All published articles of this journal are available on ScienceDirect.
Does Scapular Motion Regress with Aging and is It Restricted in Patients with Idiopathic Frozen Shoulder?
Abstract
Purposes:
It has been reported that the amount of posterior tilt and upward rotation in scapular motions decreases with aging. The purposes of the current study were to investigate age related scapular motion regression and scapular restriction in patients with idiopathic frozen shoulder (IFS).
Methods:
The groups were recruited as follows: two groups of 50 asymptomatic subjects aged in their twenties and fifties, and 56 patients with IFS. We passively moved the scapula toward 8 directions: elevation/depression; upward/downward rotation; external/internal rotation; and anterior/posterior tilt. The grading of scapular motion was ranged from 0 to 3 (3, normal; and 0, severe restriction) and the score for each direction and the total aggregated score for all directions were calculated.
Results:
Scapular restriction was present in 3 subjects (6%) in the normal 20s group, 10 (14%) in the 50s group, and 51 (91%) in the IFS group. The total score between the normal 20s and 50s groups did not show statistical difference; however, greater significance was present between the normal 50s group and the IFS group (p < 0.01). There was statistical significance in depression (p < 0.01), downward rotation (p < 0.01), and posterior tilt (p < 0.01) among the 3 groups.
Conclusion:
Depression, downward rotation, and posterior tilt substantially regress with aging. Scapular motions towards depression, downward rotation, external rotation, and posterior tilt are severely restricted in the IFS group.
INTRODUCTION
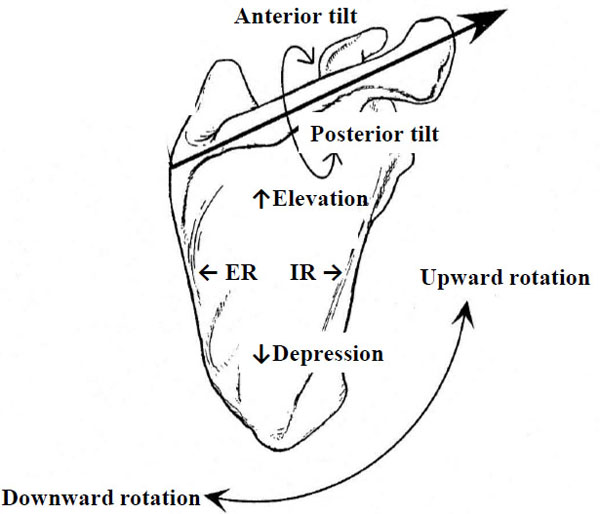
Proper control of the scapular position is an essential component for the functions of the shoulder joint, providing precise reach motion of the upper limb to a target in a grasping or pointing action. The scapula moves towards 8 directions: elevation and depression; upward and downward rotation; anterior and posterior tilt; and internal and external rotation [1-6]. The motion of the scapula is a combination of these directions, for example, which simultaneously translates towards elevation, upward rotation, posterior tilt, and internal rotation during arm elevation [4, 6]. As an individual ages, alterations of the scapular kinematics during shoulder elevation has been well documented. Children show greater scapular upward rotation than that of adults, and conversely the angles of both upward rotation and posterior tilt decrease with aging [1, 7]. Endo et al. reported that scapular upward rotation and posterior tilt decreased with aging due to thoracic kyphosis and suggested that the regressions may lead to shoulder pathologies [7].
Scapular dyskinesis, winging, and alterations of scapular kinematics have been described as dysfunctions of the scapula [8-11]. An increase in upward rotation is revealed in patients with shoulder pathologies who are over 50 years of age [12-14]. The prevalence of idiopathic frozen shoulder (IFS), the etiology has not been determined with any certainty, is especially higher in the population aged over 50 years old. Patients with IFS have shown to display increases in scapular upward rotation and on the contrary, decreases in posterior tilt in comparison with the non-affected shoulder [13, 15-18].
Changes in scapular kinematics, which are a decrease in upward rotation with aging and an increase of upward rotation in the shoulder pathologies, are conflicting reciprocally and have not been completely interpreted. Additionally, such alterations of scapular kinematics are not shown to be clinically relevant in the evaluation, treatment, and prognosis of the shoulder pathologies. The authors hypothesized that a decrease on scapular motion, i.e. scapular restriction progressed with aging and restriction of the scapular motion was severely associated with patients with IFS. The purposes of this study were to compare the magnitude of scapular motion between two groups of normal healthy subjects aged in their twenties (20s) and fifties (50s), and between the group of normal healthy subjects aged in their 50s and patients with IFS.
