All published articles of this journal are available on ScienceDirect.
Delayed Internal Fixation of Distal Radius and Bimalleolar Ankle Fractures Does Not Increase Surgical Time
Abstract
Introduction:
It is commonly believed that delay in fracture fixation of more than two weeks results in increased Surgical Time (ST), due to scar and callus formation at the fracture site. Reducing ST can lower hospital costs and decrease radiation exposure.
Methods and Results:
A retrospective chart review was conducted to investigate whether early fracture care (up to 2 days after injury) results in decreased ST and radiation exposure compared to delayed fracture care (> 14 days after injury) for distal radius and bimalleolar ankle fractures. A total of 581 radius and ankle fractures that underwent surgical fixation between 2014 and 2017 were identified from the OR registry. Cases with only a single volar locking plate for the distal radius and constructs consisting of 2 medial malleolar screws, third tubular plate, and up to 1 syndesmotic screw for the ankle were included. The mean ST for distal radius cases done up to 2 days after injury was significantly greater than ST for distal radius cases done > 14 days after injury (125.78±29.75 minutes versus 105.83±24.82 minutes respectively , p=0.06). The mean ST for ankle fracture cases done less than 2 days did not differ from ST for ankle fracture cases done > 14 days after injury (140.86±28.15 minutes versus 173.22±39.98 minutes respectively, p=0.06).
Conclusion:
There was no significant difference in radiation exposure. Delaying surgery for distal radius and bimalleolar ankle fractures > 14 days after injury does not seem to significantly affect the duration of surgery or radiation exposure.
1. INTRODUCTION
Open Reduction and Internal Fixation (ORIF) of radius and ankle fracture surgeries are some of the most common cases seen by orthopedic surgeons today. Distal radius fractures make up 20% of all fractures treated in the emergency room and make 8% to 15% of all bone-related injuries in adults [1, 2]. Ankle fractures have an incidence rate of 174 fractures per 100,000 adults every year [3]. In addition, the costs of treating these fractures are rising. In 2007, Medicare paid $170 million in distal radius fracture treatment payments, and it is projected that the costs could increase to $240 million if internal fixation continues to be used [4]. The economic burden for foot and ankle surgery was $11 Billion for the Medicare population in 2011, with a 38% increase since 2000 [5].
Quality control mechanisms can be utilized to lower hospital costs associated with these types of fracture treatments. Treating distal radius and ankle fractures as out patients can reduce hospital costs, but may result in significant delays in the time of surgery. A prevailing hypothesis is that delayed fracture fixation results in a larger amount of scar and callus tissue formation [6], leading to longer surgical times. Thus, delaying surgery for two weeks or more (enough time for initial callus to form) may lead to longer surgical times as well as increased radiation exposure to the patient and operating room staff. The specific effect of time to fracture fixation on the ability of the surgeon to execute surgical steps is unknown. Research has been conducted on how the timing of surgery affects wound infection or functional outcomes, but only one study mentioned operative times between early and delayed treatments for ankle cases [7].
The goal of this study is to investigate whether early fracture care (≤ 2 days after injury) results in decreased surgery time and radiation exposure compared to delayed fracture care (> 14 days after injury) for bimalleolar ankle and distal radius fractures. Our hypothesis was that delaying distal radius or ankle ORIFs will lead to increased surgical time and radiation exposure.
2. MATERIALS AND METHODS
A retrospective chart review was conducted at a level one trauma center. This study was awarded Institutional Review Board (IRB) exemption by our institution’s committee for health research. We queried the operating room registry for radius and ankle fractures that underwent open reduction and internal fixation between October 2014 and October 2017. From there, we screened for adult age between 18 and 65. Children were excluded from the study due to the likelihood of alternative fixation strategies. Patients above 65 were excluded due to the likelihood of osteoporotic (pathologic) bone, requiring alternative strategies for reduction and fixation, and because the majority of the patients older than 65 with distal radius fractures are treated non-operatively in our institution. A trauma fellowship-trained orthopedic surgeon selected cases with only a single volar locking plate for the distal radius and constructs consisting of 2 medial malleolar screws, third tubular plate on the fibula, and up to 1 syndesmotic screw for the ankle. Any cases with additional screws or fixation devices and additional surgeries were excluded to maintain the study population as homogeneous as possible. Ankle fractures were classified according to the Weber classification. Distal radius fractures were classified as being intra-articular or extra-articular. Open fractures were identified as such, but included in the final analysis, since it was felt that the added irrigation and debridement time will not be significant enough to sway the results in a clinically significant way. We included in our final analysis only bimalleolar ankle cases and distal radius cases that occurred ≤ 2 days or > 14 days after injury.
