin incision. The first osteotomy was performed parallel to the phalangeal base, and the second osteotomy was performed parallel to the articular surface of the phalangeal head. The thickness of the bony wedge was decided based on the required correction of the HVIA. Fixation was performed with one mini screw or K-wire from the proximal to the distal part of the phalanx. Lateral soft tissue release was performed for the first and second metatarsal heads through a 1.5 cm dorsal skin incision if HV could not be corrected with closed manual reduction. In the next step, a 1.5 cm skin incision was made on the medial aspect of the neck of the first metatarsal bone. A periosteal elevator was used to strip the neck of the first metatarsal bone. A 2.0 mm K-wire was inserted manually from the incision to the medial side of the big toe using the retrograde technique. Osteotomy was performed with a micro-bone saw at the subcapital level of the metatarsus, perpendicular to the metatarsal shaft in the sagittal plane, and parallel to the metatarsal shaft in the coronal plane. Lateral translation of the distal fragment was sufficiently obtained, and the K-wire was pushed back into the medullary canal of the first metatarsal shaft (Figs. 3 and 4).
Weight-bearing on the heel in special postoperative shoes was allowed on the first postoperative day. The K-wire was removed six weeks postoperatively. The patients were allowed to wear normal shoes, and forefoot weight-bearing was encouraged from eight weeks postoperatively.
3. RESULTS
Clinical and radiological results are depicted in Table 1. There were statistically significant improvements in all JSSF, SAFE-Q subscale, and VAS scores, as well as in the HVA, IMA, and HVIA at the final follow-up.
 |
Fig. (4). Postoperative image with the location of incisions. The photograph shows the result of the minimally invasive approach with two 1.5 cm (dorsal and medial) sutures of the skin (case 4). |
| Patient | Gender | Age | Side | Follow-up (months) |
JSSF Pre/Final |
VAS Pre/Final |
HVA Pre/Final |
IMA Pre/Final |
HVIA Pre/Final |
Fixation Method (Akin) |
Complications |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 43 | R | 31 | 69/90 | 6/1 | 29/1 | 10/3 | 21/8 | Screw | No |
| 2 | F | 61 | R | 29 | 64/85 | 5/2 | 38/11 | 13/5 | 15/8 | Screw | No |
| 3 | F | 71 | L | 13 | 64/90 | 6/1 | 30/3 | 11/3 | 19/9 | Screw | No |
| 4 | F | 77 | R | 18 | 67/90 | 4/1 | 31/8 | 12/4 | 18/2 | Screw | No |
| 5 | M | 63 | L | 32 | 60/90 | 5/1 | 22/5 | 14/8 | 17/0 | K-wire | Restriction of IP joint |
| 6 | F | 51 | L | 12 | 59/90 | 4/1 | 39/12 | 12/6 | 18/4 | Screw | No |
| 7 | F | 55 | R | 14 | 67/85 | 7/2 | 33/10 | 11/7 | 16/7 | Screw | No |
| 8 | F | 62 | L | 22 | 64/100 | 5/0 | 31/9 | 12/6 | 14/9 | Screw | No |
| 9 | F | 48 | L | 15 | 67/100 | 6/0 | 28/5 | 10/5 | 15/6 | Screw | No |
| 10 | F | 67 | R | 16 | 64/80 | 5/2 | 34/13 | 12/8 | 19/5 | Screw | No |
| - | Preoperative | Postoperative | p-value |
|---|---|---|---|
| JSSF score | 64.5 ± 3.2 | 90.0 ±6.2 | < 0.001 |
| VAS score | 5.3 ± 0.9 | 1.1 ± 0.7 | < 0.001 |
The mean JSSF score significantly improved from 64.5 preoperatively to 90.0 postoperatively (p < 0.001). The mean VAS score also significantly improved from 5.3 preoperatively to 1.1 postoperatively (p < 0.001) (Table 2).
The mean SAFE-Q subscale scores significantly im-proved in all patients after surgery (p < 0.001) (Table 3).
The mean HVA significantly improved from 31.5° (preoperatively) to 7.7° (postoperatively) (p < 0.001), the mean IMA from 11.7° to 5.5° (p < 0.001), and the mean HVIA from 17.2° to 5.8° (p < 0.001) (Figs. 5-7 and Table 4). No patient developed transfer metatarsalgia, infection, non-union, malunion, or avascular necrosis of the first metatarsal head. However, a mild restriction of the range of motion of the inter-phalangeal joint was observed postoperatively in one patient.