MATERIALS AND METHODS
Definition of Normal and Restricted Scapular Motion and Repeatability of the Scapular Examination
In order to preliminarily define normal scapular motion and restriction of the scapula, the authors randomly recruited 10 normal subjects, aged in their 20s and 70s and without prior shoulder pain and trauma, no history of throwing sports and; 10 patients with IFS who were diagnosed in our clinic. All recruits were examined by passively moving the scapula toward the eight established directions while the recruit was lying in the lateral decubitus position (Fig. 1a, b). After a comprehensive evaluation of each healthy subject, it was determined that normal scapular motion
moves freely and fully towards the eight directions; conversely, the scapula of patients with IFS displayed remarkably limited range of motion. Thus, the authors defined normal scapular motion as “no restriction with passive scapular motion (PSM)”. Mild restriction displayed slight restriction, although the restriction can be readily removed with the PSM maneuver. Moderate restriction showed greater restriction than mild restriction and some restriction remained after the PSM maneuver. Severe restriction was defined as almost no scapular motion. Thus, the grading of PSM ranged from 3 to 0 (3, normal; 2, mild restriction; 1, moderate restriction; and 0, severe restriction).
The repeatability of the PSM test in 20 healthy subjects and 10 patients with IFS was statistically investigated by the three authors using intra-class correlation coefficients (ICC). Intra-observer reliabilities ICC (1,1) indicated between 0.78 and 0.85 for movement in eight directions among 3 examiners, and ICC (1,2) ranged between 0.74 and 0.92. Inter-observer reliabilities ICC (2,3) showed 0.86 for scapular elevation; 0.82 for depression; 0.84 for upward rotation; 0.89 for downward rotation; 0.80 for external rotation; 0.75 for internal rotation; 0.71 for anterior tilt; and 0.79 for posterior tilt [19]. The PSM test, in which ICC (1,2) was higher than ICC (1,1), and ICC (2,3) was acceptable. Each patient should be examined twice by one examiner when using the PSM test in order to successfully evaluate scapular motion for a clinical assessment.
Participants and Patients with IFS
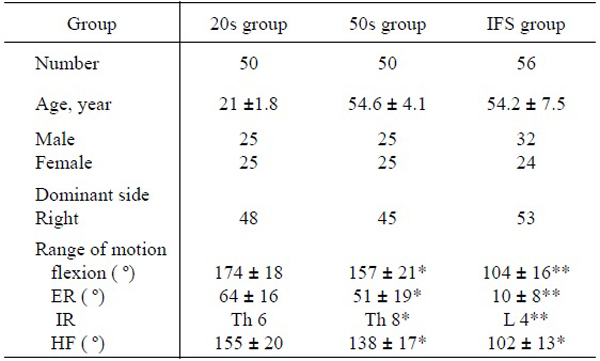
This study was approved by the Internal Review Board of our hospital (the approved number K22-04). Each subject and patient was informed of the details of the study and provided signed written consent before participation. The demographics of the 3 groups are summarized in Table 1.
Fifty healthy adults aged in their twenties (20s group) and fifties (50s group), who had no history of shoulder pain or trauma, and no participation in sport activity for two years prior to the study were enrolled in the study. Fifty-six patients who were diagnosed with the frozen phase of IFS affecting the dominant shoulder participated in the study. The patients had no trauma, no medical disorders such as diabetic mellitus and hyperthyroidism, showed normal X rays, and range of motion (ROM) revealing less than 120 degrees of flexion and less than one third of the range of external rotation against the unimpaired shoulder joints, and under the 1st lumbar spine level in internal rotation [20, 21]. The exclusion criteria were history of shoulder trauma or surgery, chronic arthritis, and neurological deficits such as stroke, myelopathy, cervical radiculopathy, and peripheral nerve palsy around the shoulder joint.