Statistical analysis was performed using Microsoft Excel for Mac (Version 16.9) and R version 3.5.0 (2018- 04-23). Primary outcome variables were Surgical Time (ST) measured in minutes and radiation exposure (measured in minutes and milligrays). We used means, standard deviations and confidence intervals to describe the primary variables and patients age. The Shapiro-Wilk normality test was used to test whether we could use parametric test to analyze the data. After verifying normality (p values for all datasets were > 0.05) a student’s t-test was used to identify statistically significant differences between the study populations. A p value of < 0.05 was considered statistically significant.
3. RESULTS
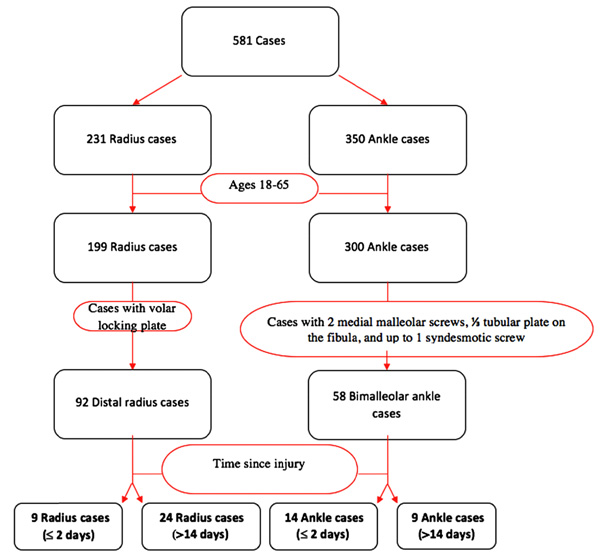
A total of 581 radius and ankle fracture cases (231 radius operations and 350 ankle operations) were identified from the operating room registry from October 2014 to October 2017. We identified 199 distal radius fracture patients and 300 ankle fracture patients between the ages of 18 and 65. For the radius group, 92 cases included a volar locking plate and for the ankle group, 58 cases involved constructs consisting of 2 medial malleolar screws, third tubular plate on the fibula, and up to 1 syndesmotic screw. For the distal radius group, 9 of the cases took place ≤ 2 days after injury and 24 were performed > 14 days after injury. For the bimalleolar ankle group, 14 of the cases took place ≤ 2 days after injury and 9 were performed > 14 days after injury. Fig. (1) summarizes how the final study population was obtained.
The mean ST for distal radius cases done ≤ 2 days after injury was 125.78±29.75 minutes (median 114, range 95-179 minutes). The mean ST for distal radius cases done > 14 days after injury was 105.83±24.82 (median 107, range 56-162 minutes). This difference was not statistically significant (p = 0.06). The groups did not differ significantly in patient age or in fracture classification (Table 1). There was one open fracture in the early surgery group. Removal of this patient from the analysis resulted in a surgical time of 119.25±23.59 minutes for the early surgery group, which was still not statistically significant from the delayed surgery group (p=0.194). Radiation exposure data was not available for the majority of the distal radius cases (perhaps due to the use of mini C-arms in these cases).
The mean ST for ankle fracture cases done ≤ 2 days after injury was 140.86±28.15 minutes (median 136, range 103-202 minutes). The mean ST for ankle cases done > 14 days after injury was 173.22±39.98 minutes (median 171, range 123-228 minutes). This difference was not statistically significant (p = 0.062). The groups did not differ significantly in patient age, however, the early surgery group had relatively more Weber B fractures and more syndesmosis fixations than the delayed surgery group (Table 2). Removal of all cases of syndesmosis fixation from the analysis resulted in surgical times of 145.5±32.03, 160.5±41.67 for the early surgery and delayed surgery groups respectfully, with a p value of 0.459, indicating no statistically significant difference. There were two open fractures in the early surgery group. Removal of these patients from the analysis resulted in a surgical time of 143.25±29.47 minutes for the early surgery group, which was still not statistically significant from the delayed surgery group (p=0.09). The mean fluoroscopy time for ankle fracture ORIF cases done ≤ 2 days after injury was not different from the mean fluoroscopy time in cases done > 14 days after injury (0.85 ± 0.23 minutes versus 0.84 ± 0.33 minutes, p = 0.49). The mean amount of radiation for ankle fracture ORIF cases done ≤ 2 days after injury was not different from the mean amount of radiation in cases done > 14 days after injury (1.19 ± 0.6 mGy versus 1.43 ± 0.65 mGy, p = 0.31).
| – | ≤ 2 Days to Surgery | > 14 days to Surgery |
|---|---|---|
| Number of cases | 9 | 24 |
| Age (years) | 49.2±12.1 | 47.0±11.9 |
| Open Fractures | 1 | 0 |
| Extra-articular Fractures | 4 (44%) | 12 (50%) |
| Intra-articular Fractures | 5 (56%) | 12 (50%) |
| Surgical time (minutes) | 125.78±29.75 * | 105.83±24.82 * |
4. DISCUSSION
This study is the first to report on the relationship between delaying surgery and surgical time for distal radius and bimalleolar ankle fractures. Prevailing thought among orthopaedic traumatologists is that delaying surgery will lead to increased callus formation at the fracture site [6] and possibly increased difficulty and time of surgery. Our hypothesis, therefore, was that delaying surgery would increase both surgical time and use of fluoroscopy during surgery. This hypothesis was rejected by our study since we could not demonstrate any adverse effects of delaying surgery in both ankle and distal radius Open Reduction and Internal Fixation (ORIF).
