All published articles of this journal are available on ScienceDirect.
Suprascapular Neuropathy in Overhead Athletes: A Systematic Review of Aetiology and Treatment Options
Abstract
Suprascapular neuropathy is often overlooked as a cause for shoulder pain in overhead athletes and can be misdiagnosed for many months, even years. With recent advancements in the understanding of the condition as well as its treatment methods, suprascapular neuropathy is now being diagnosed more frequently. However with a multitude of treatment options, it can be difficult to choose the optimal management. In this systematic review, we have carried out a detailed literature search about suprascapular neuropathy looking into evidence-based diagnostic workup and treatment modalities available. Repetitive overhead activities, rotator cuff tear and direct compression of the nerve by space-occupying lesion are important etiologies for suprascapular neuropathy. Whilst MRI is widely used for the identification of space-occupying lesions and rotator cuff injury; Electromyography (EMG) and Nerve Conduction Studies (NCS) remain gold standards for confirming injury to the nerve. Conservative treatment modalities including physiotherapy and activity modification, nerve blocks, arthroscopic and open surgical interventions are the main treatment options for suprascapular neuropathy.
1. INTRODUCTION AND BACKGROUND
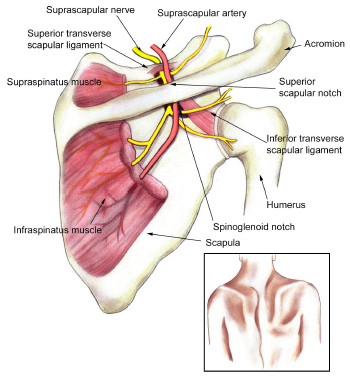
The posterosuperior aspect of the shoulder receives its sensory innervation from the suprascapular nerve. The supr- ascapular nerve also provides motor innervation to supras- pinatus and infraspinatus muscles Fig. (1). Compression or traction of nerve and rotator cuff diseases are found to be associated with suprascapular nerve damage and neuropathy. Clinical symptoms of the condition include pain in the posterior shoulder and weak forward flexion and external rotation. It is also noteworthy that the multiple presentations of suprascapular nerve neuropathy vary greatly in different patients, and thus the diagnosis of the condition is often challenging. This kind of nerve damage is a less common reason for shoulder pain and dysfunction in the general population. However, it is widely observed in athletes who play overhead sports such as volleyball, tennis, badminton and baseball. Such sports expose the athlete’s hands to overhead, abducted and externally rotated positions for prolonged periods of time [1, 2].
Observational studies have identified that players involved in overhead sports are at higher risk of injuries related to over use of the shoulder such as rotator cuff tendinopathy and tearing of glenoid labrum [3]. On the other hand, shoulder pain due to suprascapular neuropathy is observed in only 1-2% of cases and therefore, the condition is often overlooked during diagnosis for shoulder pain. Among the overhead sports athletes, the incidence of suprascapular neuropathy is maximal in volleyball players. Around 33% of volleyball players suffer from this condition at some instance in their career [4].
Traditionally, suprascapular neuropathy has always been regarded as a diagnosis of exclusion. However, now with further understanding of the aetiology and advanced diagnostic options, the condition is being recognised by physicians from an earlier onset.
2. AETIOLOGY OF SUPRASCAPULAR NEUROPATHY
Rotator cuff tear is considered as a prime cause of suprascapular neuropathy. Studies show that suprascapular neuropathy can also develop secondary to traction and micro- trauma, especially in overhead athletes, particularly due to tightening of the spinoglenoid ligament during the overhead throwing position. The risk for the development of supras- capular neuropathy also increases in patients with ossification of the transverse scapular ligament or spinoglenoid ligament. Other causes such as; compression of the nerve at spinoglenoid notch due to the presence of a bone tumor and cyst due to labral tears or capsular injury can also lead to the condition. Suprascapular neuropathy is also rarely seen following brachial neuritis, glenohumeral dislocation, fracture of the shoulder girdle and penetrating or iatrogenic injury to the nerve [5].
All these aetiological factors for suprascapular neuropathy are discussed in detail in the following sections.
