All published articles of this journal are available on ScienceDirect.
A Clinical and Magnetic Resonance Imaging Assessment of Anterior Cruciate Ligament Reconstruction with Different Fixation Techniques Using Gracilis and Semitendinosus Autograft
Abstract
Background:
Hamstring tendons are widely used in anterior cruciate ligament reconstruction. Improvements in fixation materials have increased the success of the reconstruction procedures using this type of graft. The main advantage of the hamstring tendon autograft is the lower donor site morbidity associated with its harvesting. On the other hand, tunnel widening is reported more frequently with the use of hamstring tendon autograft compared to patellar or quadriceps tendons. The objective of the present study was to evaluate three different fixation techniques at a minimum of 2 years after Anterior Cruciate Ligament (ACL) reconstruction using gracilis and semitendinosus autograft.
Methods:
Between February 2012 and March 2016, 112 ACL reconstructions using double looped semitendinosus and gracilis graft were performed. Patients were divided into 3 groups in a randomized fashion. 98 patients were followed up for 2 years. In the first group (43 patients), suspensory fixation using Retrobutton (Arthrex, Inc, Naples, Florida) was used. In the second group (30 patients), transcondylar graft fixation Bio-Transfix (Arthrex, Naples, Florida) was performed, and in the third group (25 patients), aperture fixation using AperFix (Cayenne Medical, Scottdale, Arizona, Biomet) was performed. Clinical evaluation was performed using the International Knee Documentation Committee (IKDC) form, Lysholm knee and Tegner activity level scores, as well as arthometer measurements. Tunnel enlargement and graft integrity were evaluated using Magnetic Resonance Imaging (MRI) at 6, 12 and 24 months.
Results:
Ten patients were completely lost to follow up, and four had undergone a revision ACL reconstruction before the two-year follow up period, leaving 98 patients for analysis. No statistically significant differences between the three groups were noted other than that the first group tended to have more tunnel enlargement than the other two groups, especially at the femoral tunnel (p=.026), but not at the tibial tunnel (p>0.408). Our results showed that almost 90% of the patients in the three groups had functionally normal or near normal IKDC, Lysholm and Tegner scores.
Conclusion:
The three different techniques yielded equal results as regards improved patient performance. The functional results as well as knee stability tests were not related with tunnel enlargement, at least in the short term.
1. INTRODUCTION
Anterior Cruciate Ligament (ACL) reconstruction is the sixth most common procedure in orthopaedic surgery. Almost 100.000 ACL repair procedures are performed annually in the USA alone. Although widely investigated, ACL reconstruction still continues to evolve with various technical issues under debate. These include proper tunnel placement, the use of single or double bundle technique, the type of fixation as well as the selection of the graft [1].
The most common autografts currently used are bone-patellar tendon-bone and hamstrings tendon, and, less commonly, the quadriceps tendon. A recent Cochrane trial comparing BPTB and hamstrings tendon repairs outcomes was inconclusive [2]. In 1988 Friedman pioneered the use of an arthroscopically assisted four stranded hamstring graft technique [3]. Since the early 90s, enlargement of bone tunnels after anterior cruciate ligament reconstructions has been well-documented. For ACL reconstructions using hamstrings, the incidence of enlargement varies between 11% and 47% [4]. Hamstrings autografts have relatively low donor site morbidity, the dimensions of the graft are closer to the intact ACL and the ultimate strength is as high as 4090 N [5, 6]. On the other hand, there is still concern about the graft healing within the osseous tunnels. Although many studies report bone tunnel enlargement after ACL reconstruction, none proved to be clinically significant or related to inferior clinical results or higher failure rates [7-10]. Concerns only exist in cases where a surgical reoperation is necessary.
The Magnetic Resonance Imaging (MRI) is a useful pre-operative tool both for the confirmation of an ACL tear as well as to assess concomitant injuries. It is also useful post-operatively, because it is a non-invasive way of providing valuable information regarding the graft signal and its integrity, the tunnel widening, the correct tunnel placement, problems associated with different fixation devices that could compromise the surgical outcome, and possibly of predicting the failure of an ACL reconstruction.
