All published articles of this journal are available on ScienceDirect.
Comparative Retrospective Analysis of Accuracy of Robotic-Guided versus Fluoroscopy-Guided Percutaneous Pedicle Screw Placement in Adults with Degenerative Spine Disease
Abstract
Background:
Robotic-guidance for pedicle screws can reportedly increase placement accuracies and surgical efficiencies especially in percutaneous approaches.
Objective:
The study aimed to compare the accuracy of percutaneous pedicle screw placement and post-operative course of robotic-guidance versus fluoroscopy-guidance performed by a surgeon experienced in performing fluoroscopy-guided MIS spinal fusions.
Study Design:
This is a retrospective medical chart review of 2 cohorts of consecutive patients operated by the same surgeon.
Methods:
Medical records of adults suffering from degenerative spine disease treated by percutaneous spinal fusion surgeries with robotic-guidance vs. fluoroscopy-guidance were reviewed. Endpoints included pedicle screw placement accuracy (on post-operative CTs) and surgical complications and revisions.
Results:
Ninety-nine patients were reviewed in each arm which were similar in demographics and surgical indications. The robotic arm had 5.8 screws per case on average and 6.0 in the control arm (p=0.65). No significant differences were found in postoperative complication rates revision surgeries length of stay duration of surgery screw implantation times blood loss or results of Oswestry Disability Index questionnaires.
Post-operative CTs were available for 52 patients (293 screws) in the robotic arm and 70 (421 screws) in the freehand controls. In the robotic arm 100% of screws were found accurately placed within the “safe zone” vs. 410 screws (97.4%) in the control arm (p=0.005). Of 11 breaching screws in the control arm one breached by 6mm but the patient did not suffer from any sequelae (12-month follow-up). The average follow up period was 9.2±4 months in the robotic-guided arm and 10.5±3 in the control arm. There were no significant differences in complications or revisions.
Conclusion:
A modest yet statistically significant increase in pedicle screw placement accuracy was observed with robotic-guidance compared to freehand. Larger prospective studies are needed to demonstrate differences in clinical outcomes.
1. INTRODUCTION
The benefits of Minimally Invasive Spine surgery (MIS) are supported by a significant body of published evidence. A meta-analysis of comparative studies assessing the clinical and radiological efficacy of MIS versus conventional open Transforaminal Lumbar Interbody Fusion (TLIF) procedures, concluded that significantly improved functional outcomes, reduced blood loss and shortened hospital stay were obtained following MIS, as compared to open procedures [1]. Another meta-analysis found similar fusion rates between the two techniques [2]. However, the MIS approach remains technically demanding as it limits or fully blocks the surgeon’s line of sight, requiring the use of dedicated surgical instruments and imaging platforms. This reliance increases intraoperative radiation exposure [1] and operation times during the initial stages of the learning curve, which has been estimated to span about 30 single-level MIS-TLIF cases [3].
There is a paucity of reports on multi-level MIS fusions in the literature, which can be interpreted as a proclivity for utilization of an MIS approach in less complex surgeries, despite its clinical advantages. This trend was evident in a quantitative meta-analysis of fusion and complication rates in 23 comparative studies of open versus minimally invasive/mini-open TLIF procedures, involving 1,028 patients [2].
Image-guidance systems provide surgeons high levels of accuracy and consistency, shortening the learning curve of MIS surgical techniques. Navigation systems have been shown to increase pedicle screw placement accuracy compared to freehand techniques, from about 90-91% to around 95-97% [4, 5]. Robotic guidance systems have shown similar or higher levels of accuracy [6, 7, 20], even when used in MIS procedures and compared to a freehand open approach [8, 9, 21, 23]. In addition, Kim et al. showed a decrease in radiation doses to below detectable levels when integrating navigated-assisted fluoroscopy in MIS-TLIF, in contrast to a mean 12.4 mREM radiation dose in open, standard fluoroscopy TLIFs [11]. Several studies noted significant radiation exposure reductions, ranging from 48-65%, when employing robotic-guidance in MIS fusions, compared to open-approach freehand cases [8, 9, 23]. Thus, despite limited visibility and working range, MIS procedures can be equally accurate, with equal fusion rates and with fewer complications than corresponding open approaches. The current study assesses the performance and accuracy of robotic-guided fusion procedures, executed by an experienced MIS surgeon (FZ), compared to his freehand, fluoroscopy guided, baseline performance in consecutive patient cohorts.
2. METHODS
2.1. Study Design
This was a retrospective, consecutive patient review of medical charts and imaging data collected during freehand and robotic-guided percutaneous pedicle screw instrumentation procedures, all performed by the same surgeon in a community-based hospital.
