All published articles of this journal are available on ScienceDirect.
Intra-Operative 3-Dimensional Imaging (O-arm) in Foot and Ankle Trauma Surgery: Report of 2 Cases and Review of the Literature
Abstract
Background:
Intraoperative two-dimensional (2D) fluoroscopy is the standard imaging modality available to orthopaedic surgeons worldwide. It is well-accepted, however, multiplanar 3 dimensional (3D) CT scanning is superior to 2D imaging for visualising joint surfaces and is now a fundamental feature of the pre-operative planning of intra-articular fractures.
Objective:
We present two cases in which the use of 3D intraoperative imaging and the O-arm® (Medtronic, Minneapolis, USA) led to immediate intraoperative revision to optimise fixation and articular congruity. A review of the current literature is also provided.
Methods:
During the trial period of the O-arm at our major trauma centre, intra-operative imaging was used in the lower limb trauma setting. The O-arm was used intra-operatively in a comminuted pilon fracture and a displaced talus fracture. We recorded all the intra-operative events, including quality of reduction, implant positioning and operation time. Each patient was followed-up for 12 months post-operation and was finally assessed with x-rays and the AOFAS score.
Results:
In both the cases, either fracture reduction or the implant position/usage that was observed with 2D fluoroscopy was revised following a 3D intra-operative scan. No postoperative complications were noted and the healing process was uneventful. X-rays at the final follow-up were excellent and acceptable for the talus and pilon fracture, respectively, with corresponding clinical results and AOFAS score.
Conclusion:
Although frequently used in spinal surgery, to the best of our knowledge, the use of intra-operative 3D techniques in lower limb trauma is sparse and sporadically reported. We present our cases in which the most current innovative imaging techniques influenced intra-operative outcomes without compromising patient safety. We feel that this is a real example of how innovation can positively influence patient care.
1. INTRODUCTION
A fundamental concept in the surgical treatment of intra-articular fractures is that anatomic reduction is paramount to restoring mobility and optimising function. Certainly, in ankle fractures, anatomical alignment post injury has been shown to be critical in restoring contact areas and pressures and preventing post-traumatic arthritis [1-5]. In cadaveric studies, as little as 1 mm lateral translation led to a 42% decrease in the tibiotalar contact area and abnormal stresses across the joint [6]. More recent studies have correlated postoperative ankle articular incongruity with statistically poor foot and ankle outcome scores and poorer early ankle functional outcomes [7]. Despite evidence supporting the importance of articular reduction and congruency, there is little in the literature analysing how we as orthopaedic surgeons assess articular congruity, particularly in the intra-operative setting. It is during surgery that, ultimately, the critical decision-making process occurs and after which the opportunity no longer exists to optimise articular reduction.
Computed tomography scanning is a gold standard in pre-operative imaging and planning of complex intra-articular fractures [8-10]. In fact, evidence suggests that plain radiographs are unreliable in the assessment of fracture patterns, particularly in fractures involving the foot and ankle [11-14]. In a study, nearly a quarter of all the pre-operative plans based on plain radiographs were changed following the review of the CT [15]. Therefore, it is somewhat surprising that at the time when accurate imaging is vital and can be the most influential, namely the intra-operative setting, we rely on the suboptimal imaging modality of fluoroscopy. When the surgeon is unable to completely visualize the fractured surface intra-operatively, post-operative CT scans may be necessary. If an unsatisfactory reduction or intra-articular hardware penetration is present, revision is often required, necessitating a second procedure.
Fluoroscopy itself has been shown to be less accurate compared with plain radiographs [16]. Recent evidence suggests that both intra-operative fluoroscopy and post-operative radiographs are unreliable in assessing articular congruity, with low reliability and sensitivity [17]. However, the ongoing use of fluoroscopy reflects a relatively inexpensive modality that is easily available and has minimal impact on operative time. Intra-operative cone-beam CT (O-arm®, Medtronic, Minneapolis, USA) can provide the answer to improved intra-operative real-time imaging without having a significant impact on operative time. The greatest application of this technology has been within spinal surgery where the O-arm has been paired with Stealth Navigation for accurate placement of pedicle screws in spinal stabilisation; this has resulted in lower complication rates especially in those with atypical anatomy [18-22]. We present 2 cases in which the option to use intra-operative O-arm scanning influenced intra-operative management. In addition, we present a review of the relevant literature on O-arm use in lower limb trauma.