The autograft undergoes a maturation and remodeling process often lasting more than two years and consisting of four stages: the initial avascular necrosis stage, the revascularization, the cellular proliferation, and, finally, the remodeling. The entire process from a tendon graft toward histologic and biomechanical adaptation similar to the native ACL is known as “ligamentization”. This process can be monitored by MRI, as it has been proved that an incomplete graft maturation is related to a hyperintense graft signal on MRI. When gracilis and semitendinosus autograft tendons are used, there is a slower maturation process at 6 months compared to other autografts, such as BPTB or quadriceps tendon autograft, thus suggesting a late remodeling period sometimes reaching two years. It is suggested to modify the rehabilitation protocol according to the extent of graft maturation, in order to prevent re-rupture and to maximize the clinical results. Therefore, the MRI evaluation of the graft signal can provide valuable information regarding the state of maturation, the correct placement of the graft, the integrity of the graft and the tunnel widening, and may influence the long term results.
Graft fixation is obtained using a wide range of fixation devices, which differ in shape, size, material, biomechanical properties and positioning. The modern fixation techniques provide generally good results although graft failure can occur in 6%-11% of the cases.
The purpose of this study is to compare both the clinical results and the MRI findings of different fixation techniques using hamstring autografts and to assess the outcomes at a minimum 2-year follow up.
2. METHODS
From February 2012 to March 2016, 112 patients with ACL ruptures underwent arthroscopically assisted reconstructions using hamstrings autografts. All surgeries were performed in the same institution under general or spinal anesthesia using a pneumatic tourniquet in the supine position. The ethical committee of the Hospital approved the study and the patients were informed of the study procedure, and the purpose of the study, and they provided informed consent.
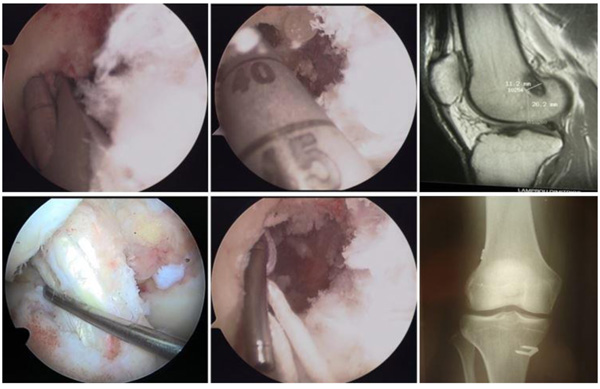
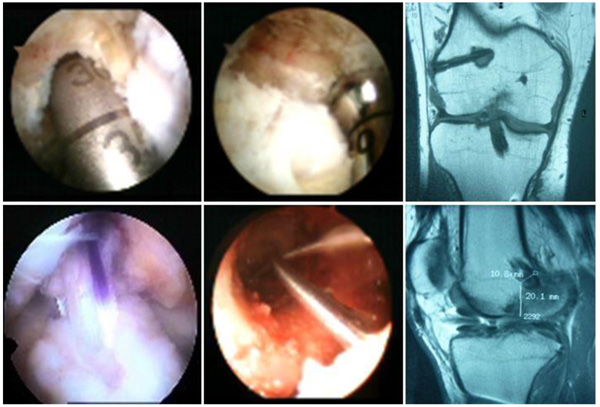
Routine diagnostic arthroscopy was performed on all patients initially. A double looped semitendinosus and gracilis tendon autograft was used. The tibial tunnel was created at the center of the footprint and reamed first while the femur was reamed either transtibially or via AM portal trying to put the tunnels as anatomically as possible. The positioning of the femoral tunnel is the primary factor for graft isometry [11]. The positioning of the tibial tunnel is the primary factor ressible for the impingement of the graft against the roof of the intercondylar roof [12]. The guide pin was inserted approximately 2-2.5 cm medial to the tibial tuberosity to approximately 6-8 mm anterior to the posterior cruciate ligament with an angle of 55o-65o with respect to the medial joint line of the tibia. After the tibial tunnel was rasped, the femoral guide pin was inserted using the femoral offset guide which was selected according to the graft thickness, preserving 1.5-2.0 mm thickness of the posterior femoral cortex. In the first group (Group A), a suspensory femoral graft fixation with RetroButton (Arthrex, Inc, Naples, Fl.) device was used in 43 patients (31 males and 12 females) (Fig. 1). In the second group (Group B), the Bio-TransFix device (Arthrex, Inc, Naples, Fl.) was used for transcondular femoral fixation in 30 patients (22 males and 8 females) (Fig. 2). The third group (Group C) included 25 patients (20 men and 5 women) and an aperture fixation with the AperFix device (Cayenne Medical, Scottdale, Ar, Zimmer, Biomet) was used (Fig. 3). In groups A and B a bioabsorbable screw and a post tie with u staple was used for the tibial graft fixation. In group C a non absorbable PEEK (polyetheretherketone) polymer sheath-screw implant was used for tibial sided fixation (Table 1).

