All published articles of this journal are available on ScienceDirect.
Patellar Tendon Rupture Following Total Knee Arthroplasty
Abstract
Background:
Patellar tendon rupture following Total Knee Arthroplasty (TKA) is rare. There is no consensus on optimal treatment.
Methods:
All patients who underwent a primary repair of a traumatic patellar tendon rupture following a TKA between 2008 and 2016, were retrospectively reviewed. Patient information, implant, repair type (anchor vs. bone tunnel), graft use, and complications were recorded.
Results:
Twenty-six patients met our inclusion criteria. The average age was 69.7+11 years. There were 19 females (73.1%). The average time from TKA to PT rupture was 13.6 months (range: 0- 135 months). The average incidence was 62.32 per 100,000 TKA. PT was repaired with anchors (A) in 9 (4 with a graft) and trans-osseous tunnels (TO) in 12 (5 required graft), and 5 with other methods. There was a significant improvement in KSS from 61 to 83 (P=0.023). There was a significant difference in time from PT tear to surgery in patients with grafts (42 days) and those without grafts (6 days) (P<0.001). Compared to A repair, TO had 2.39 times odds of re-tear (95% CI: 0.38,15.4; P=0.354) and 1.37 times odds of infection (95% CI:0.074,25.6; P=0.83). Repairs with a graft had a 1.90 times odds of re-tear (95% CI: 0.29, 12.19; P=0.49) and 6.3 time odds of infection (95% CI 0.26, 166.7; P=0.25).
Conclusion:
Surgical repair of PT tears following TKA leads to significant clinical improvement, regardless of the fixation method or graft use. We found no difference in outcomes between A and TO repairs and or with graft use.
1. INTRODUCTION
Patella Tendon (PT) rupture is a rare complication following Total Knee Arthroplasty (TKA) and is estimated to occur in 0.17-1.0% of patients [1-3]. Most of these injuries are a result of avulsion from the tibial tubercle insertion, with a minority being mid-substance or infra-patellar avulsions [2]. This complication is thought to be due to compromised blood supply to the extensor mechanism that occurs during TKA [4]. Studies exploring outcomes of patellar tendon rupture repair have shown mixed results [1, 2, 5, 6]. Presently, the two main repair types include suture anchors (A) and transosseous (TO) repairs and both can be augmented by an allograft in the setting of poor tissue quality. Due to the low incidence of this complication, it is still not known which technique is superior. The purpose of this study is to compare the outcomes and complications of these techniques.
2. MATERIALS AND METHODS
After obtaining approval from our Institutional Review Board, we searched through surgical database for patellar repair surgeries performed between January 1, 2008, and December 31, 2016. Our integrated health care system includes 14 medical centers with over 100 orthopaedic surgeons. Our system does not catalogue surgical cases by CPT codes, rather by interfacility codes. We, therefore, searched for “patellar tendon repair” and “open repair of tendon, knee” in our database to identify patients who had undergone a patellar tendon repair. A retrospective chart review was then performed to identify those patients who had a prior total knee arthroplasty (TKA) who underwent surgical repair of a patellar tendon tear. The operative reports, progress reports, history and physical examination, physical therapy notes, and emergency room notes were reviewed and relevant data were collected.
Data gathered included age, gender, side of surgery, BMI, length of time between TKA and patellar tendon rupture (months). In addition, pre- and post-operative Knee Society Scores (KSS) [7, 8], and range of motion including extensor lag were also recorded. We were unable to collect pre-operative KSS for 10 patients and post-operative KSS were only used for patients with a minimum of 3 months post-PT repair, leaving 12 patients with both scores.
The information recorded from the operative report included tourniquet time, repair type, patellar thickness after resection (mm) (measured using the internal digital software (Philips iSite Radiology, Version 3.6.120), patellar polyethylene thickness (mm), implant manufacturer, and use of auto- or allograft. Complications such as re-rupture, infection, and thromboembolic events were also recorded.
Means and medians of continuous variables were compared using t-tests and Kruskal-Wallis tests as deemed appropriate. Unadjusted odd ratios were calculated using logistic regression. All P values were 2-sided with an alpha = 0.05. Statistical analyses were performed with SAS 9.3 (SAS Institute, Cary, NC).