2. METHODS - RESULTS
This study was performed at the Royal London Hospital Major Trauma Centre, UK and the patients were recruited prospectively. In February 2018, an O-arm scanner was available as part of the Spinal Surgery Unit under trial along with its associated navigation system for pedicle screw placement. When the unit was not in use by our colleagues in spinal surgery, we were able to use it in the trauma setting. The O-arm was used in two lower limb trauma cases. The first was a 42-year-old gentleman with a pilon fracture following a road traffic accident, and the second was a 24-year-old female with a talus fracture following a fall from height. All the intra-operative events were recorded and the exact duration of time needed to obtain the O-arm images was noted. Both the patients were followed up for 12 months.
2.1. Case 1: The Pilon Fracture
The first case was of a 42-year-old, strong and healthy architect and keen ultra-marathon runner who was involved in a motorbike versus car road accident. He was knocked off his motorbike whilst travelling at approximately 40 miles per hour and although he was wearing riding boots, he sustained an isolated injury to his right ankle. He described immediate gross deformity and severe pain. He was brought to the Accident and Emergency Department by an ambulance and an assessment was conducted as per the Advanced Trauma & Life Support protocols. His ankle injury was imaged with plain radiographs as shown in Figs. (1A & B). This was an isolated, closed injury and the limb was neurovascularly intact on presentation. There was gross swelling and deformity, with extensive ecchymosis. The patient had no previous medical history of note, no regular medications and was an independent non-smoker who was an ultra-marathon runner. Multiple unsuccessful attempts at reduction were attempted in the Accident and Emergency department under conscious sedation (Figs. 1C & D).
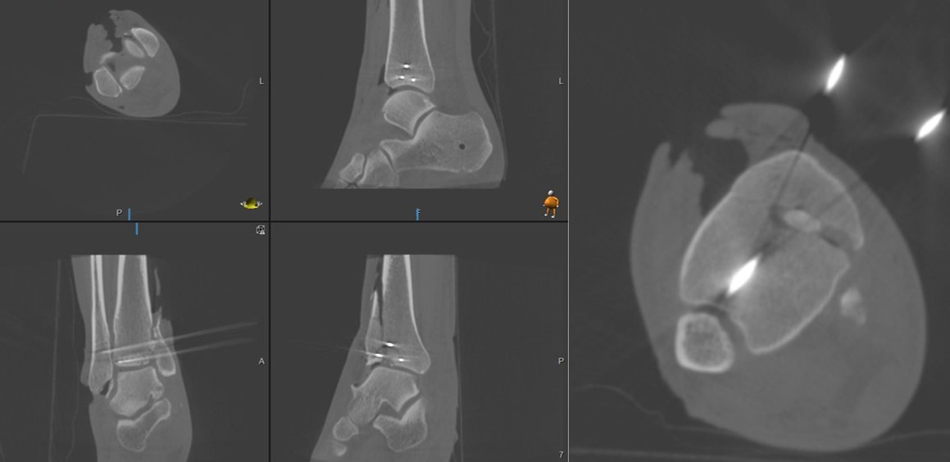
The patient was taken to the operating theatre emergently and under a general anaesthetic, a closed reduction was achieved under intra-operative radiological guidance and an ankle spanning external fixator was applied in a standard delta frame configuration. (Figs. 1E & F). A post-frame CT scan was obtained and demonstrated a highly comminuted tibial plafond fracture with cartilage loss and a bony avulsion of the fibular insertion of the anterior talofibular ligament (Fig. 2). Due to extensive swelling and fracture blistering, the patient was made to rest, and the foot was treated with ice and elevation for a period of 7 days until the soft tissues were deemed suitable to undergo further surgery. The definitive procedure was performed under general anaesthetic with the patient in supine position and with a tourniquet positioned on the right thigh. Following extensive pre-operative planning, the decision was taken to retain part of the frame construct to maintain fracture reduction and length restoration. An anterior approach to the distal tibia was utilised, curved anteromedially at its proximal extent. The vertical fracture site was opened and the comminuted fragments were removed from