Procedures
The examiner (K. E.) assessed each scapula of both the dominant and non-dominant shoulders twice in the two groups of the normal healthy subjects and the IFS groups with the PSM test. Two types of the grading score were recorded; the grading score for each direction of the scapula, and the aggregate scores as the total PSM score for each group. Additionally, active ROMs of the dominant shoulder joint, such as, flexion, external rotation, internal rotation (hand behind back), and horizontal flexion were measured with a goniometer.
Numbers of restriction of scapular motion toward each direction in demographics of three groups.
 |
Data Analysis
All statistical analyses were conducted using the SPSS software package (version 21.0; SPSS, Chicago, USA) with a significance of α= 0.05. The Shapiro-Wilk test revealed that the data did not follow a normal distribution and so non-parametric statistical analyses were used. Analyses of correlations between outcome measures of the 8 scapular directions and total score in 56 affected shoulders were carried out with the Spearman’s rank correlation coefficient. The Kruskal-Wallis test was performed in order to compare the total grading scores among the three groups. Furthermore, the Mann-Whitney test was also used to compare between the total grading scores of the three groups. Each grading score in the 8 scapular directions was analyzed with the Mann-Whitney test and Bonferroni correction (α= 0.05/3). The Kruskal-Wallis test was used to compare the number of participants, age, sex, dominant side, ROMs of the shoulder joint in the three groups.
RESULTS
There were no significant differences in the number of subjects, gender, and the dominant arm except age and ROMs among the three groups. Each ROM of the shoulder joint in the normal healthy 20s group was statistically greater than those in the normal healthy 50s group (p < 0.05), and there were also significant differences in ROMs between the normal healthy 50s and the IFS group (p < 0.01) (Table 1).
Total Score of the PSM Test in the Three Groups
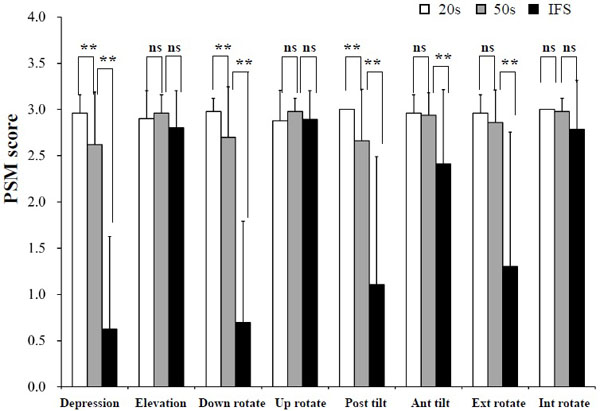
No statistical differences were found among 8 directions of scapular motion in the dominant and non-dominant arms in the 20s and the 50s groups (p > 0.07). Fig. (2) showed the total score of PSM for the three groups. Both Kruskal-Wallis and Mann-Whitney tests showed no statistical difference between the normal healthy 20s group and the 50s group, but there were statistical differences in the mean total score between the normal healthy 50s group and the IFS group (p < 0.05).
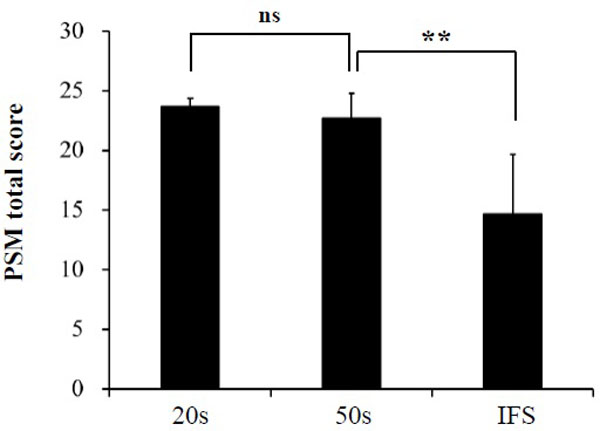
Total score of passive scapular motion in three groups.
The mean total score was 23.6 ± 0.7, 22.7 ± 2.1, 14.6 ± 5.1 in the normal twenties group, normal fifties group, and idiopathic frozen shoulder groups, respectively.
20s, normal twenties; 50s, normal fifties; IFS, idiopathic frozen shoulder; ns; no significance; ** p < 0.01.
