All published articles of this journal are available on ScienceDirect.
Role of Biplane Double Supported Screw Fixation For Fracture Neck Femur In Elderly Population: A Prospective Study
Abstract
Introduction:
The treatment of fracture neck femur varies according to the age of patient, the displacement of fracture fragments and the duration of the fracture. Various treatment options available for elderly are screw fixation, hemiarthroplasty and total hip arthroplasty.
Materials and Methods:
This is a prospective study done at authors institutes between January 2014- December 2016. 30 patients aged more than 50 years who sustained fracture neck femur were included in the study. 3 patients were lost to follow up and 2 patients died due to medical comorbidities. Out of the 25 remaining patients, 17 were males and 8 were females and they were operated by the biplane double supported screw fixation method (BDSF TECHNIQUE) and were followed up for a period of two years. The final Harris Hip Score at the last follow up was calculated.
Results:
Out of the 25 patients, the union was achieved in all the patients. The mean duration of union was 10 weeks. 1 patient had progressive femoral head resorption due to chondrolysis resulting in antalgic gait and unbearable pain and underwent total hip arthroplasty. The mean harris hip score was 81.2
Conclusion:
In elderly patients with osteoporosis and in those patients who can not afford arthroplasty or in those patients where arthroplasty is contraindicated, BDSF method is an alternate method for fixing fracture neck femur.
1. INTRODUCTION
Fracture of neck femur is a very common injury in patients more than 50 years of age. According to the present scenario, arthroplasty should be reserved for patients more than 80 years, while in patients age less than 60 sustaining fracture neck femur, joint salvage must be attempted while the ideal treatment of fracture neck femur in the age group 60-80 is still a matter of debate [1].
A number of controversies exist in relation to the cannulated screw fixation for fracture neck femur like number of screws to be used, position of screws in the head and neck and the configuration of screws to be used. A number of biomechanical studies have been done in relation to the ideal screw configuration [2-9].
While some authors have suggested central screw placement [10], others have suggested peripheral screw placement [3, 5, 11]. Some authors believe that the screws should be placed parallel to each other [3, 4, 11-13], while others believe that screws should be divergent in lateral view [9, 14, 15].
The most commonly used methods by surgeons worldwide to fix fracture neck femur is three parallel screws inserted in inverted triangle configuration [16, 17]. Since the screws are inserted close to each other with entry points near the thin cortex at the base of greater trochanter, they may not be able to withstand anteroposterior bending and varus stresses especially in osteoporotic patients.
To overcome this problem of osteoporosis and for those patients in which arthroplasty is contraindicated, Filipov [18] devised a method of Biplane Double Supported Screw Fixation (BDSF) in which the two screws are laid in two planes, which makes it possible for the entry points of middle and distal screws to be placed in distal solid cortex of proximal diaphysis, the distal screw is placed in the dorsal oblique plane while the middle and proximal screws are inserted in ventral oblique plane. BDSF method uses two calcar buttressed screws: The position achieved by the distal as well as the middle screw, in view of statics, turns them into a simple beam with an overhanging end, loaded with a vertical force. This beam with an overhanging end successfully supports the head fragment, bearing the body weight and transferring it to the diaphysis [19].
2. MATERIALS AND METHODS
After obtaining proper clearance from the ethical committee, thirty patients presenting with fracture neck femur aged more than 50 years at authors institute between January 2014-December 2016 were included in the study. Inclusion criteria were poor socioeconomic status leading to non-affordability for arthroplasty, patients with mental illnesses like dementia, patients having risk cardiopulmonary status which places them at an extra risk for a longer surgery like arthroplasty and patients with severe osteoporosis. Patients with injury more than twenty-one days old were not included in the study. Three patients were lost to follow up while two patients died due to the associated comorbidities. The remaining twenty-five patients, out of which seventeen were males and eight were females, were followed up for a period of two years and the final Harris hip score was recorded.