2.3 . Procedure
MIS-TLIF with pedicle screw instrumentation was performed in a percutaneous approach. A semiautonomous, bone-mounted, surgical guidance robot (Renaissance©, Mazor Robotics Ltd., Caesarea, Israel) was used. The system is comprised of a small, parallel robot, mounted directly to the patient’s spine, which intraoperatively guides surgical tools along preoperatively planned trajectories. The robotic unit is connected to a workstation, which holds the kinematic controllers and computer running proprietary software used for preoperative planning, intraoperative registration process and control of the robotic unit. The planning stage uses a preoperative CT scan to optimize implant sizes and tailor operative trajectories to suit the anatomical constraints, yielding a detailed surgical blueprint. The system’s features and surgical technique, including the intraoperative use of mounting platforms and the automated registration process, have been previously detailed [10-12]. The current study used different mounting platforms to mount the robotic guidance unit to the patient’s spine, in accordance with the manufacturer’s recommendations and the surgeon’s judgment. The robotic system guided the surgeon to the preoperatively planned trajectory, after which, a cannula was placed through the robotic unit’s arm and then secured to the bone at its tip. A manually operated power-drill was passed through the cannula to drill pilot holes of 3 mm diameter and 30 mm depth. A solid reduction tube was used to insert a K-wire to facilitate the instrumentation of each pedicle. All pedicle screws (Viper2©, Depuy-Synthes Spine Inc., Raynham, MA) were placed in a percutaneous approach over these K-wires.
2.4. Control Arm
Using fluoroscopy-guidance, a Jamshidi needle was used to create a pilot hole and insert a K-wire into the pedicle. There was no difference in techniques between the two arms once the K-wires were within the pedicle.
In both study arms, decompressions were performed in a minimally invasive fashion through a tubular retractor system [add system name, manufacturer, city and state].
2.5 . Outcome Measures
Antero-posterior and lateral fluoroscopy images were used for review of pedicle screw placement intraoperatively at the end of instrumentation in both arms. Pedicle screw accuracy, as determined in accordance with Gertzbein and Robbins’s classification [13] of screw positions viewed on postoperative CTs, was compared, as were surgical complications and revision incidence.
3. RESULTS
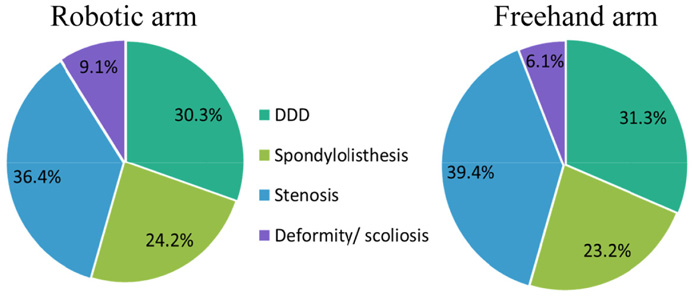
The charts of 99 patients undergoing percutaneous, robotic-guided pedicle screw instrumentation between the years 2012-2013, were reviewed. Charts of 99 additional patients operated between 2011-2012, using a percutaneous approach with fluoroscopic guidance, were reviewed as a control arm. Surgical indications were similar between arms, with the majority of patients presenting stenosis, followed by degenerative disc degeneration, spondylolisthesis and deformity/scoliosis (Fig 1). No significant differences in patient demographics and baseline characteristics were observed between cohorts (Table 1). The distribution of patient sex across cohorts was similar, with 48 females in the robotic arm and 53 in the freehand group. Mean age and BMI were 60.4±13.5 years and 35.3±28.5 kg/m2 in the robotic group and 58.9±14.3 years and 30.0±8.1 kg/m2 in the freehand group (p=0.47 and p=0.08, respectively).
| - | Robotic Arm | Freehand Arm | - |
|---|---|---|---|
| # of patients | 99 | 99 | p |
| % Females | 48% | 53% | 0.57 |
| Age | 60.4±13.5 | 58.9±14.3 | 0.47 |
| BMI | 35.3±28.5 | 30.0±8.1 | 0.08 |
| Duration of surgery (mins) | 127.5 | 118.9 | 0.32 |
| Avg # screws | 5.8 | 6 | 0.55 |
| Avg blood loss (mL) | 72.4 | 88.4 | 0.17 |
| ALOS (days) | 2.1 | 2.4 | 0.20 |
| Follow up period (months) | 9.2 ± 4 | 10.5 ± 3 | 0.008 |
| Revisions | 1* | 0 | 1.00 |
A total of 572 screws (mean 5.8 screws per patient) were inserted in the lumbar spine under robotic guidance and 593 screws (mean 6.0 screws per patient) were inserted freehand. There were no registration failures or aborted cases in the robotic group. Mean surgery time was 127.5±57.5 min with an estimated blood loss (EBL) of 72.4±57.2 mL in the robotic arm and 118.9±62.8 min and 88.4±74.5 mL, respectively, in the freehand cohort (p=0.32 and p=0.12, respectively). Hospitalization length averaged 2.1±1.2 days and 2.4±1.4 days in the robotic and freehand cohorts, respectively.