| Subscale | Preoperative | Postoperative | p-value |
|---|---|---|---|
| Pain and pain-related | 68.4 ± 7.8 | 96.3 ± 2.3 | < 0.001 |
| Physical functioning and daily living | 86.4 ± 6.3 | 98.8 ± 1.5 | < 0.001 |
| Social functioning | 68.3 ± 11.0 | 99.4 ± 0.2 | < 0.001 |
| Shoe-related | 52.8 ± 9.2 | 87. 0± 1.7 | < 0.001 |
| General health and well-being | 71.6 ± 11.8 | 98.5 ± 0.7 | < 0.001 |
 |
Fig. (5). Representative dorsoplantar and lateral radiographs 29 months after DLMO-A. Complete healing of the osteotomies is visible (case 2). |
 |
Fig. (6). Representative dorsoplantar and lateral radiographs 31 months after DLMO-A. Complete healing of the osteotomies is visible (case 1). |
 |
Fig. (7). Representative dorsoplantar and lateral radiographs 18 months after DLMO-A. Complete healing of the osteotomies is visible (case 4). |
| - | Preoperative | Postoperative | p-value |
|---|---|---|---|
| HVA (°) | 31.5±4.9 | 7.7±4.0 | < 0.001 |
| IMA (°) | 11.7±1.3 | 5.5±1.8 | < 0.001 |
| HVIA (°) | 17.2±2.2 | 5.8±3.0 | < 0.001 |
4. DISCUSSION
Many different surgical procedures have been described for the surgical treatment of HV depending on the degree of the deformity. In recent years, minimally invasive surgery has become increasingly common [3-5, 7-9, 14-16]. Percutaneous distal first metatarsal osteotomy was first described by Bösch et al. in 1990 [7], and satisfactory results were reported in 2000 [3]. Magnan et al. reported a mean total American Orthopedic Foot and Ankle Society score of 88.2 (out of a total of 100) using percutaneous distal osteotomy [4]. Seki et al. reported a mean total JSSF score of 90.4 using DLMO with selective release of lateral soft tissue after a mean postoperative follow-up of 38.8 months [8].
In our study, a mean total JSSF score of 90.0 was documented for a mean postoperative follow-up of 20.2 months, and there were no serious complications. However, a mild restriction of the range of motion of the interphalangeal joint was observed postoperatively in one patient. We considered this joint stiffness to be associated with the K-wire placement to temporarily fix the metatarsophalangeal and interphalangeal joints. Previous studies have reported K-wire removal four [3, 7-9], six [5, 15], and seven [14] weeks postoperatively. In the present study, the K-wire was removed six weeks postoperatively. However, we considered that it is necessary to remove the wire earlier, ideally once callus formation is observed.
At the same time, complications and poor outcomes have been reported for minimally invasive methods in other articles [14, 16]. Therefore, the use of DLMO for the treatment of HV is still controversial. DLMO involves fixation with only a single K-wire that is passed under the subcutaneous tissue to the distal end of the big toe. Accordingly, DLMO has not been applied for HV with HVI deformity. We decided to use DLMO and additionally perform Akin osteotomy to improve fixation. Akin osteotomy is a popular technique for isolated HVI [17-19], and the fixation in Akin osteotomy can also be performed with a K-wire, monofilament wire or screw [20, 21], which aligns with the minimally invasive approach of DLMO.
Chiang et al. reported that Bösch osteotomy, despite a generally reliable correction of the deformity, resulted in 12.5% of early arthritic changes [6]. They explained the degenerative change as being related to an increased reactive force after extensive correction and immobilization of the metatarsophalangeal joint with a K-wire. We believe that overcorrection of HV with a single K-wire in case of concomitant HVI can increase the stress load on the metatarso-phalangeal joint, and alignment correction with the Akin procedure can help to reduce the stress load on the metatarso-phalangeal joint.
The present study has some limitations. It was a retrospective study with a small number of patients (a total of 10 feet operated) and a short postoperative follow-up (mean 20.2 months).
CONCLUSION
DLMO-A safely and effectively corrects mild-to-moderate HV with HVI, however, the postoperative follow-up period is short. It is necessary to conduct a longer follow-up to detect possible stiffness or new deformities. Further studies with a larger number of patients and a longer follow-up period are needed to adequately assess the value of DLMO-A in HV with concomitant HVI.
LIST OF ABBREVIATIONS
| DLMO | = Distal Linear Metatarsal Osteotomy |
| DLMO-A | = Distal Linear Metatarsal Osteotomy Combined with Akin Osteotomy |
| HV | = Hallux Valgus |
| HVA | = HV Angle |
| HVI | = Hallux Valgus Interphalangeus |
| HVIA | = HVI Angle |
| IMA | = Intermetatarsal Angle |
| JSSF | = Japan Society for Surgery of the Foot |
| SAFE-Q | = Self-Administered Foot Evaluation Questionnaire |
| VAS | = Visual Analog Scale |
FUNDING
No funding was obtained for this study.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Research Ethics Committee of Fukuoka University (2018M063), and all subjects provided informed consent before study inclusion.
HUMAN AND ANIMAL RIGHTS
No animal were used in the research, All procedures performed involving human participants were in accordance with the Helsinki Declaration of 1975, as revised in 2008.
CONSENT FOR PUBLICATION
Written informed consent was obtained from all participants for prospective data collection, follow-up examinations, and publication of the clinical results and images in international journals.
CONFLICT OF INTEREST
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
ACKNOWLEDGEMENTS
We would like to thank Editage (www.editage.jp) for English language editing.