3. SURGICAL TECHNIQUE
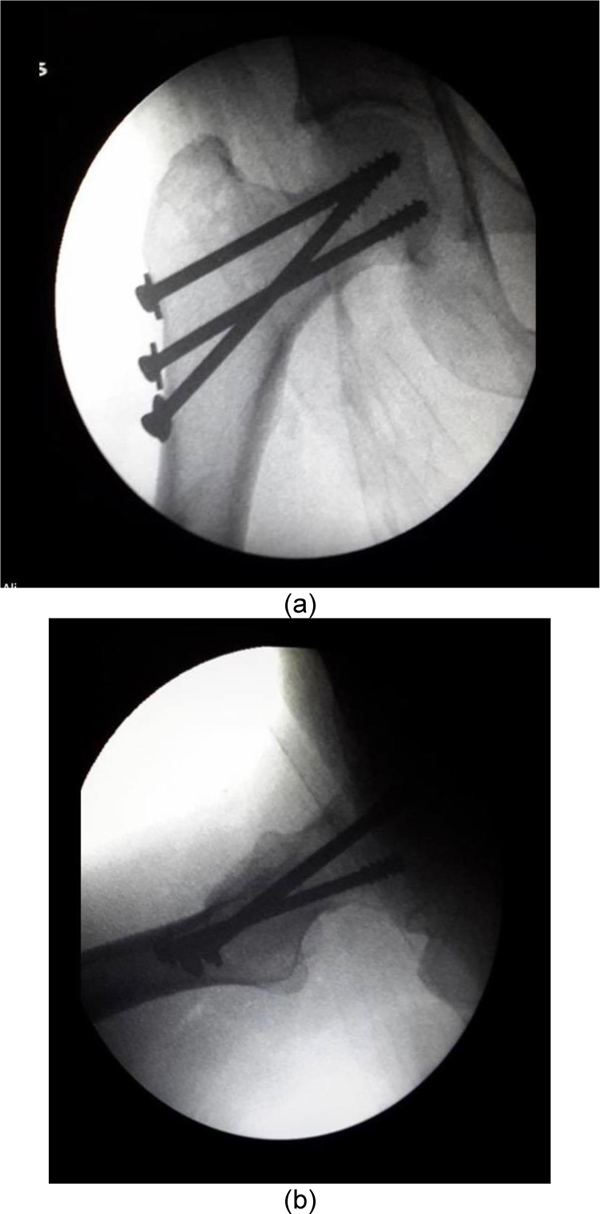
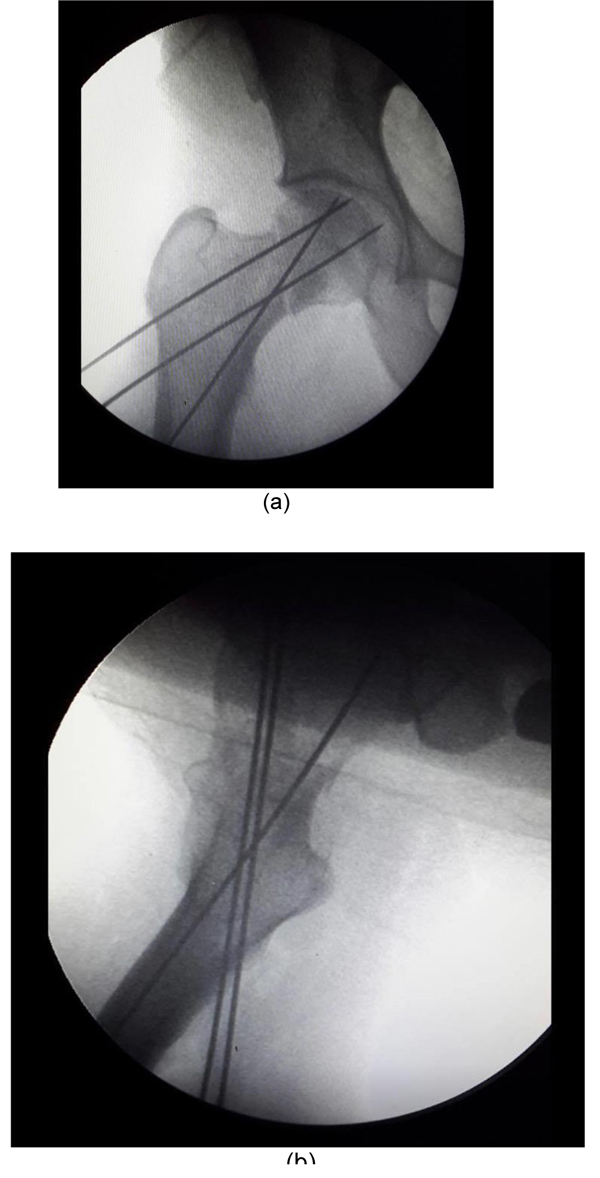
After getting proper consent and pre-anesthetic clearance, the patients are put supine on traction table and reduction is done by traction, internal rotation and slight abduction of the limb as shown in Figs. (1a, b, c). A straight incision starting at the base of greater trochanter is made with a length of approximately 7-8 cm with BDSF method, three cannulated screws are put in two different planes in the lateral view. The distal screw is placed in the dorsal oblique plane while the middle and proximal screws are placed in the ventral oblique plane as shown in Figs. (2a and b)

The first step is to put guide wire for the distal cannulated screw. Its tip is placed 5-7 cm distally from the base of the greater trochanter in the anterior one-third of the surface of the femoral diaphysis. It is directed proximally at an angle of 150-165o, with inclination from anteriorly–distally to posteriorly–proximally, so that after it touches on the curve of the distal femoral neck cortex, the wire goes into the posterior half of the femoral head as shown in Fig. (3).