2.1. Rotator Cuff Injury
From Plancher’s anatomic studies, we know that the spinoglenoid ligament is present in all patients. Although there is some variation in the size and thickness of the ligament between men and women, there is no significant difference between the linear space for suprascapular nerve to pass through and the ligament. The inferolateral part of the ligament has superficial and deep layers inserting into the posterior aspect of the shoulder capsule and glenoid neck. The supras- capular nerve and branches of the suprascapular artery and vein pass along the base of the scapular spine. The nerve supplying infraspinatus and the suprascapular artery and vein also pass below the ligament [6].
Injury due to traction or compression of the nerve at any point in this path can lead to suprascapular neuropathy. Retracted superior or posterior rotator cuff tear is the most common cause for suprascapular nerve traction injury. Tension on the suprascapular nerve lying at the suprascapular notch or spinoglenoid notch increases with the retraction of supras- pinatus and infraspinatus tendons. Studies on cadavers by Gosk et al showed that as the retraction of supraspinatus tendon increases, it reduces the angle between the suprascapular nerve and its first motor branch, which leads to an increase in tension and thus causes traction injury. They also found that massive rotator cuff tear was the main reason for suprascapular neuro- pathy in eight different overhead players [7]. On the other hand, comparative studies by Lajtai et al found that rotator cuff tear and muscle atrophy were responsible for only 8% of suprascapular neuropathy cases [8].
Cadaveric studies have shown that the tension on the neurovascular pedicle increases significantly once the lateral advancement of a retracted rotator cuff tear exceeds 3 cm [9] . Other studies suggest that if the rotator cuff retraction increases by 3 cm, it causes significant tension on the motor branches of the suprascapular nerve. In addition, the tension on the medial portion of the suprascapular nerve starts to increase only by 1 cm extension of the rotator cuff. Increased tension is one of the important reasons for traction injury to the nerve [10].
It has also been reported that following surgical repair of rotator cuff tear, the tendons can be advanced up to 3.5 cm without any significant risk to the health of the suprascapular nerve. Various reports suggest that surgical repair of rotator cuff tear can help in either partially or completely resolving suprascapular neuropathy. Nerve recovery by reinnervation has been found in patients with suprascapular neuropathy follow- ing arthroscopic rotator cuff repair [11].
2.2. Nerve injury: Sports Specific Etiology
Various etiological mechanisms for suprascapular neuro- pathy have been proposed which include repeated traction, microtrauma, ischaemia of the nerve and compression of the nerve by soft tissue, tumor or cyst. However, nerve injury due to repetitive trauma is considered to be the main reason for the development of suprascapular neuropathy [12].
Two main sites for suprascapular nerve injury are: the suprascapular notch and the spinoglenoid notch. The symptoms alongside clinical presentation for suprascapular neuropathy thus depend on the location of nerve injury.
2.3. Aetiology and Causes at the Suprascapular Notch
Suprascapular nerve entrapment is more common at the suprascapular notch under the transverse scapular ligament and is again typically seen in athletes practicing repetitive overhead movements. Physical examination is an essential part of diagnosis and nerve compression at the suprascapular notch is usually due to a more proximal injury and will result in weakness and atrophy of both supraspinatus and infraspinatus, with shoulder pain being a more prominent feature in comparison to entrapment at the spinoglenoid notch. The pain is attributed to the deep sensory fibers usually along the superior aspect of the scapula radiating to the shoulder and exacerbated in particular with adduction of the extended arm [12, 13].
2.4. Aetiology and Causes at the Spinoglenoid Notch
Injury of suprascapular nerve at the spinoglenoid notch has been found to cause isolated atrophy and weakness of the infraspinatus muscle. This condition is also known as infras- pinatus syndrome. A systematic literature review by Lee et al found that suprascapular neuropathy due to infraspinatus syndrome is common in overhead game athletes, particularly volleyball players [14].
Other rarer causes include ganglion cysts which are more common at the spinoglenoid notch. Pain is a less common symptom as the deep sensory fibers to the joint will have exited more proximally. The spinoglenoid ligament lays into the posterior glenohumeral capsule. Observations suggest that the ligament gets stretched and rigid with the abduction and internal rotation of the ipsilateral upper limb across the body. Such action leads to the traction of suprascapular nerve at the spinoglenoid notch [15, 16].