| Group A | Group B | Group C | |
|---|---|---|---|
| Age at surgery | 29±12 | 27±10 | 28±10 |
| Lost on follow up | 5 | 3 | 2 |
| 2 years follow up | 43 | 30 | 25 |
| Male (n) | 31 | 22 | 20 |
| Female (n) | 12 | 8 | 5 |
| Median interval from injury to surgery | 4.5 mo (3 wk-2yr, 9mo) |
4 mo (3 wk-3yr, 6 mo) |
4 mo (2 wk-3yr, 10 mo) |
| Medial/Lateral meniscal lesions | 11/4 | 9/4 | 8/3 |
Patients followed an identical conservative postoperative rehabilitation program. The inclusion criteria were unilateral ACL rupture confirmed clinically and by MRI, age 17-50 years, no previous knee ligament surgery and a normal contralateral knee. Patients who had a concurrent meniscal injury that was managed with partial meniscectomy were also included. The exclusion criteria were concomitant ligament injuries and grade iii and iv cartilage defects requiring additional chondroplasty. The experimental part of this study was performed by 1.5 Tesla MRI scan (Philips Gyroscan NT Compact Plus), which took place at 6, 12 and 24 months after surgical reconstruction. MRI images were constructed from 2.0 mm-thick slices with 1 mm gap between slices. In our centre, the standard knee protocol comprises Coronal T2 weighted fat suppressed sequence, TSE sagittal intermediate weighted sequence, TSE axial intermediate weighted with fat suppression and T1-weighted sequences as well as small coil images and small FOV images when necessary. The following parameters were tested in the MRI: (i) the anterior and posterior femoral and tibial tunnel diameter at a distance of 2 cm from the joint surface; (ii) the widening of the tunnels and their shape; (iii) the signal of the intra-articular part of the implant as compared to the central and the peripheral parts in order to evaluate its integrity, and (iv) the existence or not of acquired lesions (meniscal or chondral). Anterioposterior and lateral digital plain radiographs at 6, 12 and 24 months were also performed.
2.1. Postoperative Treatment
The hemovac drain was removed on the first day after surgery. A non-aggressive rehabilitation program was followed. Postoperatively, a brace was used in full extension for 4 days. The second day postoperatively the patients were allowed partial weight bearing as tolerated and closed-chain exercises were encouraged. At 4 weeks, the patients were weaned of crutches; at 6 weeks, the brace was removed and full range of motion was gained. At three months, the patients began activities such as jogging and swimming. Open-chain exercises were allowed at 4 months. All kinds of sports were allowed 9-12 months after operation.
3. RESULTS
A total of 112 patients suffering a fresh or chronic ACL injury were operated on, using double looped semitendinosus and gracilis graft. Ten patients were completely lost to follow up, and four had undergone a revision ACL reconstruction before the two year follow up period, leaving 98 patients for analysis. All patients in the three groups had functionally normal or near-normal IKDC, Lysholm and Tegner scores. The average subjective IKDC knee form scores at 2 years were 90 ± 10 in group A, 89 ± 10 in group B and 89 ± 11 in group C (p>0.6) and KT1000 differences were 2.2 ± 1.6mm in group A, 2.1 ± 1.5 in group B and 2.4 ± 1.8 in group C, p=0.498 (Table 2).