3. RESULTS
3.1. Patient Demographics
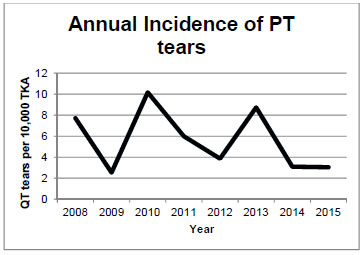
Four hundred PT repairs were identified during our database search and from this, 26 patients were identified who sustained a PT disruption after a TKA. During our study period, 41,722 total knee arthroplasties were performed in our institution. The average incidence was 62.32 per 100,000 TKA. The average annual incidence of PT tears with TKA can be seen in Fig. (1).
The average age at the time of surgery was 69.7 years (range, 53 to 88) and there were 19 females (73.1%). Seventeen patients were Caucasian, three Asian, three Hispanic, and two African American. Twenty-five patients underwent a TKA for osteoarthritis and one patient for posttraumatic degenerative reasons. The average time between TKA to PT tear was 13.6 months (range 0 to 135 months). Patients with predisposing factors included fourteen taking statins, six with diabetes, and one with stage three chronic kidney disease (Table 1).
| Age | Gender | Mechanism of Injury | Time from Injury to Surgery (days) | Prosthesis | Notes |
|---|---|---|---|---|---|
| 59 | F | Fall | 0 | Zimmer Natural Knee | Diabetic, Taking statins, had re-tear |
| 88 | M | Progressive | 18 | J&J Depuy Sigma | Had re-tear |
| 67 | F | Fall | 25 | J&J Depuy Sigma | - |
| 80 | F | Fall | 31 | J&J Depuy Sigma | Had re-tear |
| 57 | F | During TKA | 0 | Zimmer Natural Knee (Revision) | Had infection |
| 81 | F | Fall | 16 | J&J Depuy Sigma (Revision) | Taking statins |
| 64 | F | Spontaneous | 117 | Zimmer Natural Knee (Revision) | Taking statins, had re-tear, had DVT |
| 81 | M | Getting up from sitting | 65 | Zimmer Natural Knee | Taking statins |
| 53 | F | Fall | 21 | J&J Depuy Sigma (Revision) | Diabetic, Taking statins |
| 83 | F | Spontaneous | 15 | J&J Depuy Sigma | Taking statins, had infection |
| 65 | F | Getting up from sitting | 13 | Zimmer Natural Knee | Had e-tear |
| 80 | F | Fall | 0 | Zimmer Natural Knee | Stage 3 CKD |
| 67 | F | Getting up from sitting | 1 | Zimmer Natural Knee | Diabetic, Taking statins |
| 60 | F | Fall | 23 | Zimmer Natural Knee | Taking statins |
| 86 | M | Spontaneous | 6 | J&J Depuy Sigma | Diabetic, Taking statins |
| 75 | F | Getting up from sitting | 2 | Zimmer Natural Knee | Taking statins |
| 64 | F | Fall | 41 | J&J Depuy Sigma | Diabetic, Taking statins, had DVT |
| 53 | F | Progressive | n/a | J&J Depuy Sigma | Taking statins |
| 53 | M | Fall | n/a | J&J Depuy Sigma | Had infection |
| 68 | F | During TKA | 112 | J&J Depuy Sigma | Had re-tear, Had infection |
| 78 | M | Playing sports | 43 | J&J Depuy Sigma | Had re-tear |
| 62 | F | Fall | 7 | J&J Depuy Sigma | - |
| 65 | F | Fall | 6 | Smith & Nephew Genesis II | - |
| 83 | M | Spontaneous | 0 | Unknown | - |
| 60 | M | Walking | 1 | J&J Depuy Sigma | Diabetic, Taking statins |
| 80 | F | Progressive | 21 | J&J Depuy Sigma (Revision) | Taking statins |
Eleven injuries occurred due to a fall, four from getting up from a seated position, four were progressive, three had a spontaneous or unknown cause, two during TKA surgery, one occurred while playing sports, and one occurred while walking. Twenty disruptions occurred following primary total knee arthroplasty, five after a revision total knee arthroplasty, and one during a primary TKA. The average time between surgery and tear was 0.8 months (range, 0 to 3.9 months).