Sandow & Ilic provided another proposal for traumatic injury to the suprascapular nerve. According to them, when the upper limb is abducted and externally rotated, the medial border of the supraspinatus tendon present at the spinoglenoid notch compresses the suprascapular nerve. Repeated upper limb action thus causes trauma to the nerve and injures it [17].
Plancher & Petterson’s recent study supported this mechanism of nerve injury in their research paper. The spinoglenoid ligament is affected by the position of the glenohumeral joint. They found repetitive shoulder movements together with changes in pressure are factors that cause compression on the suprascapular nerve alongside recurrent trauma [18]. Another systematic review by Lee et al found that suprascapular neuropathy due to infraspinatus syndrome is common in overhead game athletes, particularly volleyball players [14].
2.5. The Sling Effect
One important reason for traction injury in volleyball players is the huge amount of motion occurring at the shoulder during throwing action. The role of the scapula in allowing throwing motion as well as other overhead sports activity is now well-researched. It has been observed that the movement of the scapula during protraction and retraction leads to significant trauma of the suprascapular nerve at both the suprascapular and spinoglenoid notches. This phenomenon is known as the ‘sling effect’. The sling effect proposes that certain positioning of the upper limb during overhead activity exposes the suprascapular nerve at the suprascapular notch to a significant amount of sheer stress and thus resulting in injury. Sling effect also suggests that the suprascapular nerve is exposed to high risk of traction injury when it bends around the spine of the scapula at the spinoglenoid notch [19].
Chronic overuse of the shoulder, as well as functional instability, may cause the suprascapular nerve to angle sharply at the spinoglenoid notch, as an adaptive response. This condition is known as ‘SICK scapula’ which is an abbreviation for Scapular protraction, Inferior border prominence, Coracoid tightness, and Kinesis abnormalities of the scapula [20]. While imaging for the shoulder injuries of volleyball players, another study found that SICK scapula significantly contributes to increased tension on the suprascapular nerve and thus causes traumatic injury [15].
The injury to the posterior part of the suprascapular nerve is thought to occur due to multiple, abrupt, peculiar stretching of infraspinatus tendon during the deceleration phase of the floater serve (the most common type of overhead volleyball serve). Ferretti observed such injury in volleyball players while Arash et al. observed this in various overhead sports players as well as labourers [15].
2.6. Other Etiologies
• Nerve ischaemia: In very rare conditions, microemboli formed after any trauma gets trapped in the suprascapular artery and then migrate to the vasanervorum thus hindering the blood and fluid supply to the suprascapular nerve. This leads to nerve ischemia and then neuropathy [21].
3. PRESENTATION & DIAGNOSIS OF SUPRASCAPULAR NEUROPATHY
The pertinent clinical presentations of suprascapular neuropathy are as follows:
- Shoulder pain which worsens on cross-body adduction or internal rotation of ipsilateral muscle.
- Atrophy of supraspinatus or/and infraspinatus muscle, observable on physical examination.
- Weakness of shoulder abduction and external rotation observed during manual muscle testing.
- The tenderness between the clavicle and the spine of the scapula or deep and posterior to the acromioclavicular joint [22].
Radiological examination using X-rays is the first step in diagnostic workup if suprascapular neuropathy is suspected. It is important to have a radiological view of a suprascapular and spinoglenoid notch along with a standard view of the shoulder area. However, no remarkable changes can be observed in the radiographic images unless there is a prominent trauma responsible for the condition. The suprascapular notch is best seen on oblique coronal images orientated along the scapula. The spinoglenoid notch is best seen on axial images. MRI of the shoulder helps in identifying muscle oedema, muscle atrophy, and ganglionic cyst Fig. (2) [23]. Three Tesla (3-T) MRI scan is another tool used in the diagnosis of suprascapular neuropathy because it is helpful in identifying any nerve abnormality or any denervation changes in muscles [24]. The effectiveness of MRI lies in the direct visualization of nerve as well as the simultaneous assessment of the cervical spine, brachial plexus, and rotator cuff.

Ultrasound is also applicable for the diagnosis of cysts particularly within the suprascapular notch and other muscle abnormalities as it is an inexpensive and relatively accurate diagnostic tool [24].