The middle guide wire is placed next. The entry point is at 2-4 cm proximally from the entry point of the distal wire, in the posterior one-third of femoral shaft. This wire is placed at an angle of 135-140o and inclined from posteriorly-distally to anteriorly-proximally, so that after it touches the curve of the distal femoral neck cortex, the wire goes into the anterior one-third of the femoral head in the lateral view and in A-P view, the guidewire rests in distal one third of femoral head.
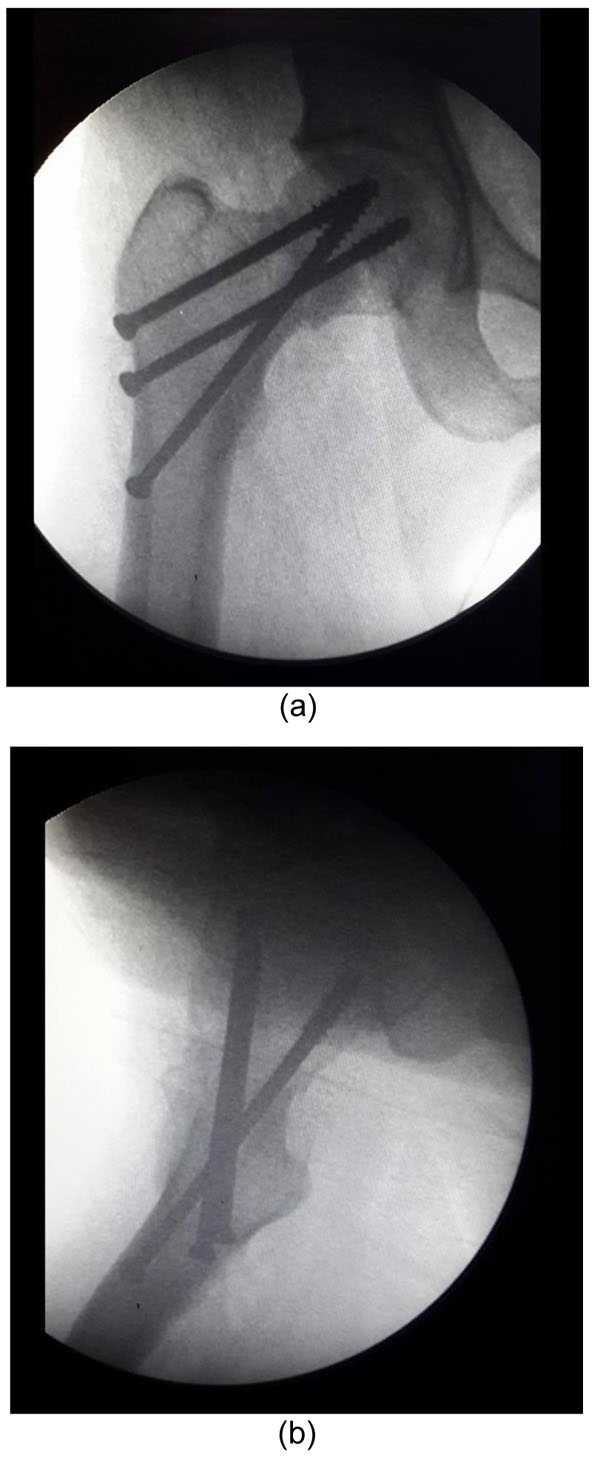
The proximal guidewire is laid in the last. The entry point is 1-2 cm proximally from the entry point of middle wire in the posterior one-third of femoral shaft. It is placed parallel to the middle wire and is directed posterior-distally to anterior proximally so that in the A-P view, the guidewire lies in proximal one-third of femoral head and in the lateral view, it lies in anterior one-third of femoral head as shown in Figs. (4a and b)
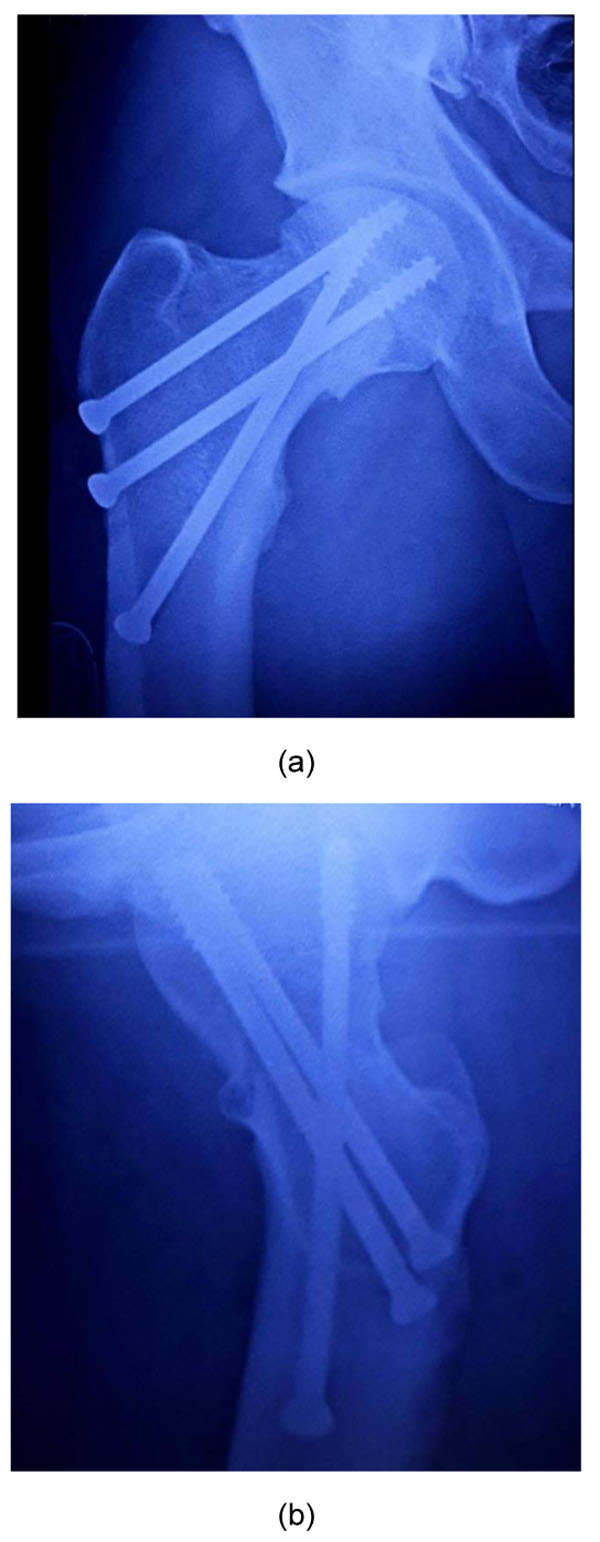
Being perpendicular to fracture surface, the middle and proximal screws are placed first followed by insertion of the distal screw as shown in Figs. (5a and b).
4. POSTOPERATIVE PROTOCOL
Postoperative radiographs were obtained on the first postoperative day. The patient was encouraged to do static quadriceps and active assisted/active Straight Leg Raising (SLR) exercises once the patient feels comfortable. The patient was made to sit up on the bedside and non-weightbearing walking was started 24 hours after the surgery.
Patients were discharged from hospital 48 to 72 hours after surgery. All the patients were followed up clinically and radiologically after three weeks, six weeks, three months, six months, twelve months and after two years. Partial weight bearing was allowed after three weeks and full weight bearing was allowed after the radiographic union was evident. Radiologically fracture union was defined as continuity of at least three cortices in AP and lateral views without any fracture gap. Clinically fracture was considered as healed when there was no local tenderness and patient could do full weightbearing without any support. Stair climbing and hip abductor strengthening exercises were gradually initiated after 6 weeks.