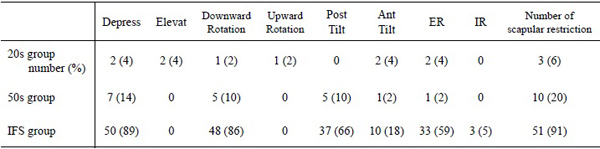
Each Score of Each Direction and the Number of Restricted Scapula in the Three Groups
The numbers of restricted scapula in the three groups are summarized in Table 2. From the PSM test, scapular restriction was found to be present in only three subjects (6%) in the 20s normal healthy group, 10 (14%) in the normal healthy 50s group, and 51 (91%) in the IFS group. The PSM grading scores for each scapular direction from the three groups are shown in Fig. (3). There were significant differences in depression (p < 0.01), downward rotation (p < 0.01) and posterior tilt (p < 0.01) between the three groups, and greater significances in restriction towards the three direction (p < 0.05) were also present between the normal healthy 20s and the 50s groups. Statistical differences between the normal healthy 50s group and the IFS group were identified in depression (p < 0.01), downward rotation (P < 0.01), posterior tilt (p < 0.01), anterior tilt (p < 0.05), and external rotation (p < 0.01).
Numbers of restriction of scapular motion toward each direction in three groups.
 |
Each score of passive scapular motion grading score to each direction in 3 groups.
20s, normal twenties; 50s, normal fifties; IFS, idiopathic frozen shoulder; Down rotate, Downward rotation; Up rotate, Upward rotation; Post tilt, Posterior tilt; Ant tilt, Anterior tilt; Ext rotate, External rotation; Int rotate, Internal rotation; ns, no significance; * p < 0.05; ** p < 0.01.
Correlation Coefficient in Each Score and Total Score of Scapular Motion
The correlation coefficient of each scapular restriction, calculated using the Spearman’s rank test, is shown in Table 3. Correlation coefficient values (CCV) for restriction of depression (0.941), for downward rotation (0.879), for posterior tilt (0.804), and for that of external rotation (0.733) were significantly correlated with the total score (Table 3). Restriction of depression greatly showed mutual correlation between those of downward rotation (CCV = 0.914) and posterior tilt (CCV = 0.748).
Correlation coefficient and p value in each direction of scapular restriction.
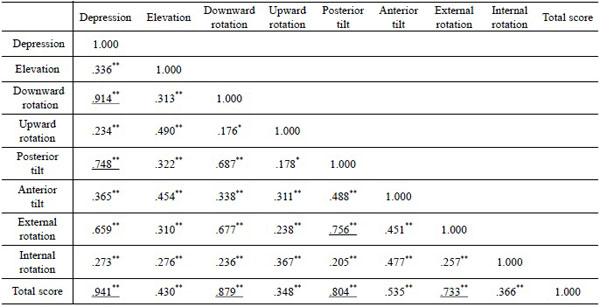 |
*, P < 0.05; **, p < 0.01 ; under line means correlation coefficient value more than 0.7.
DISCUSSION
The most important findings of the present study are firstly that depression, downward rotation, and posterior tilt in the normal healthy 50s group significantly decrease compared to those of the normal healthy 20s group. The result validates that the amount of scapular motion reduces with aging. The regression of scapular motion conceivably corresponds with less ROMs of the shoulder joint in the normal healthy 50s group. The age-related regression of scapular motion may be due to poor posture, periscapular muscles weakness, and/or restraint of rib motion. Poor postures, including thoracic kyphosis, forward head position, and slouched trunk postures have been directly linked to alterations in the scapular kinematics and regress the amount of thoracic motion and shoulder joint movement [3, 7, 22-24]. Kyphosis of the thoracic spine eventually translates the scapula toward elevation, upwards rotation, anterior tilt, and internal rotation. Such positional alterations of the scapula with aging may provide less scapular motion toward depression, downward rotation, and posterior tilt. However, as thoracic kyphosis is not so common in the fifties subjects in this study another factor that restrains rib motion and leads to restriction of the scapula appears to be present. As the scapula is depressed inferiorly, the trunk bends laterally and the rib bones move closer to each other reducing the space between them. Scapular depression and downward rotation reciprocally correlates with rib depression toward the inferior direction, thus posterior tilt of the scapular synchronizes with elevation, posterior rotation, and the retraction of the ribs [25]. Further study is necessary to clarify the interplay between scapular motion and rib movement.