Electrodiagnostic studies are gaining popularity as an important diagnostic tool for suprascapular neuropathy. Positive sharp waves and fibrillation potentials indicated by electromyography can suggest denervation while polyphasic motor unit action potentials suggest motor innervation abnormalities. Larissa et al suggest that electromyography (EMG) and nerve conduction velocity (NCV) tests are the gold standards for the detection of suprascapular nerve injury [10]. This study was conducted as a retrospective cohort study in a Tertiary medical center on 65 patients with electormyo- gaphically confirmed suprascapular neuropathy. The study concluded that there were three main causes of SSN in these patients; namely trauma, inflammatory process (i.e. Brachial neuritis), and cyst. EMG and NCV are suggested in the following conditions:
- Consistent pain in the posterosuperior aspect of the shoulder and no confirm diagnosis is found.
- Atrophy as well as the weakness of supraspinatus and infraspinatus tendons in the absence of rotator cuff injury.
- MRI observations show muscle edema.
- Massive rotator cuff tear with retraction and consequent traction on the nerve.
A study examining the normative values for the electro- diagnosis has shown that the normal distal motor latencies to the supraspinatus muscles during stimulation at the Erb point are 2.7 msec ± 0.5 and to the infraspinatus muscles, 3.3 msec ± 0.5. Side-to-side differences greater than 0.4 msec suggest focal entrapment of the SSN or another neural injury.
In some cases, where outcomes of these electrodiagnostic studies are negative or not specific; fluoroscopically guided local anesthetic injection is used. This injection is administered to the region of the suprascapular nerve and related pain relief is evaluated. This method is very effective in confirming the involvement of suprascapular nerve injury in shoulder pain [25].
4. TREATMENT MODALITIES FOR SUPRASCAPULAR NEUROPATHY
Treatment for suprascapular neuropathy is selected on the basis of different factors such as etiology of nerve damage, the severity of nerve damage, duration of pain and weakness in the shoulder, degree of functional disability and patient’s choice. The three main types of treatment options are physical therapy, nerve block and surgical repair.
4.1. Physical Therapy
If the suprascapular neuropathy is caused due to rotator cuff tear or labral tear with paralabral cyst, the treatment selection is done with regards to the pathology. However, in the case of isolated nerve injury, the conservative treatment plan including activity modification, analgesic drugs, and physical therapy is initiated. The patient is asked to avoid or stop overhead activity as soon as he/she is diagnosed with suprascapular neuropathy. Following which, a physical therapy program is initiated which focuses on the movement of shoulder and muscle strengthening. The therapy also includes scapular stabilization [26].
Different studies on patients with isolated suprascapular neuropathy suggest that non-operative treatment for 6 months to 1 year provides good to excellent outcomes in the majority of the patients while surgical intervention following physical therapy is required in only 20% patients [14]. Boykin et al suggest that such non-operative treatments in the case of suprascapular neuropathy due to compression by mass or a cyst do not provide satisfactory results. It has been found that 53% of patients with suprascapular neuropathy due to spinoglenoid cyst get significant pain control and symptomatic relief with non-operative methods while 96% of such patients experience positive outcomes with surgical treatment [4].
4.2. Nerve Block
Nerve blocks are non-surgical treatment options for suprascapular neuropathy. Nerve blocks are usually adminis- tered to manage shoulder pain in pre-operative setups as well as in the case of painful shoulder conditions like adhesive capsulitis. Diagnostic usage and specificity of nerve blocks are widely debated, but the blocks are used to achieve rapid symptomatic relief so that the patient can properly participate in the rehabilitation physical therapy. Nerve blocks consist of an injection of an anaesthetic mixed with corticosteroid administered to the suprascapular notch [27].
Newer techniques like radiofrequency ablation of suprascapular nerve or palliative treatment for pain due to suprascapular neuropathy are still in the research phase and are not yet widely applied.
4.3. Surgical Treatment
Surgical treatment options can be offered to patients where conservative modalities have been exhausted. Furthermore, surgical intervention is immediately offered if suprascapular neuropathy is concomitant to rotator cuff tear or labrum tears with paralabral cysts. However, literature review suggests that there are debates about performing nerve decompression in addition to treating concomitant pathology. Many researchers recommend only correction of isolated rotator cuff or labral pathology and avoid concomitant nerve decompression [4].