Once the fracture was healed, patients were encouraged to sit on the floor cross-legged and to do squatting as it is an essential part of the routine in Indian population
5. RESULTS
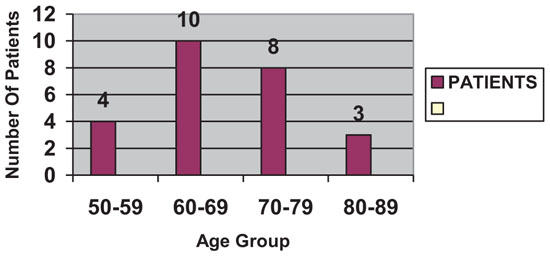
Out of the 25 patients, 17 were males (68%) and 8 (32%) were females. The average age was 67.8 years. The youngest patients were aged 52 years while eldest being 88 years. Majority of the patient i.e 18 out of 25 patient belong to 60-80 years of age group details of which were shown in Bar Chart.
Out of the 25 patients, 2 (8%) were Garden type 1, 3 (12%) were Garden type 2, 6 (24%) were Garden type 3 and 14 (56%) were Garden type 4.
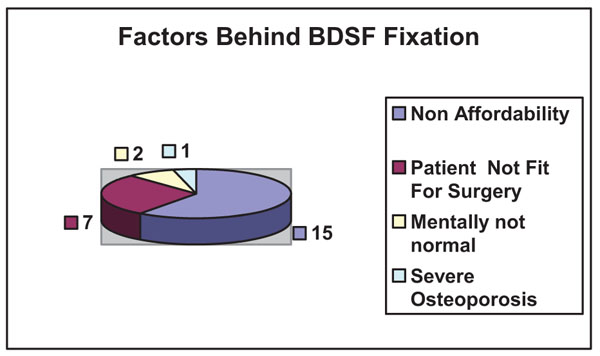
A most common factor behind the BDSF was non-affordability of the patient to arthroplasty followed by patients unfit for surgery as shown in Pie Chart.
The mean HARRIS HIP score was 81.2. Out of the 25 patients, 3 (8.57%) had poor HHS, 4 (11.42%) had fair HHS, 9 (28.57%) had good HHS, while excellent HHS was seen in 9 (51.42%) patients.
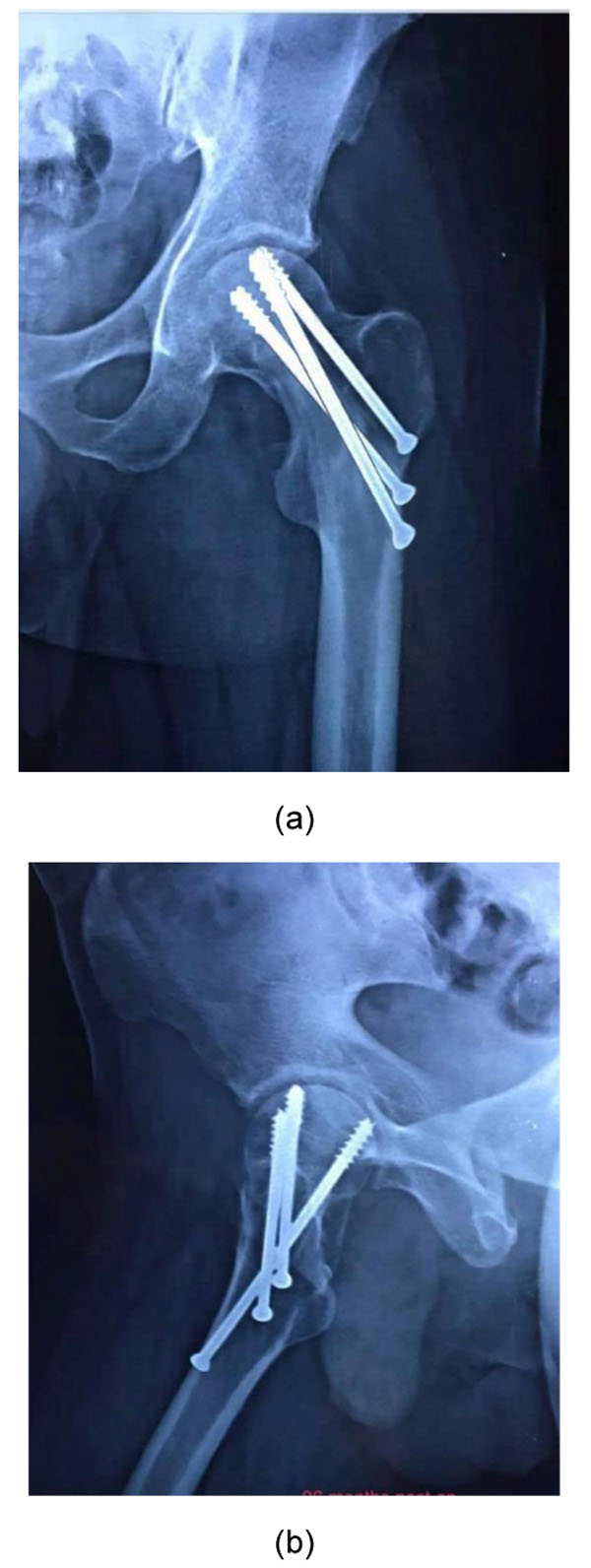
All the fractures united uneventfully as shown in Figs. (6a and b, 7a and b). The mean duration of union was 10 weeks. One patient had femoral head resorption due to the chondrolysis and required a total hip arthroplasty. None of the cases had an implant failure.