Postoperative CTs were available for 52 patients (293 screws) in the robotic arm and 70 patients (421 screws) in the freehand arm (Table 2). All screws (100%) in the robotic arm were within the safe zone, i.e., fully within the pedicle or breaching less than 2 mm, while 2.6% (11 screws) placed in fluoroscopy-guided freehand procedures deviated from the safe zone (p=0.004), ten (2.4%) of which were grade C and one (0.2%) was a grade E breach.
| - | Robotic – 293 Screws | Freehand – 421 Screws | - | ||
|---|---|---|---|---|---|
| Gertzbein Robbins | Screws | % | Screws | % | P |
| A | 285 | 97.3% | 388 | 92.2% | 0.009 |
| B | 8 | 2.7% | 22 | 5.2% | - |
| A+B | 293 | 100.0% | 410 | 97.4% | 0.004 |
| C | 0 | 0.0% | 10 | 2.4% | - |
| D | 0 | 0.0% | 0 | 0.0% | - |
| E | 0 | 0.0% | 1 | 0.2% | - |
| C+D+E | 0 | 0.0% | 11 | 2.6% | 0.004 |
Average follow-up duration was 9.2±4 months in the robotic arm and 10.5 ± 3 months in the freehand arm (p=0.008). During this time, Oswestry Disability Index (ODI) was assessed in approximately 50% of the patient population, typically within six weeks of surgery. ODIs were similar between treatment groups, with a mean score of 10.5 following robotic surgery and 11.7 after freehand procedures (p=0.45). The grade E breach was asymptomatic throughout the 12-month follow-up period and did not require revision surgery. A single revision surgery was required in the robotic group within one week of surgery, due to a superficial wound infection (quill suture broke). The wound was washed out and closed, and the hardware was not removed or replaced. No other complications or revisions were recorded in either group.
4. DISCUSSION
Without a direct line of sight to the anatomical landmarks, surgeons attempting percutaneous insertion of pedicle screws depend on either imaging systems or computer guidance to accurately instrument the spine. This work compared pedicle screw placement accuracy following robotic-guided versus image-guided percutaneous pedicle screw instrumentation procedures. There were no pedicular breaches of 2 mm or more in the robotic arm, which is attributed to the detailed planning stage and precise intraoperative mechanical guidance. This is a significant achievement, particularly when compared to reports in the literature of open procedures benefiting from the full visibility of the anatomical landmarks [4, 5]. Similar degrees of accuracy, ranging between 98.5-100%, have been previously reported for the same robot platform [7, 12, 14, 22, 23] (Table 3), demonstrating a weighted-average of 99.3% accuracy of pedicle screw placement with the Renaissance guidance system. In the first report in the literature on the use of this system, Hu et al. presented findings from a consecutive series of 95 multilevel robotic-guided spine surgeries (960 screws), among which, 24 patients (25.3%) were operated using an MIS or hybrid open-MIS approach [7]. They highlight a 98.9% accuracy rate, where only a single screw had to be revised due to misplacement-associated radiculopathy. Onen et al. reported a mean accuracy of 98.5% in 27 surgeries (136 screws), of which 11 (40.8%) were performed using a percutaneous approach [14]. When assessing the radiation doses in the first 13 cases versus the next 14 cases, the authors found a 50% reduction in radiation exposure per screw, from 1.8 seconds to 0.9 sec per screw, in the latter group (p<0.05). In a randomized, controlled trial conducted by Kim et al., 99.4% accuracy was achieved in both the MIS robotic guidance arm and in the freehand open approach, yet the single revision of a breaching screw was in the freehand arm [22]. Another randomized, controlled trial found 100% accuracy [23], while a cadaveric study, which tested all four available Renaissance mounting platforms, achieved 100% accuracy in the 216 attempted trajectories from T1 to S1 vertebras [12].
| Author | Year | Study Type | Number of Screws | Screws in Safe Zone* |
|---|---|---|---|---|
| Hu | 2013 | Retrospective | 960 | 98.9% |
| Onen | 2014 | Prospective | 136 | 98.5% |
| Kim | 2016 | RCT** | 158 | 99.4% |
| Hyun | 2016 | RCT** | 130 | 100% |
| Fujishiro | 2015 | Cadaveric study | 216 | 100% |
| Zahrawi | Current | Retrospective | 293 | 100% |
| Weighted average | 99.3% | |||
Reports of accuracy achieved with the SpineAssist system (the previous generation of the Renaissance), have been less consistent. The majority of the works have been summarized by Onen et al. [14], however, several new studies have been published since. A recent two-surgeon retrospective SpineAssist study reported 98.5% accuracy of percutaneously placed pedicle screws [15]. In their analysis of the performance of 13 surgeons using the SpineAssist robotic platform during spine surgeries, Schatlo et al. report of a mean accuracy rate of 96.2%, with a peak number of misplacements occurring during cases 16-20. They ascribe this transient increase to the more lenient supervision and increased surgeon confidence during this skill-building period. This contrasts with the results presented by Hu et al., Van Dijk et al. and the current study, where no learning curve was observed, and high placement accuracy was obtained from the very first cases. Of note, however, these were single-surgeon studies or 2-surgeons in the case of Van Dijk et al., and all experienced surgeons, compared to the 13 surgeons in the paper by Schatlo et al., many of whom were surgical residents.