5. SURGICAL TREATMENT AT SUPRASCAPULAR NOTCH
Nerve damage at the suprascapular notch is usually treated with the release of the transverse ligament by an open or arthroscopic technique. Fewer complications have been observed with the open technique. Patients are reported to have adequate pain relief as well as improved muscle strength with the open technique. However, muscle atrophy cannot be reversed in all cases using this technique. Improvement of supraspinatus muscle strength is observed among 90% of patients treated by open technique while no significant improvement of infraspinatus muscle is seen [28].
6. ARTHROSCOPIC APPROACH TO THE SUPRASCAPULAR NOTCH
The arthroscopic release is not only less invasive and allows for better visualisation and access, but importantly it also allows for any intra-articular pathology to be addressed and is becoming increasingly used.
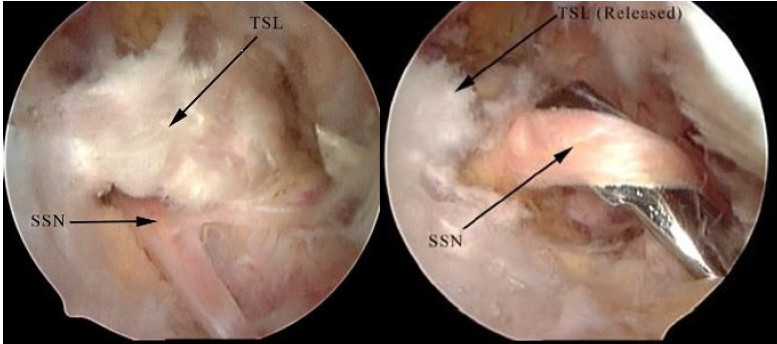
The patient is placed in a beach chair position, with the arthroscope in an anterolateral portal alongside an accessory anterior and posterior portal. The coracoid process is first visualised, followed by dissection medially of the fibrofatty tissue via a lateral portal [11]. The coracoacromial and coracoclavicular ligaments are identified, following which the suprascapular notch can be located at the medial base of the coracoid. The transverse scapular ligament can then be released using arthroscopic punches with careful dissection in order to avoid injury to the suprascapular artery and nerve Fig. (3) [29]. Following this the nerve can be probed to verify that there is no further compression [11, 30].
7. SURGICAL TREATMENT AT SPINOGLENOID NOTCH
Nerve damage at spinoglenoid notch is usually secondary to nerve compression by the space-occupying lesion. Surgical management of such lesions often requires open or arthroscopic approach and resection of the lesion. It is noteworthy that patients with suprascapular neuropathy at spinoglenoid notch show poor results with physical therapy alone and thus are suggested to have surgical intervention immediately. Cyst recurrence rates are very low with both the methods [11]. Literature review suggests that ultrasound-guided paralabral cyst aspiration is a good alternative to surgical intervention for suprascapular neuropathy due to compression at spinoglenoid notch. While the majority of patients reported excellent pain relief with the technique, recurrence rates for cyst are found to be between75-100% [31].
8. ARTHROSCOPIC SURGICAL APPROACH AT THE SPINOGLENOID NOTCH
The patient is placed in a beach chair position and a trans-rotator cuff portal is created with the arthroscope placed laterally through the portal. The posterosuperior capsule should be released at the periphery of the labrum until supraspinatus can be visualised. Supraspinatus is then superiorly elevated. The suprascapular nerve can be located 2.5cm medial to the superior aspect of the glenoid towards the base of the supraspinatus fossa, from where it can be posteriorly traced as it passes through the spinoglenoid notch. Handheld basket punches can be used to release the nervein in this location [12, 30].
CONCLUSION
The presence of suprascapular neuropathy can be more easily recognised now due to increased understanding of the condition and improved diagnostic methods. Overhead athletes presenting with vague posterosuperior shoulder pain, muscle atrophy, weakness of supraspinatus and infraspinatus tendons must be investigated for suprascapular neuropathy. The condi- tion must also be investigated in all the athletes with a rotator cuff tear, due to the high incidence. MRI and EMG are the most reliable diagnostic techniques to identify suprascapular neuropathy and rotator cuff health. Recently, fluoroscopically guided injections to the suprascapular notch are also gaining popularity as a diagnostic method for the condition. While conservative physical methods can be applied to treat the isolated suprascapular neuropathy, open or arthroscopic surgical intervention is the definitive way of treating suprascapular neuropathy due to rotator cuff tear and cystic compression.
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