3.2. Surgical Findings
Twenty-one patients had complete tears and five had partial tears. Of the complete tears, eleven were avulsions off the tubercle, five from the patella, four were midsubstance tears, and one was a midsubstance and patella combined tear. Of the five partial tears, three were midsubstance tears and two from the tubercle (Table 2). Five patients underwent concomitant operations; two patients had a polyethylene liner exchange, one had a contralateral TKA, one had a knee arthroscopy revision, and one had a revision of the femoral component.
Twenty-one PT ruptures were repaired by two main methods, suture anchor (A)(N=9) and transosseous (TO)(N=12) repair with allografts being used in four and five patients respectively. The types of allografts used are listed in Table 2. The remaining 5 patients underwent other types of surgeries detailed in Table 2.
| Age | Gender | Partial/ Complete tear |
Location of Tear | Type of Repair | Retear | Notes |
|---|---|---|---|---|---|---|
| 59 | F | Complete | Tibial Tubercle | Suture Anchor | Y | - |
| 88 | M | Complete | Tibial Tubercle | Suture Anchor | Y | - |
| 67 | F | Complete | Tibial Tubercle | Suture Anchor | N | - |
| 80 | F | Complete | Inferior pole of Patella | Suture Anchor | Y | - |
| 57 | F | Complete | Tibial Tubercle | Suture Anchor | N | Concomitant Knee arthroscopy revision |
| 81 | F | Complete | Tibial Tubercle | Suture Anchor | N | - |
| 64 | F | Complete | Tibial Tubercle | Suture Anchor | Y | Polyethylene liner exchange |
| 81 | M | Partial | Tibial Tubercle | Suture Anchor | N | - |
| 53 | F | Complete | Tibial Tubercle | Suture Anchor | N | - |
| 83 | F | Complete | Inferior pole of Patella | Transosseous | N | - |
| 65 | F | Complete | Midsubstance and patella combined tear | Transosseous | Y | - |
| 80 | F | Complete | Inferior pole of Patella | Transosseous | N | - |
| 67 | F | Partial | Midsubstance | Transosseous | N | - |
| 60 | F | Partial | Midsubstance | Transosseous | N | Revision of femoral component |
| 86 | M | Complete | Inferior pole of Patella | Transosseous | Y | - |
| 75 | F | Complete | Midsubstance | Transosseous | N | Polyethylene exchange |
| 64 | F | Complete | Inferior pole of Patella | Transosseous | Y | - |
| 53 | F | Complete | Tibial Tubercle | Transosseous | N | Ipsilateral TKA |
| 53 | M | Complete | Tibial Tubercle | Transosseous | N | - |
| 68 | F | Complete | Tibial Tubercle | Transosseous | N | - |
| 78 | M | Complete | Midsubstance | Transosseous | N | - |
| 62 | F | Partial | Midsubstance | End to End | N | - |
| 65 | F | Complete | Tibial Tubercle | End to End | N | - |
| 83 | M | Partial | Midsubstance | End to End | N | - |
| 60 | M | Complete | Midsubstance | End to End | Y | - |
| 80 | F | Complete | Tibial Tubercle | Repaired with polypropylene mesh | N | - |
3.3. Implant Characteristics
In the 26 patients, 14 Sigma (Johnson and Johnson, Warsaw, IN), 10 Natural Knee (Zimmer, Warsaw, IN), 1 Genesis II (Smith and Nephew, London, UK), and 1 unknown system were implanted during the TKA. Following the procedure, the average patella thickness was 17.3mm (range, 14.3-22.4mm).
3.4. Clinical Findings
There was a significant difference in time from PT tear to surgery in patients with grafts (42 days) and those without grafts (6 days) (p<0.001). Overall, there was a significant improvement of KSS from 61 to 83 (p=0.023) after PT repair surgery. There was no difference between A and TO in pre- (p=0.38) and post- (p=0.78) operative KSS scores (TO=20 +21.6, A=15.3+15.3), post-op extension lag (TO=9.8+10.82, A=10.1+10.82, p=0.91) or ROM (TO=9.69+7.69, A=10.22 +7.69, p=0.98). In the A group, there was no difference in pre and post KSS (15.3+14.6, p=0.054) nor in the TO group (20.3+20.6, p=0.06). There was no difference in post-op KSS in graft vs. no graft (20.1+17.6, p=0.46) or extensor lag (45.6+34.2, p=0.72). Five of the TO patients had extensor lags greater than or equal to 30 degrees as compared to just one in the A cohort. The average postoperative flexion for the TO group was 111 degrees (range, 90-120 degrees) and 109 degrees for the A group (range, 70-125), with nine of the twenty-one patients being able to flex their knee 120 degrees or greater.