Two studies have reported inferior screw instrumentation accuracy with SpineAssist compared to freehand surgeries. Ringel et al. [16] reported 85% accuracy in the MIS SpineAssist-guided arm compared to 93% accuracy in the open approach freehand control arm. They attributed the results primarily to the type of mounting platform they used to attach the robot to the patient’s spine, and to skiving, or skidding of the surgical tools off of concave or convex surfaces, mainly laterally from the facet joint. Several recent studies using the same mounting platform did not encounter inaccuracy [10, 12, 15] and demonstrate the ability to avoid skiving. This is achieved either by: 1) avoiding during the planning phase screw entry points on uneven bony structures, such as by adopting a convergent screw trajectory; or 2) by preparing the anatomy to create a relatively flat surface for docking the tools properly. The former engages the bone on a flatter surface, while the latter relies on proper surgical technique which involves dissecting the soft tissues along the specified trajectory, and preparing the landing area for the robot’s cannula on the bone [10, 12]. Ringel et al. [16] also note the limited view of the iliac crest during the planning, which has since been resolved in the newer Renaissance system software. The considerably low screw placement accuracy reported for both the robotic and conventional fluoroscopy arms in a small-scale, prospective comparative study, claimed inferior results for the robotic arm (79%) [17], which may have been influenced by the small 64-screws sample size, extent of surgeon experience with the system and the reliability of the Rampersaud assessment scale.
The present comparative analysis demonstrated a modest, yet significant, improvement in percutaneous pedicle screw positioning accuracy when implementing robotic guidance. Screw accuracy correlates but is not synonymous with clinical outcomes or adverse events. In a comparative analysis of 1,056 screws, of which about half were placed in a percutaneous approach with fluoroscopy guidance, Oh et al. demonstrated that the greater the severity of breaching, the higher the incidence of suffering from a new neural deficit. This may also be affected by the shortcomings of most screw position grading systems that fail to account for breach directionality, which is cardinal in predicting clinical sequelae. More specifically, breaches in the medial and inferior walls, proximal to neural structures, can present a significantly greater threat than a similar grade lateral breach. Although lateral or superior deviations can compromise the biomechanical qualities of the instrumentation, medial and inferior breaches are more likely to induce long-term and irreversible neurological deficit. In their analysis of 62 robotic-assisted pedicle screw instrumentation procedures, Roser et al. [9] report a two-fold higher incidence of lateral (5.3%) versus medial (2.5%) deviations in their early experiences with the SpineAssist. In keeping with this report, both Ringel et al. [16] and Schatlo et al. [18] observed a higher incidence of lateral versus medial misplacements in the robotic arm, which can be minimized by both performing solid docking on a bony structure and by implementing counter-skiving measures [10, 12, 19]. The screw positioning accuracy obtained in the robotic group presented in this work was secured by the detailed planning of the trajectories and their docking surface on the bone, coupled with precise mechanical guidance to the planned entry points. Thus, the modest improvement in accuracy rates when compared to the freehand cohort can be of marked short-term and long-term clinical significance.
CONCLUSION
The present study, although controlled, was limited in it being a retrospective, single-surgeon series. Moreover, while the follow-up duration was significantly longer for the freehand arm, the additional four weeks of data were not projected to have influenced complication or revision rates.
The current study corroborates the growing evidence that guidance of pedicle screw insertions by the Renaissance robot is capable of increasing pedicle screw implantation accuracy, and thus may reduce the rate of instrumentation-related complications. As an enabler of MIS surgeries, this robotic system bears the potential to also reduce surgical and medical complications associated with this approach. Therefore, future studies should place more focus on establishing its clinical advantage (e.g., clinical complication and revision rates) rather than its technical capabilities (e.g., accuracy).
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
No animals/humans were used for studies that are the basis of this research.
CONSENT FOR PUBLICATION
Not applicable.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGMENTS
The primary author (FZ) is a consultant and owns stock of Mazor Robotics, the manufacturer of Renaissance Guidance System. The other authors have no personal financial or institutional interests in any of the drugs, materials, or devices described in this article.