the fracture site. The depressed plafond fragments were reduced under direct vision and the anterior cortex was reduced anatomically, as it was not comminuted. The reduction was provisionally maintained with pointed forceps and three 1.25 mm Kirschner wires, which could be later used for 3.5 mm fully threaded cannulated screws. Once the fracture was provisionally stabilised, radiographs were obtained and although they appeared to show a satisfactory reduction on lateral views, anteroposterior views showed a malreduction (Fig. 3). The question at this stage was whether to perform a second incision posteriorly and switch to a dual approach. The O-arm was used to acquire intra-operative multiplanar images to identify issues with the reduction (Fig. 4). It could be clearly seen that a fracture fragment remained incarcerated within the vertical shear fracture, preventing reduction. This fragment was not seen under direct vision due to its impaction into adjacent cancellous bone. Following O-arm image acquisition, the surgical team was able to re-explore the fracture site through the existing anterior approach, identify and remove the incar



2.2. Case 2: The Talus Fracture
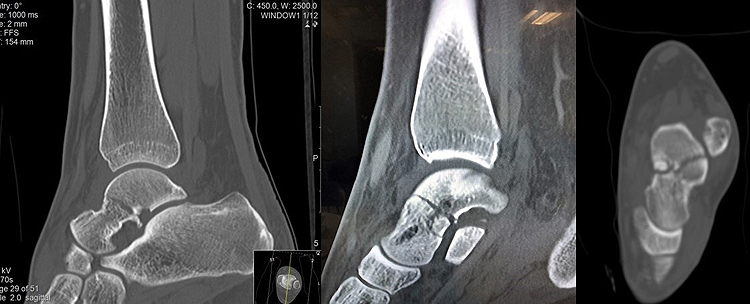
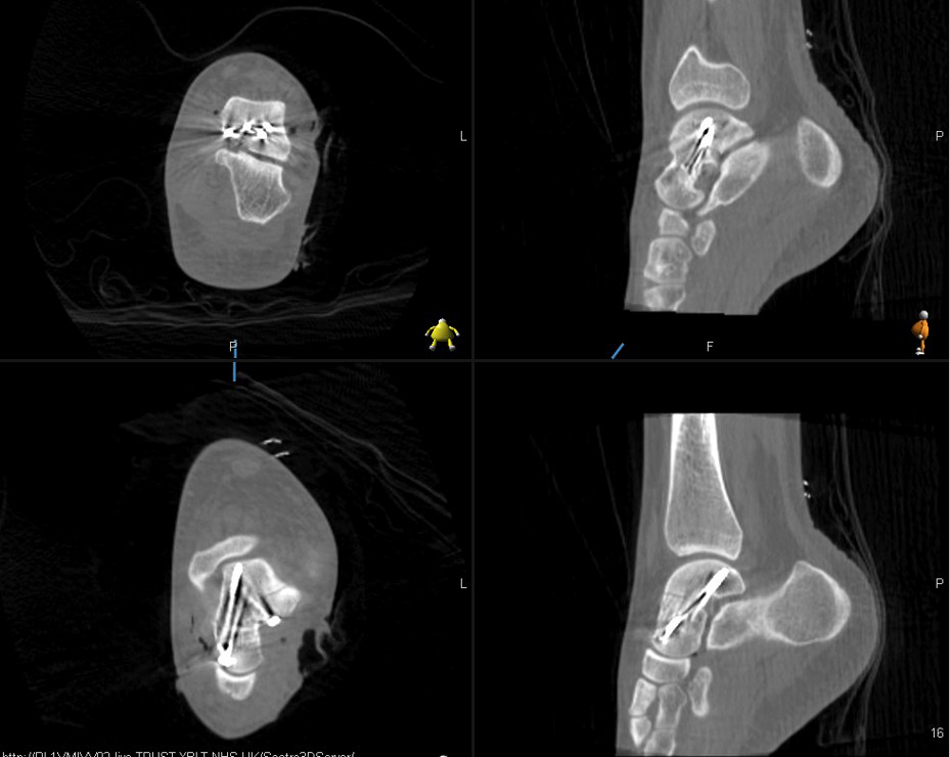
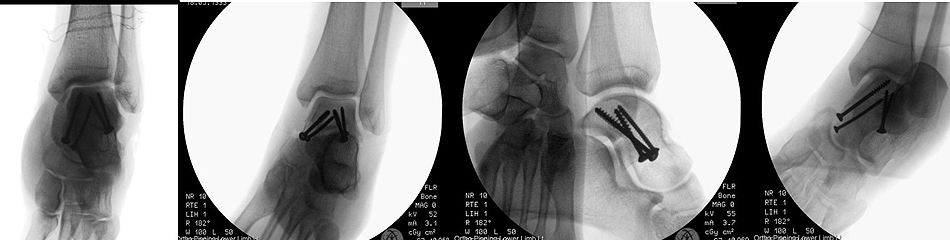
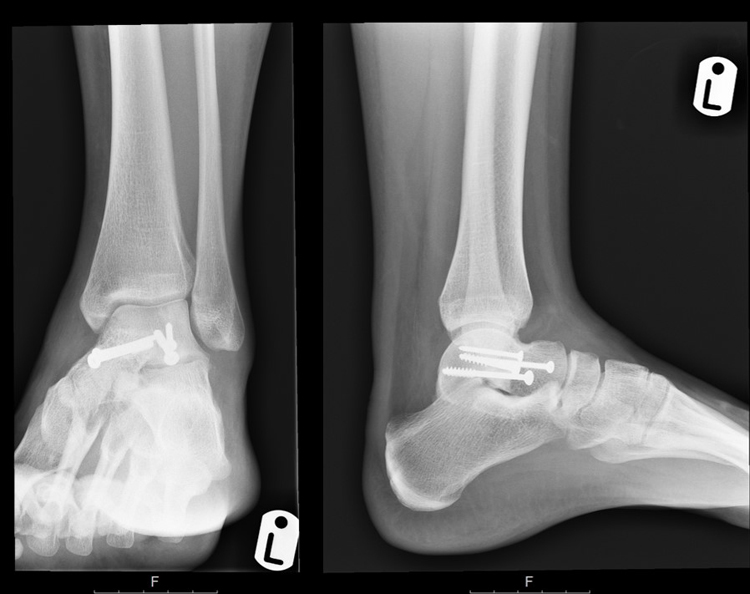
The second case was of a 24-year-old strong and healthy female office worker who fell approximately 2 metres off an indoor climbing wall. She described her left forefoot hitting the wall as she fell and a hyper-dorsiflexed position of the left ankle when landing. She experienced immediate pain and swelling and was unable to bear weight. She was brought into the accident emergency by ambulance and on presentation, had an isolated, closed injury and she was neurovascularly intact. She had no medical history of note, no regular medications and was an otherwise fit and healthy, non-smoking individual. She underwent initial investigation with plain radiographs of the left ankle and a subsequent CT scan at the accident and emergency department. Sagittal images from the CT scan showed a left talar body fracture with medial comminution and a loose articular fragment impacted in the fracture site. There was a subtle varus malalignment of the longitudinal axis of the injured talus due to the medial comminution and medial collapse (Fig. 7). The patient was operated on the 7th day post-injury, during which time the limb was rested, iced and elevated to manage soft tissue swelling. The pre-operative plan involved a standard dual incision technique to ensure anatomical reduction and correction of the varus malalignment. The patient was in the supine position, with a thigh tourniquet inflated and a bump under the left buttock, which was removed when addressing the medial side. An initial lateral approach to the talus was utilised through which the fracture site was accessed and cleared of interposing fracture fragments. The lateral side of the fracture was then reduced and provisionally held with 1.25 mm K-wires; a 4 mm partially threaded cannulated screw was inserted through the incision from the lateral talar process