The second findings are that depression, downward rotation, anterior and posterior tilts, and external rotation severely are restricted in the IFS group in comparison to those of the normal healthy 50s group. Pathophysiology of IFS has generally been understood as adhesive capsulitis [26], contracture of the coracohumeral ligament [27, 28], and abnormal scapular kinematics. Biomechanical investigators have described that there is a significant increase in scapular upward rotation on the affected side of patients with IFS when compared to the non-affected side [13, 15, 16-18, 29], and that the degree of anterior and posterior tilt did not show a significant difference between the non-affected and affected shoulders during flexion and abduction [15]. All of the patients within the IFS group, who complained of remarkably decreased shoulder ROMs and pain during motion, demonstrated severe restriction of depression, downward rotation, posterior tilt and external rotation. Tightened cuff muscles and periscapular muscles, adhesive capsulitis, and contracture of the coracohumeral ligament are assumed to comprehensively contribute to the development of scapular motion restriction. As reported in previous literature, anterior capsular tightness of the shoulder joint reduces posterior tilt and external rotation of the scapula [13].
If the rotator cuff muscles are tightened, the scapular motion should be restrained within a small amount of translation toward all directions, however our result indicates restriction toward 4 directions. Therefore the muscles are not the causative soft tissue source of scapular restriction in IFS. Tightness of the upper trapezius, the rhomboideus, and/or the superior capsule may cause scapular restriction toward depression and downward rotation. Restriction of external rotation appears to be due to tightness of the middle serratus anterior, the pectoralis major and/or the anterior capsule. Tightness of the lower serratus anterior, the pectoralis minor [30], the anterior capsule [13], the coracohumeral ligament may restrict scapular posterior tilt. In patients with IFS, after manipulation of the shoulder joint under brachial plexus block, moderate restoration of scapular restriction was achieved. Hence, tightness of the capsule appears to be substantially responsible for restriction of the scapula. Scapular motion showed normal at the final examination (data not shown).
Contracture of the sternoclavicular joint may empirically contribute to restriction of the scapula, because passive motion of the joint induces pain but the maneuver increases in the amount of scapular motion. Further studies are necessary to identify the causative soft tissues and /or joints of scapular restriction in the future.
The clinical implications of the study are shown as following. Physical exercises would stop or restore age-related progressive regression of scapular motion such as depression, downward rotation and posterior tilt. Furthermore, improvement of poor posture and the restoration of thoracic motion including the thoracic spine, clavicle, and ribs regain normal scapular function. Physical therapy treatments that aim to restore scapular motion are also crucial to patients with shoulder pathologies who have undergone arthroscopic surgery or have been treated conservatively. The PSM test reveals a three-fold clinical relevance: firstly, to clearly identify the extent in which scapular motion is restricted; secondly, the evaluation and treatment of the scapula can be conducted simultaneously; and finally that the derived score from the PSM test indicates a precise correlation with the severity of the condition in IFS.
The authors recognize that this study has some limitations. A potentially significant limitation is that the PSM test is a static manual examination and cannot exclude the motion of other joints such as the sternoclavicular joint and the acromioclavicular joint. For instance, posterior tilt is predominately in the acromioclavicular joint with a small contribution from the sternoclavicular joint [12]. The PSM does not only include the single motion of the scapular, but includes the motion of the glenohumeral joint and other joints described previously. Therefore, further and detailed study is necessary to determine whether the PSM test is consistent with dynamic scapular motion by conducting 3-dimensional dynamic scapular motion analysis in the future. A second limitation is that this study investigates restriction of the scapula in patients with IFS, which is just one of a number of shoulder pathologies. Alteration of scapular kinematics or scapular dyskinesis has also been recognized in impingement syndrome, rotator cuff tears, shoulder instability, other forms of stiff shoulder, and overhead sports’ injury. Further research should include these shoulder pathologies and their evaluation using the PSM test.
CONCLUSION
The scapular motions of depression, downward rotation, and posterior tilt reduce with aging and a restriction of these three movement patterns is also frequently associated with patients with IFS. Restriction of scapular motion increasing with aging may be one of the causative events that leads to shoulder joint pathologies in the over fifties population.
CONFLICT OF INTEREST
This research had no financial affiliation, including research funding, or any involvement with any commercial organization that has a financial interest in any matter included in this manuscript.
ACKNOWLEDGEMENTS
Declared none.