Tunnel enlargement in all three groups was more significant at the femoral tunnels p>0.026 (Tables 3-4) than the tibial tunnels p>0.408 (Tables 3-4).
The analysis of the results of tunnel enlargement showed a statistically significant difference at the coronal plane in the thigh in group A (Table 3), while there was no statistically significant difference in the sagittal plane (Table 4). There was no statistically significant difference between the groups for tibial tunnel widening at the coronal plane and no statistically significant difference was observed at the sagittal plane either.
Two patients in group A (4.6%), one in group B (3.4%) and one in group C (4.1%) sustained a new graft rupture due to adequate trauma. There were also 5 fresh meniscal injuries in group A (11.6%), 3 in group B (10%) and 2 in group C (8%) (Table 5).
Ten additional procedures were performed with no correlation to the randomized groups. These cases were grouped together and analyzed against the rest of the material. No significant difference was noted either with respect to the various knee scores (Lysholm, Tegner, IKDC) or with respect to KT 1000 arthrometer evaluation results. Two deep infections were noted (one in the RetroButton, and one in the TransFix group), treated by arthroscopic washouts, retention of the graft and culture specific iv antibiotic therapy, with eventual healing of the graft and a clinically stable knee. In two other cases (one in the RetroButton, and one in the AperFix group) a deep vein thrombosis that occurred was treated by thrombolytic treatment. There were also two broken implants (in the TransFix group) at 20 and 27 weeks postoperatively with no signs of instability.
| Scores | Group Α | Group Β | Group C | |
|---|---|---|---|---|
| Pre-op | Tegner | 3 (1-5) | 3 (1-5) | 3 (1-4) |
| Lysholm | 74 (56-83) | 71 (36-82) | 70 (35-78) | |
| IKDC | 57 (46-79) | 48 (30-76) | 55 (35-73) | |
| KT 1000 | 4.2/5.6* | 4.3/5.7* | 4.9/5.4* | |
| Post-op 6 months |
Tegner | 5 (3-8) | 5 (3-8) | 5 (3-8) |
| Lysholm | 86 (70-90) | 87 (72-92) | 85 (68-92) | |
| IKDC | 82 (72-95) | 80 (57-90) | 84 (62-92) | |
| ΚΤ 1000 | 2.2/2.4* | 1.8/1.9* | 2.0/2.6* | |
| 1 year | Tegner | 6 (4-10) | 6 (3-9) | 6 (4-9) |
| Lysholm | 90 (72-100) | 88 (67-96) | 89 (74-100) | |
| IKDC | 88 (72-100) | 88 (57-95) | 87 (68-100) | |
| ΚΤ 1000 | 2.0/2.2* | 1.6/1.7* | 2.1/2.5* | |
| 2 years | Tegner | 6 (4-10) | 7 (3-9) | 6 (4-9) |
| Lysholm | 90 (72-100) | 89 (67-96) | 89 (74-100) | |
| IKDC | 89 (72-100) | 90 (57-95) | 89 (68-100) | |
| ΚΤ 1000 | 1.6/2.2* | 1.3/2.1* | 1.7/2.4* |
| Tunnel widening | Group Α | Group Β | Group C | P value | |
|---|---|---|---|---|---|
| Femur/ Tibia 6 months |
6-8mm | 5 / 1 | 0 / 0 | 0 / 0 | .028/.309 |
| 4-6mm | 9 / 7 | 5 / 1 | 2 / 5 | ||
| 2-4mm | 11 / 11 | 8 / 7 | 7 / 8 | ||
| <2mm | 18 / 24 | 17 / 22 | 16 / 12 | ||
| Femur/ Tibia 1 year |
6-8mm | 5 / 2 | 1 / 0 | 0 / 0 | .011/.376 |