into the talar body. Given the excellent reduction in intra-operative radiographs, the decision taken was to further place a identical wire percutaneously, dorsomedial from the talar head into the talar body. The O-arm was then used to give multiplanar images of the fracture reduction. This showed an anatomical fracture reduction and restoration of the long axis of the talus. Based on these images, the decision was taken to fix the medial side percutaneously avoiding a more extensive approach and dissection medially. Following the O-arm images, two 4 mm partially threaded cannulated screws were inserted over the guide wires and tightened sequentially to achieve compression at the fracture site. One fully 3.5mm cortical screw was inserted adjacent and parallel to each one of the partially threaded screws to augment the fixation. The lateral one was inserted through the incision, and the medial one through a stab incision dorsomedially distal to the talar head. A final O-arm image sequence was acquired to ensure the maintenance of reduction and no prominence of metal work (Fig. 8). Final intra-operative radiographs are shown in Fig. (9). Each image acquisition with the O-arm took under 4 minutes. The limb was placed in a below knee splint in neutral ankle position, which was changed to a full below knee cast two weeks later after the swelling had subsided completely and the wound was dry and healthy. The patient remained immobilized and non-weight bearing for 6 weeks postoperatively. She remained non-weight bearing in a boot that allowed ankle range of motion exercises for an additional six weeks. The fracture healed uneventfully without early signs of arthritis or avascular necrosis at one-year post-operative (Fig. 10) and she had an AOFAS score of 95.


3. DISCUSSION
As a part of meticulous pre-operative planning protocols, orthopaedic surgeons often spend significant time scrolling through pre-operative imaging, delineating fracture patterns, identifying individual fracture fragments and carefully outlining an operative strategy for the fixation of intraarticular fractures. A pre-operative CT scan is the gold standard modality in this planning phase. With this in mind, it is bizarre that at the point of the execution of the said plan, where accuracy is essential during surgery, we rely on an inaccurate imaging modality because of convenience and availability. Fluoroscopy has been shown to be less accurate compared to plain radiographs. In fact, neither fluoroscopy nor plain radiography is reliable or sensitive in assessing articular congruity [14, 15]. Garner et al. [16] found 21% sensitivities for fluoroscopy and 36% sensitivities for plain radiographs and deemed these unacceptable for modalities that are considered to be the standard of care worldwide. Based on these numbers, they found that only 21%-36% of patients with articular incongruency were actually identified using fluoroscopy or plain radiographs. Furthermore, neither imaging modality was found to have better than moderate intraobserver or interobserver reliability, indicating that the assessment of articular reduction varies significantly between practitioners.