There were 2 (7.69%) deep vein thromboses and 4 infections (15.38%). Eight patients had re-tears, 4 in the SA group (3 non-allografts, 1 non-allografts), 3 in the TO group (2 non-allograft, 1 allograft) and one in the other group. Compared to A repair, TO repair had 2.39 times odds of re-tear (95% CI: 0.38,15.4; p=0.354), 1.37 times odds of infection (95% CI:0.074,25.6; p=0.83). Compared to repairs without a graft, graft repairs had 1.90 times odds of re-tear (95% CI: 0.29, 12.19; p=0.49) and 6.3 times odds of infection (95% CI 0.26, 166.7; p=0.25).
4. DISCUSSION
The results of this study show that patellar tendon repair following a TKA can cause significant improvement to functional outcomes of patients. Furthermore, there was no significant difference between functional outcomes, ROM, or post-op extension lags when comparing the SA group to the TO group or in patients who received a graft versus those who did not receive a graft. There was, however, a significant difference in time from PT tear to surgery in patients with and without grafts, with grafts more often being used in patients who had longer duration between injury and treatment.
The current gold standard for direct repair is with trans-osseous drill holes in the patella, but suture anchors have gained popularity [1, 3, 6]. Augmentation techniques for patients with poor tissue quality have also been described [3, 9]. Augmentations usually involve hamstring autograft, fresh-frozen or freeze-dried Achilles tendon with a bone block, extensor mechanism allograft, or synthetic meshes [2, 9]. These recommendations are consistent with our findings of non-allograft techniques performed on an average of 6 days following injury versus allografts being used in surgeries performed on an average of 42 days post-injury.
Although functional outcomes as a whole improved for patients following the intervention, PT repair continues to have high rates of complications consistent with the current literature. A study by Rand et al. [1] reported on the results of patellar tendon repair following TKA found that 10 out of 18 attempted repairs sustained a re-rupture (55.5%). The re-tear rate reported in our study (30.8%), although high, was lower as compared to the findings in the study reported by Rand et al. [1]. This is likely due to improvements in surgical technology and techniques over the past three decades. Conversely, the mean extensor lag in patients with successful and unsuccessful repairs was similar (-1 and -22 degrees in Rand et al. [1] respectively, compared to -7 and -20 respectively in our study). Schoderbek et al. [2] compared pre and post-op KSS scores among patients who had evidence of an extensor mechanism injury who underwent a revision TKA. They found that there was a significant improvement in the KSS score, but improvements still lagged behind patients who had no extensor mechanism injury prior to TKA revision [2]. This supports our conclusion that surgery can improve functional outcomes in patients with patellar tendon injuries following TKA, but that the results remain inferior to patients without patellar tendon disruptions. Our study reports an infection rate of 15.38% and DVT findings in 7.69% of patients, which is much higher than primary TKA surgery [10]. Furthermore, the failure rate of 30.8%, while lower than other studies, remains high [1, 5]. Eleven of the 26 patients in this study continued to have an extensor lag following surgery, indicating high levels of residual deficits.
Overall, this paper has shown some improvement as compared to past studies, but the outcomes nevertheless remain poor. More research is needed to assess differences in outcomes between transosseous versus suture anchor repair and augmentation versus no augmentation.
Our study has several limitations. The small number of patients that qualified for inclusion limits significant conclusions, and even more so once they were separated into the TO and A groups. Furthermore, due to the variable nature of patellar tendon injury presentations and surgeon dependent repairs, outcomes may be difficult to reproduce. Outcomes of patellar tendon repairs following TKA have steadily improved though overall success has remained low.
CONCLUSION
In conclusion, surgical repair of PT tears following TKA leads to significant clinical improvement, regardless of the fixation method or graft use. We found no difference in outcomes between A and TO repairs and or with graft use.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the ethics committee of Tulane School of Medicine, USA.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