6. DISCUSSION
There seems to be a lot of controversy regarding the cannulated screw fixation for fracture neck femur like the number of screws to be used, configuration of screws and their position in head and neck. The method most widely practiced by surgeons for fixing the fracture neck femur is by three cancellous screws placed parallel to each other and various authors have reported the failure rate to be as high as 20-42% [20-24]. This failure can be accounted for many factors. One of the factors is that the entry point of the screws lies in the thin and fragile cortex of greater trochanter or near to it and such a mechanical construct relies on inter-fragmentary compression achieved intra-operatively for its success but the amount of interfragmentary compression achieved depends on how much solid the cancellous bone is. So this accounts for high failure rate in osteoporosis [18].
Biplane Double Supported Screw Fixation method [18] (BDSF) overcomes these problems and has various unique advantages and the results of our study prove it to be a useful method particularly in relevance to the Indian population.
The position of the distal screw as well as the middle screw achieved by the method, in terms of statics, turns them into a simple beam with an overhanging end, loaded with a vertical force. This beam with an overhanging end successfully supports the head fragment bearing the body weight and transferring it to the diaphysis. Moreover, due to the biplane placement, enough space for a third screw is provided, whereas in the conventional methods for fixing neck femur, only one or a maximum of two screws can be placed at an obtuse angle [25, 26]. Another advantage of the method is that due to the increase in the distance between the two supporting points, the weight borne by the bone is reduced. Since the entry points of the screws are positioned wide apart from each other, which ensures that when weightbearing, the tensile forces are spread over a greater surface of the lateral cortex and thus the risk of its fracturing decreases significantly. Since the distal screw touches the posterior cortex and also being placed at an obtuse angle, it provides improved strength of fixation at the anteroposterior bending of neck (when arising from a chair) and this has been confirmed biomechanically [27].
Since ours is a government tertiary care referral centre, majority of our patients do not have insurance coverage and have to spend on their own, so for those patients who can not afford arthroplasty, BDSF method can be picked as the first choice in the selected age group since the cost of screw fixation is remarkably less as compared to arthroplasty. Majority of our operated cases came from rural background who require sitting cross-legged and squatting for their daily activities and despite being told not to do such activities, these patients at follow up were found to be very comfortable in doing such activities, while in case of arthroplasty, prolonged supervision is required.
BDSF method has several advantages such as small learning curve, cost-effectiveness, short operative time and it requires normal theatre set up but the only critical point is the perfect positioning of the guide wires which initially may seem difficult but with strict adherence to principles this can be mastered in no time.
The strength of our study is that it is a prospective study with adequate follow up while the weakness is that the sample size is small.
CONCLUSION
BDSF method was devised mainly to address that group of patients who have contraindications for arthroplasty and we have found this as an excellent method in terms of fracture consolidation and functional outcome. This construct provides the solid stability required for endosteal healing of these fractures and we found it very suitable for Indian patients whose daily activities require sitting cross-legged as well as squatting. We, therefore, recommend that this method of fixation must be attempted in selected cases of fracture neck femur in the older population.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
No animals/humans were used for studies that are the basis of this research.
CONSENT FOR PUBLICATION
Patient consent was taken from the patient prior to the publication of this article.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