The O-arm offers an intra-operative cone beam CT scan with high quality, linked multiplanar images that can be actively scrolled, as well as 3D reconstructed images. There is literature on the previous attempts at 3D imaging in trauma, primarily using the Siemens ISO-C3D™ system (Siemens, Erlangen, Germany). However, this system and similar ones are actually an extension of fluoroscopy and are based on multiple plane x-rays. These fluoroscopic systems had several disadvantages: a higher dose of radiation, small field of view, low quality and a spin range of 190 degrees with the remaining arc being a fabricated image [23]. All of these factors affected the ultimate functionality of the ISO-C3D system. That said, it still proved to be superior to simple fluoroscopy and certainly eluded the potential benefits of intra-operative cone beam CT scanning.
Previous authors have published studies on the use of the Siemens ISO-C3D fluoroscopic system. Moon et al. [21] used it in the surgical treatment of 109 fractures in 101 patients, including upper and lower limb fractures as well as pelvic and acetabular fractures. They found an overall intra-operative revision rate of 9.2%, with a sub-analysis showing the highest revision rate for injury type such as for syndesmotic injury, with a revision rate of 23.1%. Kendoff et al. [22] used the system in 248 consecutive patients with intraarticular fractures. In 19% of all cases, intraoperative image analysis resulted in the immediate adjustment of the reduction or hardware exchange. These revisions were said to be based on Iso-C3D views of the articular surface that were not visible using fluoroscopy. Richter et al. [24] analysed a series of 62 fractures, most of which were in the hindfoot and midfoot. They found an intra-operative revision rate of 39%, similar to the 40.3% revision rate observed in 377 calcaneal fracture fixations by Franke et al. [25]. It is clear that even the fluoroscopic based systems highlighted the benefits of multiplanar intra-operative imaging.
The literature specifically regarding the use of O-arm in foot and ankle trauma is sparse. Hsu et al. [26] published a case report in which the O-arm was used in confirming the cannulated screw guide wire position in a delayed presentation navicular stress fracture. The same authors published a case report describing the use of the O-arm in the evaluation of syndesmosis reduction in a Maisonneuve fracture of the ankle [27]. Eckardt and Lind [28] retrospectively evaluated 62 patients with calcaneal fractures who underwent provisional ORIF under standard fluoroscopy, followed by the O-arm 3-D CT before definitive fixation to assess if reduction was satisfactory. The 3-D CT evaluation showed an intraoperative revision rate of 40%. Finally, Chowdhary et al. [29] utilised the intra-operative O-arm in 33 acute fractures and summarised the benefits such as a reduction in intraoperative complications and minimising the need for secondary procedures.
The acquisition of a complete O-arm image took under 4 minutes in each of the cases. This did not extend the length of surgery significantly and represented 4% and 3.5% of the total operative time for case 1 and case 2, respectively. The extra information gained from one O-arm spin must not be underestimated and is significantly greater than multiple c-arm images. In terms of radiation dose, a single complete O-arm spin has been noted to emit 7.9mGy, equivalent to 5.6 standard radiographs [27]. An intraoperative O-arm scan replaces the need for a post-operative assessment CT scan, sparing the patient radiation and reducing overall cost. Eckardt and Lind [28] showed that intraoperative radiation exposure with the O-arm during foot surgery was less than that with a conventional CT scan of the foot postoperatively.
CONCLUSION
Our early experience with the O-arm was encouraging and showed great potential. In both the cases, the O-arm images contributed to an intra-operative change in articular reduction that would otherwise have been accepted based on satisfactory fluoroscopy views. It also enabled more minimally invasive approaches to be used without compromising articular congruity and anatomic restoration. Further research will focus on the collection of patients’ reported outcome measures to show the benefit of more accurate intra-operative imaging in the reconstruction of complex articular fractures. Regardless, with the current evidence, it is clear that intra-operative CT scanning holds significant advantages over our current gold standard of 2D fluoroscopy.
ABBREVIATION
| AOFAS | American Orthopaedic Foot & Ankle Society |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Both the patients gave informed consent for participation in the study, as well as for the publication of their medical history and radiographs in medical journals.
FUNDING
The authors declare that there was no funding or writing assistance.
CONFLICT OF INTEREST
The authors declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