| 4-6mm | 10 / 6 | 6 / 3 | 2 / 5 | ||
| 2-4mm | 10 / 13 | 7 / 5 | 8 / 8 | ||
| <2mm | 18 / 22 | 16 / 22 | 15 / 12 | ||
| Femur/ Tibia 2 years |
6-8mm | 5 / 3 | 0 / 1 | 0 / 0 | .026/.336 |
| 4-6mm | 10 / 7 | 6 / 4 | 0 / 4 | ||
| 2-4mm | 10 / 13 | 9 / 5 | 9 / 11 | ||
| <2 mm | 18 / 20 | 15 / 20 | 16 / 10 |
| Tunnel widening | Group Α | Group Β | Group C | P value | |
|---|---|---|---|---|---|
| Femur/ Tibia 6 months |
6-8mm | 1 / 0 | 0 / 0 | 0 / 0 | .430/.182 |
| 4-6mm | 3 / 1 | 3 / 1 | 0 / 2 | ||
| 2-4mm | 15 / 21 | 9 / 6 | 10 / 8 | ||
| <2 mm | 24 / 21 | 18 / 23 | 15 / 15 | ||
| Femur/ Tibia 1 year |
6-8mm | 3 / 1 | 1 / 0 | 0 / 0 | .008/.449 |
| 4-6mm | 8 / 9 | 5 / 3 | 2 / 3 | ||
| 2-4mm | 12 / 14 | 8 / 7 | 8 / 10 | ||
| <2 mm | 20 / 19 | 16 / 20 | 15 / 12 | ||
| Femur/ Tibia 2 years |
6-8mm | 4 / 2 | 0 / 1 | 0 / 0 | .101/.408 |
| 4-6mm | 8 / 9 | 6 / 5 | 0 / 2 | ||
| 2-4mm | 14 / 14 | 10 / 6 | 9 / 10 | ||
| <2 mm | 17 / 18 | 14 / 18 | 16 / 13 |
| Graft rerupture/failure | Group Α | Group Β | Group C |
|---|---|---|---|
| 6 months | 0 | 0 | 0 |
| 1 year | 1 | 1 | 0 |
| 2 years | 1 | 0 | 1 |
| New meniscal lesions | |||
| 6 months | 0 | 0 | 0 |
| 1 year | 2 | 1 | 1 |
| 2years | 3 | 2 | 1 |
4. DISCUSSION
Anterior cruciate ligament tear is a detrimental event for any patient, and appropriate management is important in order to ensure return to pre-injury activity but also to prevent long-term complications due to the knee injury. Surgical management of ACL tear appears to be the answer in patients who wish to restore their pre-injury activity level [3, 5, 6, 13-17]. Hamstring tendons are being used increasingly in anterior cruciate ligament reconstruction claiming lower harvest-site morbidity when compared with patellar tendon grafts [18, 19]. It has been shown that a 4-stranded hamstring tendon graft is stronger than the BPTB graft [19], but the weakest point in hamstring tendon ACL reconstruction is not the graft itself but the fixation sites.
In MRI observation of the patients’ postoperative condition, a normal ACL graft should have low signal intensity on short TE sequences [7, 20-22]. Intermediate signal was often seen at approximately 4 to 8 months postoperatively, decreasing with time and usually completely resolving by 12 months [20]. This increased signal is thought to be due to graft revascularization and ligamentization [23, 24]. Because the doubled semitendinosus and gracilis tendon graft is composed of four separate strands, intermediate signal and even fluid can normally be seen between the strands of the graft of T2-weighted sequences. This normal intermediate signal is always oriented along the fibers of the graft as opposed to a tear, which is perpendicular to the graft. A helpful feature distinguishing revascularization of the graft from disruption is the lack of concomitant secondary signs of rupture, such as anterior tibial translation and uncovering of the posterior horn of the meniscus.