A retrospective review on closed Weber B bimalleolar or bimalleolar equivalent ankle fractures reported no significant difference in operative time for early versus delayed treatment [7]. Our study also produced similar results, confirming no. significant difference in operative time with delayed treatment. The literature discussing the effect of delaying surgery on procedure time is sparse, but many studies have investigated the relationship between delaying treatment and functional outcome scores or wound infection. One distal radius study reported similar quick Disability of Arm, Shoulder and Hand (DASH) scores, volar tilt, radial inclination, and radial length for both <21 days and >21 days treatment groups [8]. A previous ankle fracture study concluded that fractures treated within one day experienced no wound complications whereas 11% of the cases in the delayed group presented with wound infection and lower functional outcome American Orthopaedic Foot and Ankle (AOFAS), Olerud-Molander Ankle (OMAS) and Visual Analog Scale (VAS) pain scores [9]. Another study confirmed the higher incidence of wound infection (17.6% vs. 3.0%) in the delayed ankle treatment group along with a prolonged hospital stay [10]. However, a more recent retrospective chart review study shows no association with delayed surgery on the length of stay and complication rate. However, patients operated on after 6 days showed lower OMAS, Lower Extremity Functional Scale (LEFS), and Self reported Foot and Ankle (SEFAS) functional outcome scores [11]. Delaying surgery on ankle fractures beyond 24 hours was also found to be associated with increased hospital stay [12]. The results of the current study suggest that outcome measures and individual health system operational costs should dictate decision making on whether to delay ORIF for distal radius or ankle fractures. The surgeon should not expect significant adverse effects on surgical time or radiation time by delaying these surgeries.
| ≤ 2 Days to Surgery | > 14 days to Surgery | |
|---|---|---|
| Number of cases | 14 | 9 |
| Age (years) | 44.3±14.7 | 43.1±15.2 |
| Open Fractures | 2 | 0 |
| Weber B Fractures | 10 (71%) | 4 (44%) |
| Weber C Fractures | 4 (29%) | 5 (56%) |
| Syndesmosis fixation | 6 (43%) | 3 (33%) |
| Surgical time (minutes) | 140.86±28.15 * | 173.22±39.98 * |
| Fluoroscopy time (minutes) | 0.85 ± 0.23 ** | 0.84 ± 0.33 ** |
| Radiation amount (milligrays) | 1.19 ± 0.6 *** | 1.43 ± 0.65 *** |
This study has some noteworthy limitations. Firstly, the study is retrospective in nature and was conducted at only one institution. Therefore, it is uncertain whether the results are generalizable to other trauma centers. Secondly, the surgeries that underwent ORIF for both the ankle and distal radius group were not performed by a single surgeon. This adds variability to the data since different surgeons conduct ORIF at their own respective pace. Thirdly, the ankle group included some cases with the incorporation of the syndesmotic screw and some without. The reason for the surgeon variability and inclusion of up to one syndesmotic screw was the limited data provided by the operating room registry for only the last 3 years. Finally, because of the small sample size, this study may have been underpowered to detect a statistically significant difference between the sample groups. Although not reaching statistical significance, there was a trend (p=0.06) in the ankle fracture group toward decreasing surgical time with early surgery. However, this trend was not seen when we excluded open fractures and there was an opposite trend in the distal radius fractures. These findings together suggest that the overall conclusions of the study were unlikely to change even with larger sample size. Moving forward, a prospective study with fewer surgeons can be conducted to attempt to show a clearer relationship between delay in surgery and operation length.
CONCLUSION
This study was not able to demonstrate that delaying ORIF of bimalleolar ankle fractures and distal radius fractures resulted in a clinically or statistically significant increase in procedure time or radiation exposure. Based on the results of this study, the surgeon should take into consideration other factors (reported outcomes, cost, health system operational consideration, etc.) in making the decision about surgical timing. A larger prospective clinical trial is warranted to confirm these findings.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was awarded Institutional Board Review (IRB).
HUMAN AND ANIMAL RIGHTS
No animals/humans were used for studies that are the basis of this research.
CONSENT FOR PUBLICATION
Not applicable.
CONFLICT OF INTEREST
Authors have not received grant support or research fun-ding, and do not have any proprietary interests in the material described in the article or any other conflict of interest.
ACKNOWLEDGEMENTS
We would like to thank Luke Karl for his help in data collection.