ACL fixation methods have improved significantly over the past decade. Currently a variety of fixation techniques are available allowing for early return of neuromuscular function. After arthroscopic ACL reconstruction, the autograft used to replace the ruptured ligament undergoes a biological healing process consisting of four phases: initial necrosis, revascularization, cellular repopulation and remodeling [25-28]. Graft fixation has not only to withstand the physiological forces but also to facilitate the biological incorporation of the graft construct. Among the related complications, tunnel elongation has been reported regardless of the technique used [17, 26]. Tunnel widening seen after anterior cruciate ligament reconstruction has been the topic of several reports since the 1990s [8, 9, 19, 29, 30] Tunnel widening occurs mainly during the first 6 months after surgery, while the process of maturation (ligamentization) may continue for more than a year [27, 28, 31]. The aetiology of this enlargement is multifactorial, including both mechanical and biological factors. Mechanical factors include micro motion of the graft in the tunnels, inappropriate positioning, bone necrosis during drilling as well as aggressive rehabilitation programs. Biological factors include bone resorption, graft edema, tunnel synovial fluid infiltration, and increased cytokine concentration (IL-6 & TNF-alpha). Hoher et al. [10] showed that graft tunnel motion can be 2 to 3mm even during physiologic loads when suspensory fixation (endobutton) was used. Results are conflicting as to whether or not rigid fixation of the graft close to the joint, known as aperture fixation, can decrease graft-tunnel motion and possibly tunnel widening [4, 32-34]. In porcine femora, the interference screws and the Rigidfix fixation demonsrated inferior fixation biomechanics compared with Bio-Transfix (Arthrex, Inc, Naples, Fl.) and EndoButton techniques [35]. Transcondylar femoral cross-pin fixation was described by Clark, et al. [14]. They showed that biomechanical properties were superior to other femoral fixation devices in hamstring ACL surgery, although Rose, et al. [36] confute their hypothesis that the trasfixation technique leads to less laxity and therefore to a better clinical outcome when compared with the use of bioabsorbable screws. According to a recent study by Lopes et al., greater enlargment of the femoral bone tunnel was observed when a bioabsorbable trans-tunnel pin system was used with medial portal technique, compared to extracortical fixation [37]. Will a shorter graft and more rigid graft complex fixation produce less tunnel enlargement? The most optimal fixation method has not yet been defined. In the present study, different fixation techniques were compared. No statistically significant differences between the fixation methods were observed except tunnel enlargement at the coronal plane at the femoral side in group A (RetroButton). There were no significant differences between the groups either with respect to the various knee scores (Lysholm, Tegner, IKDC) or with respect to KT 1000 arthrometer evaluation results. The goal of the present study was to evaluate different fixation devices, to compare the expected development of tunnel widening when using hamstring autografts and if there is any impact or clinical implication and finally to report the results at 6 months, 1 and 2 years after surgery. We hypothesized that all 3 techniques provide equal results in restoring knee stability.
There are some limitations in this study. Three groups are difficult to handle. Statistical analysis became difficult to interpret, and there was little room for missing cases. Also in some cases of the third group there was some difficulty in measuring the tunnels on the femoral side on MRI, because of artifacts caused by the femoral implant material. We believe that more, randomized, controlled, prospective studies are needed.
CONCLUSION
This study showed that more rigid fixation techniques lead to less femoral tunnel enlargement but do not lead to significant differences with respect to Lysholm, Tegner, IKDC scores or arthrometric evaluation results. It is important to evaluate the performance of these fixation methods in prospective randomized studies comparing them with standard methods. According to our study, all three techniques yielded satisfactory results in almost 90% of patients in all groups. We concluded that the position of the fixation sites and type of fixation device are contributing, but are not the only factors responsible for development of tunnel widening after ACL surgery. As other authors have reported [8, 9, 29, 30, 34], we did not find a significant correlation between tunnel widening and clinical outcome. This could be because TW is without implications for the clinical situation or a difference did not emerge because of a small number of patients. On the other hand, we also believe that all fixation techniques should be designed in a manner that will reduce the incidence of TW as much as possible, because it is clear that a wide bone tunnel filled with fibrous tissue can potentially complicate a later revision ACL procedure. We have not been able to establish any superiority of one fixation technique over the other, because they all have similar results and overall patient satisfaction was more than 89%.
LIST OF ABBREVIATIONS
| IKDC | = International Knee Documentation Committee |
| ACL | = Anterior Cruciate Ligament |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Review Board approval was obtained before starting the study from Agioi Anargyroi General Hospital.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Each patient gave written and informed consent before each surgical procedure.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


